 Case Report
Case Report
Embolic Stroke from Aortic Valve Papillary Fibroelastoma an Unsuspected Finding
Jennane Ratiba*, Souilk Houda, Hilal Safae and Mesmoudi boutaina
Service of cardiology, Perpignan hospital, France
Jennane Ratiba, Service of cardiology, Perpignan hospital, France.
Received Date:August 22, 2022; Published Date:September 21, 2022
Summary
Background: Cardiac papillary fibroelastomas are considered the second most common benign primary cardiac tumor after myxoma.
Case summary: The clinical presentation of these tumours varies from asymptomatic to severe ischaemic or embolic complications. The patient presented with left hemiplegia and dysarthria, and as part of its etiological assessment a transesophageal ultrasound was performed objectifying papillary fibroelastoma of the aortic valve arising from the endocardium of the left coronary cusp. The diagnosis was clarified by the other imaging systems (scanner and magnetic resonance imaging). In front of the embolic episode and the size of the fibroelastoma, the patient was operated, and recovered well.
Conclusion: This case contributes to highlighting that cardiac papillary fibroelastomas are a rare but potentially significant cause of cardioembolic stroke. Urgent resection of the tumour is not only life saving but also avoids tumour related vascular, embolic or neurological complications.
Keywords:Cardiac papillary fibroelastoma; Stroke; Aortic valve
Introduction
Papillary fibroelastomas are small benign tumors that represent 10% of all cardiac tumors and measure 9–12 mm. Histologically, their constituting layers have a similarity to those of the chordaetendineae. They can develop on any endocardial surface, 90% of the cases are attached to the aortic valve [1]. Even though they are categorized as benign tumors and in the majority of cases they are asymptomatic. Those in the right-side of the heart can cause pulmonary embolism, while those in the left-side can cause serious complications, such as systemic embolic events, stroke and acute myocardial infarction.
Case Report
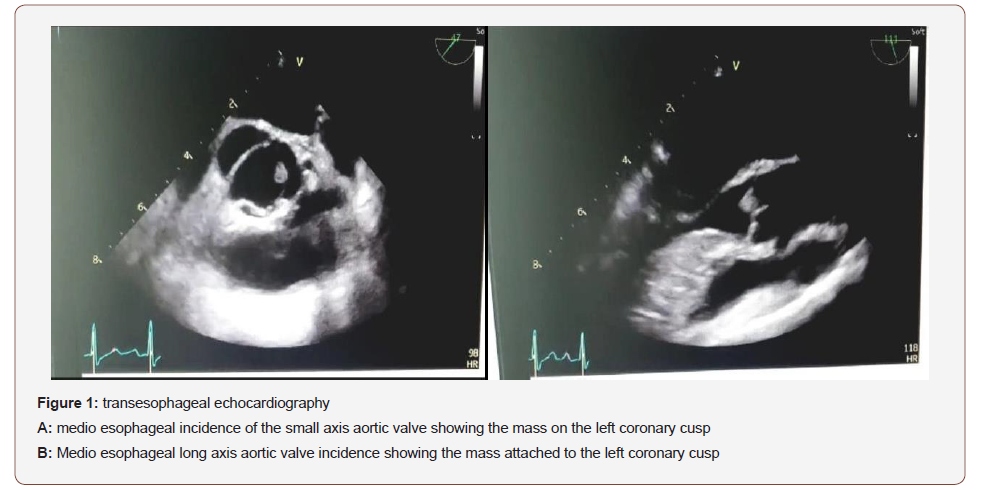
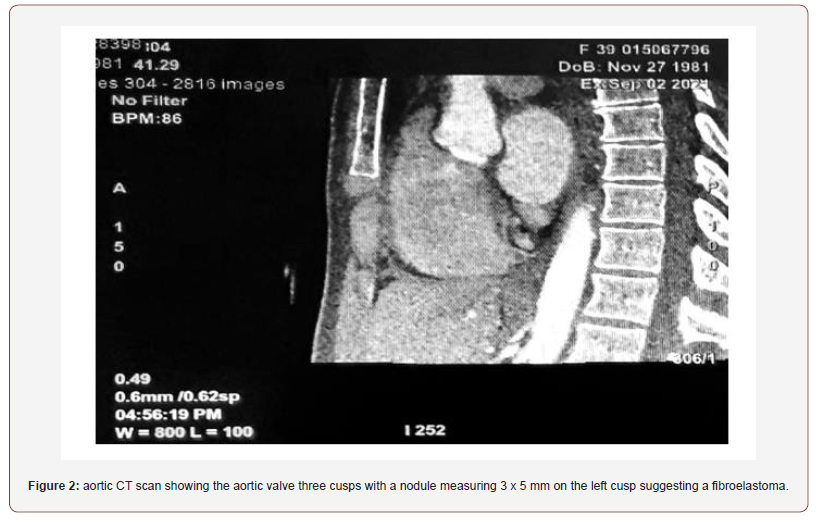
A 49 year old woman with no cardiovascular risk factors was admitted to the emergency department with left hemiplegia and dysarthria, without other symptoms. The patient was initially evaluated by a magnetic resonance imaging of the brain, who revealed subacute ischemic infarct. The patient was admitted to the neurology ward for further study. At admission, the patient was afebrile and hemodynamically stable. An electrocardiogram showed normal sinus rhythm and physical examination was unremarkable, except for a left side body paralysis. Blood tests were also normal. Supra-aortic trunks ultrasound presented no significant lesions. No arrhythmias were found on electrocardiographic monitoring. A transesophageal echocardiogram showed a small echodensity attached to the aortic valve arising from the endocardium of the left coronary cusp (Figure 1). The diagnosis was clarified by the other imaging systems scanner (Figure 2) and magnetic resonance imaging. No other source of the emboli was identified. Because of the acute phase of the stroke, anticoagulation was delayed. And the patient was referred for surgical resection.
Discussion
Cardiac papillary fibroelastomas (CPFs) are considered the second most common benign primary cardiac tumor after myxoma [5]. Characteristically they have a short pedicle and multiple papillary fronds similar to a sea anemone. They often (85%) originate from the valvular endocardium. The aortic valve (29%), mitral valve (25%), tricuspid valve (17%) and pulmonary valve (13%) are involved in that order [2]. However, CPFs arising from semilunar valves are located with equal frequencies on the ventricular and arterial sides of the valves. In addition, non-valvular origin was observed in approximately 16% cases that included left and right ventricular septal and mural endocardial surfaces, atrial endocardium, papillary muscles, chordae tendinae or intima of the right coronary ostium [3].
The majority of patients are asymptomatic and the tumors are most often incidentally diagnosed at the time of routine echocardiography, cardiac catheterization, cardiac surgery or autopsy. Although histologically benign, CPFs have the potential to lead in life threatening complications from embolization of fragments into the coronary arteries, systemic circulation and pulmonary circulation depending on their size, mobility and location [4]. The mechanism of these complications could be either by the fragmentation of the CPF, or by the disintegration of the thrombi that have adhered to the surface of these tumors. Also, there is another mechanism that is the prolapse of the tumor itself into any coronary ostium leading to an acute myocardial infarction [1].
Large retrospective studies estimate the risk of CPF related stroke or transient ischemic attack at 6% at 1 year to 13.5% at 5 years and the recurrence of stroke in non resected tumors around 16% to 24%, with a mean follow-up of 31 months [6] However, the prevalence is not well documented, and this makes the need for anticoagulation unclear [7]. Clinical presentation of CPFs varies from asymptomatic to severe thromboembolic complications. However, pulmonary embolism, congestive heart failure, near syncope, ventricular fibrillation and sudden death have also been reported. The transesophageal echocardiography is superior to the transthoracic one in the detection, the localization and the description of the cardiac masses and it has better visualization of valves and cardiac chambers [1] It provides the best spatial and temporal resolution and demonstrates an overall sensitivity of 77% rendering it first choice among the different cardiac imaging modalities [4].
Cardiac magnetic resonance imaging scans allow, on top of the previous, a tissue characterization and enhancement pattern, evidencing T2 hyperintensity due to the high proportion of connective tissue and mucopolysaccharide matrix, with atypical enhancement due to the avascular nature of these lesions [7]. Surgical excision is the sole curative treatment of CPF, which was performed for the first time by Licht-enstein in 1979. During the procedure all cardiac chambers and valves must be inspected to eliminate other localizations of the tumor, and sometimes to look for the association of CPF with vegetations. Furthermore, valvular regurgitation can be caused either by the tumor itself or by the surgeon after the excision. In this matter, the surgical procedure must be completed either by valvular repair, every time the valve is repairable, otherwise valvular replacement can be done [1].
Therapeutic decisions should take into consideration not only the presence of symptoms but also the potential of life threatening complications. There is a general consensus that symptomatic patients should be referred for curative surgical excision of the tumour. In addition asymptomatic patients with large (>1 cm) mobile masses especially left sided, as in our case, should also be considered candidates for curative surgical excision due to the increased risk of cardiovascular complications from embolization and sudden cardiac death. On the other hand, asymptomatic patients with small left sided non mobile lesions are being closely followed up with echocardiography until symptoms develop or tumours enlarge and become mobile [4].
Conclusion
In conclusion, this case contributes to highlighting that CPFs are a rare but potentially significant cause of cardioembolic stroke among the elderly population and should be considered in the differential diagnosis of a cardiac valve mass. Once diagnosed, surgical resection is required in most cases for reducing the risk of stroke recurrence.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Reda Bzikha, Amin Serradj, Sébastien Querona (2021) Papillary fibroelastoma of aortic valve mimicking an infective endocarditis. Cirugía Cardiovascular 28(5): 300-303.
- Grinda JM, Couetil JP, Chauvaud S, D’Attellis N, Berrebi A, et al. (1999) Cardiac valve papillary fibroelastoma: surgical excision for revealed or potential embolization. J Thorac Cardiovasc Surg 117(1): 106-110.
- Neerod K Jha, Michael Khouri, Donogh M Murphy, Alessandro Salustri, Javed A Khan, et al. (2010) Papillary fibroelastoma of the aortic valve - a case report and literature review. Journal of Cardiothoracic Surgery 5: 84.
- Fragiskos Parthenakis, Evangelia Nyktari, Alexandros Patrianakos, Antonis Pitsis, Anthoula Asimaki, et al. (2009) Asymptomatic papillary fibroelastoma of the Aortic valve in a young woman. Cardiovascular Ultrasound 7: 43.
- Tamin SS, Maleszewski JJ, Scott CG, Khan SK, Edwards WD, et al. (2015) Prognostic and bioepidemiologic implications of papillary fibroelastomas. J Am Coll Cardiol 65: 2420-2429.
- Bonavia L, Jackson J, Pui-Yee Law J, Yii M, Joshi D (2019) Brainstem stroke caused by left atrial cardiac papillary fibroelastoma: an increasingly recognized rare cause of stroke. Cardiovasc Pathol 40: 65-67.
- Laura Esteban Lucía, Soraya De la Fuente Batista, Andrea María Kallmeyer Mayor, Marcelino Cortés García (2021) Cardioembolic Stroke Secondary to an Aortic Valve Fibroelastoma: An Increasingly Recognized Rare Cause of Stroke. Stroke 52: e111-e114.
-
Jennane Ratiba*, Souilk Houda, Hilal Safae and Mesmoudi boutaina. Embolic Stroke from Aortic Valve Papillary Fibroelastoma an Unsuspected Finding. On J Cardio Res & Rep. 6(5): 2022. OJCRR.MS.ID.000648.
-
Cardiac papillary fibroelastoma, Stroke, Aortic valve, Cardioembolic stroke, Myocardial infarction, Echocardiogram, Neurology, Left hemiplegia, Dysarthria, Aortic valve, Mitral valve, Tricuspid valve, Pulmonary valve
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






