 Research Article
Research Article
Does Interleukin-2 Predict Success of Thrombolytic Therapy
Abdel Mohsen Mostafa Aboualia1*, Eman Rashed Zaky1 and Mohamad Yousri Shaheen2
1Department of Cardiology, Al-Azhar University, Egypt
2Department of Clinical pathology, Al-Azhar University, Egypt
Abdel Mohsen Mostafa Aboualia, Department of Cardiology, Al-Azhar University, Cairo, Egypt.
Received Date: June 05, 2020; Published Date: June 19, 2020
Abstract
Background: Atherosclerosis and its complication is proved to be an inflammatory process with increasing evidence of the role of cytokines in atherosclerosis pathophysiology.
Objective: To investigate the predictive role of admission level of interleukin-2 (IL-2) in acute myocardial infarction patients in detecting success of thrombolytic therapy.
Patients and Method: Forty patients with the diagnosis of ST-elevation myocardial infarction (STEMI) (20 patients diagnosed as STEMI with successful thrombolytic therapy and 20 patients diagnosed as STEMI with failed thrombolytic therapy) from those attending the Coronary Care Units in Cardiology department Al Hussein university hospital between April to May 2013 underwent echocardiography and baseline and after 3days follow up of IL-2 level .
Results: The age in STEMI success group was 44.7 ± 9.41 years while in the failed thrombolytic group 58.3 ± 7.93 years, hypertension (HTN) and diabetes mellitus (DM) were more prevalent in STEMI success group while smoking more in thrombolytic failed group. In the present study, Interleukin-2 was 274.3 ± 104.2 pg/ml in STEMI success group and 215.1 ± 49.4 pg/ml in STEMI failed group with no significant difference.
Conclusions: Admission level of serum IL-2 failed to predict the success of thrombolytic therapy
Introduction
Acute coronary syndrome (ACS) is the most common presentation of cardiovascular disease. Sensitive biomarkers improve the diagnosis of ACS among clinician leading to advancement in the management and reduction in mortality [1]. Till this time the superiority of primary percutaneous coronary intervention (PPCI) in those patient is evidence based. ST-elevation myocardial infarction (STEMI) patients presented in COVID-19 era or to hospitals without PCI facilities should receive thrombolytic therapy. Prediction of success is crucial to determine eligibility for thrombolytic therapy. Interleukin-2 (IL-2) has multiple functions, sometimes opposing to each other during an inflammatory response. IL-2 has osteoprotective effect on regulatory cells expansion. Also, IL-2 stimulates natural killer cells to proliferate and induces cytolytic activity when present at high levels and stimulates B cells division and antibody production. So, it has a role in the atherosclerosis inflammatory process and its sequale [2]. Recent studies have shown that IL-2 has an action on atherosclerosis and remodeling after myocardial infarction in mice [3]. But there is lack of results about IL-2 as a predictor of thrombolysis success.
Aim of the Work
To investigate the predictive role of admission level of interleukin-2 (IL-2) in acute myocardial infarction patients in detecting success of thrombolytic therapy.
Patients and Method
This study was included (40) patients with the diagnosis of STEMI from those attending the Coronary Care Units in Cardiology department Al-Hussein university hospital, between April 2013 and August 2013.
The studied population were classified into two equal groups based on thrombolysis success
STEMI success group: ST segment elevation myocardial infarction group with successful thrombolytic therapy which included 20 patients.
STEMI failed group: ST segment elevation myocardial infarction group with failed thrombolytic therapy which included 20 patients.
Exclusion criteria: previous myocardial infarction or coronary intervention in the last three month, active inflammation, or active immunological diseases.
Method
After informed consent was taken, all patients underwent the following: -
1. Detailed history with special emphasis on: Age and gender, smoking, diabetes mellitus, hypertension, and dyslipidemia.
2. Clinical (general, cardiac) examination.
3. Laboratory work up including
a) Cardiac enzyme creatine kinase-myocardial band (CKMB) and troponin I to diagnose STEMI.
b) Serum interleukin-2: by ELISA at time of admission and after 7 days (Orgenium Laboratories’ Tiilitie 3 FIN-01720 Vantaa FINLAND).
4. Resting 12 leads ECG to diagnose TSEMI based on fourth universal definition of myocardial infarction [4].
5. Resting conventional trans-thoracic echocardiography at time of admission with the patients in the left lateral decubitus. Images were obtained using Philips IE 33 X machine. Recordings and calculations of Aortic root, Left atrium dimension, internal measurements of the LV and LV systolic function using biplane modified Simpson’s methods [5].
6. The patients were classified according to the success of thromboolysis identified by – resolution of chest pain, accelerated idio-ventricular rhythm (AIVR), and ST segment Resolution (STR) >50% in the lead with maximum ST elevation in pre-Thrombolytic ECG after 2 hours of streptokinase infusion [6].
7. Statistical Analysis of the Data The data were analyzed statistically using IBM-SPSS-22 (Statistical Package for Social Science version 22). Means and standard deviation were used to describe data distribution. t-test was used for comparison between groups. The test was considered significant if the probability (p-value) was less than 0.05.
Result
The clinical findings of the patients
Age
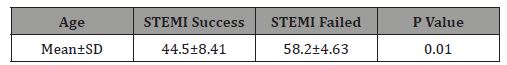
The age was lower in STEMI success group than STEMI failed group (44.5±8.41 versus 58.2±4.63 years) and this difference is statistically significant (p value = 0.01) (Table 1).
Table 1: Comparison between the groups regarded to age (years).
Gender
No statistically significant difference between the groups as regard gender (21 patients (70%) were males in STEMI success group and 24(80%) in STEMI failed group) with P value >0.05.
Risk factors
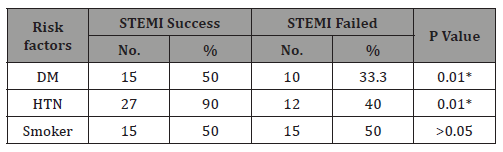
Regarding to the risk factors, in STEMI success group 10(50%) of the patients had diabetes mellitus, 16(90%) had hypertension and 10(50%) were smoker and in STEMI failed group 7(35%) of the patients had diabetes mellitus, 8 (40%) had hypertension and 10(50%) were smoker. There was a statistically significant differences between the two groups as regard diabetes mellitus and hypertension (Table 2).
Table 2: Comparison between the groups regarded to risk factors.
Interleukin-2 level at time of admission and after 3 days: (pg/dl)
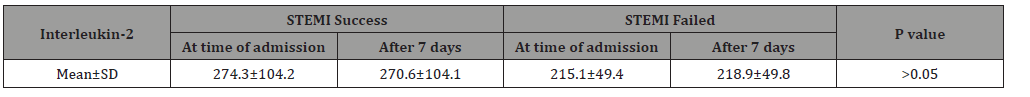
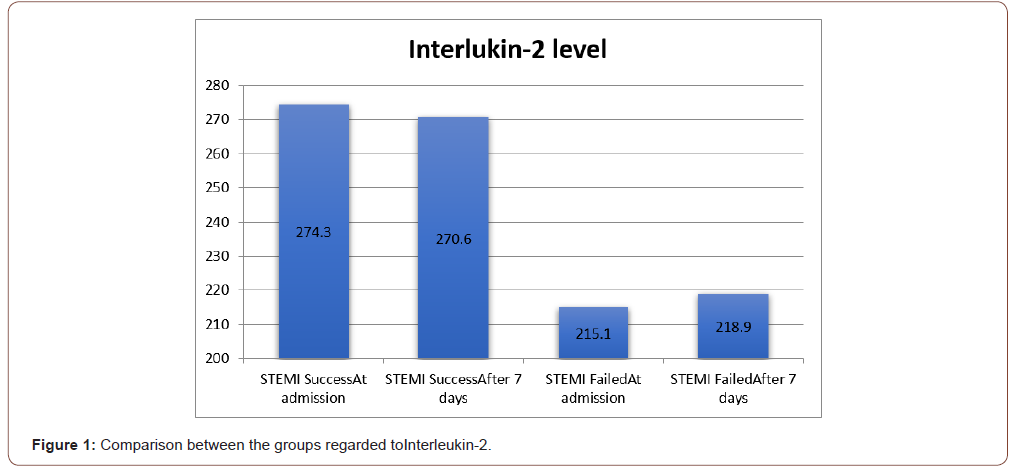
Regarding to the Interleukin-2, in STEMI success group it ranged between 140-475 pg/dl and mean±SD was 274.3±104.2 pg/dl and in STEMI failed group it ranged between 146-290 pg/dl and mean±SD was 215.1±49.4 pg/dl. After 3 days, in STEMI success group mean±SD was 270.6±104.1 and in STEMI failed group mean±SD was 218.9±49.8. There was no statistically significant difference between the four groups with P> 0.05 (Figure 1 & Table 3).
Table 3: Comparison between the groups regarded to risk factors.
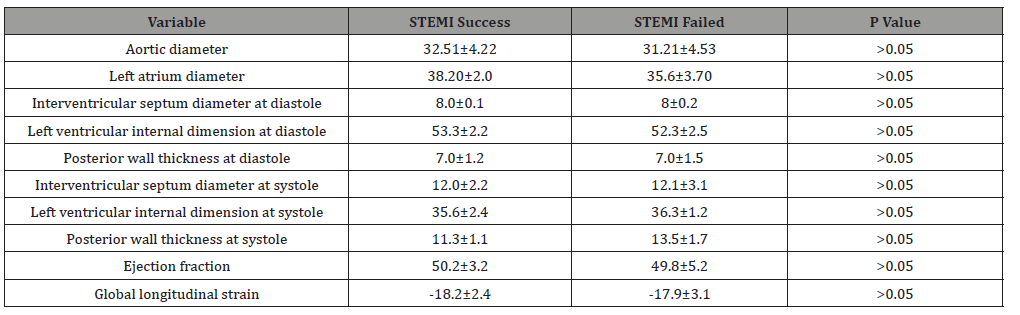
Echocardiographic parameters
No significant difference between the two groups regarding conventional echo-parameters. Global longitudinal strain of LV was reduced in both groups and more in STEMI failed group although this difference is not significant (p value >0.5) (Table 4).
Table 4: Echo parameters of the two groups at time of admission.
Discussion
There has been more evidence of the role of immune and inflammatory processes in the development and progression of atherosclerosis. Macrophages and T lymphocytes have many roles one of them release of cytokines [7]. Also, nowadays increasing roles of targets therapy for atherosclerosis made plenty of cytokines research [8]. Interleukin-2 (IL-2) is a small α-helical cytokine that regulates immune cell homeostasis and discovered more than 30 years earlier. IL-2 showed to have therapeutic efficacy for immune diseases by its anti-inflammatory action mediated by regulatory T cell expansion. Combining this finding with the pathophysiology of myocardial infarction in the form of plaque rupture and erosions elucidate the protective role of this cytokine in myocardial infarction [9].
In Dinh, et al. [10] the IL‐2 complex ( composed of IL‐2 and anti‐IL‐2 monoclonal antibody ) was found to selectively expands the athero-protective regulatory T cells up to 6 times and effectively inhibits the development and progression of atherosclerosis in Apolipoprotein E ‐/‐ mice. So, significantly attenuates the ventricular remodeling and resulting in reduced infarct size with improved left ventricular (LV) function after myocardial infarction. Also, Webster, et al. [11] demonstrated that IL‐2 attenuated cardiomyocyte apoptosis in a mouse myocardial infarction model. Zeng, et al. [3] demonstrated that IL‐2 complex exerts cardiac protective effects by directly inhibiting the infiltration of macrophages and facilitating the polarization of anti‐inflammatory M2 macrophages, which results in attenuation of cardiomyocytes apoptosis and the inflammatory responses. The expansion of regulatory T cells by the IL‐2 complex may be a potentially valuable approach in improving ischemic heart disease.
In Bouchentouf, et al. [12] found that a single intravascular injection of recombinant human IL‐2(rhIL‐2) two days after myocardial infarction improved the ejection fraction of left ventricular by 27.7% of immune competent mice but no effect on the ejection fraction of the immune-deficient mice. Cardiac angiogenesis and decreased collagen deposition were enhanced by the administration of rhIL‐2 and this help to preserve the integrity and function of myocardium especially in the scar and border areas of infracted myocardium. In this study no gender difference between the groups with diabetes mellitus and hypertension were more prevalent in STEMI success group. In Ding, et al. [7] hypertension more prevalent in CAD group (46.5%).
In the current study, patients were presented by STEMI and underwent thrombolysis; half of them respond successfully to thrombolytic therapy. Although the level of interlukin-2 was lower in failed to respond to thrombolytic group at baseline and after 3 days this difference was non-significant statistically. In this study no role for echocardiography in prediction of outcome of thrombolytic therapy and no previous known study addressed this issue. The elevation of these markers in STEMI success group may be explained by the release of metabolites after pharmacological revascularization. IL-2 may be induced in the repercussed myocardium to modulate the reaction to injury. In other words, increased levels of IL-2 suggest good reperfusion, while low of IL-2 level means ischemic but not repercussed myocardium.
Ding, et al. [7] found an increased IL-2 expression in CAD patients (39 pg/ml) than in healthy controls (27 pg/ml) (p < 0.01) but they did not risk stratify the patients. This study is the first to study interlukin2 as a predictor for successful thrombolysis in acute myocardial infarction patients.
Conclusion
Admission level of serum IL-2 failed to predict the success of thrombolytic therapy and we must search for another cytokine as a predictor.
Acknowledgement
All co-authors contributed equally to the article.
Conflict of Interest
No conflict of interest.
References
- Melo L, Duarte J, Roque D, de Oliveira IF, Faustino A, et al. (2017) Infectious Endocarditis: Sample from the Department of Internal Medicine of a Hospital. Internal Medicine 24 (1): 19-23.
- Teixeira J, Marques A (2019) Prophylaxis of Bacterial Endocarditis: State of the Art. Journal of the Portuguese Society of Anesthesiology 28(3): 174-180.
- Sobreiro D, Sampaio R, Siciliano R, Brazil C, Branco C, et al. (2018) Early Diagnosis and Treatment in Infective Endocarditis: Challenges for a Better Prognosis. Arquivos Brasileiros de Cardiologia 112(2): 201-203.
- Gutierrez P, Calderaro D, Caramelli B (2004) Infectious endocarditis. Magazine of the Brazilian Medical Association 50(2): 118-119.
- Madeira MP (2018) Profile of inpatients diagnosed with Infectious Endocarditis in the Internal Medicine service of a Tertiary Hospital in Ceará.
- Bravo DPL, Coelho APP, Dahia CB, Bicudo FB, Santos JEP (2018) Treatment of Infectious Endocarditis with Valve Replacement. Notebooks of Medicine-UNIFESO 1(1).
- Garrido RQ (2016) Risk factors for early infectious endocarditis of prosthetic valves: a case-control study.
- Lamas C (2020) Infective Endocarditis: Still a Deadly Disease. Brazilian Archives of Cardiology 114(1): 9-11.
- Galvao JLFM (2016) Endocarditis infection: a review of the microorganism for treatment.
- Marques A, Cruz I, Caldeira D, Alegria S, Gomes AC, et al. (2019) Risk Factors for In-Hospital Mortality in Infective Endocarditis. Brazilian Archives of Cardiology.
- Marti-Carvajal AJ, Dayer M, Conterno LO, Garay AGG, Marti-Amarista CE (2020) A comparison of different antibiotic regimens for the treatment of infective endocarditis. Cochrane Database Syst Rev (5).
- Sotero FD, Rosario M, Fonseca AC, Ferro JM (2019) Neurological complications of infective endocarditis. Curr Neurol Neurosci 19(5): 23.
- De goes Marques CR (2018) Infectious endocarditis as a risk factor for ischemic stroke: an integrative review. Research Week at Tiradentes University-SEMPESq (18).
- Mondragao A, Ramos AR, Barbedo M (2017) Infectious endocarditis as a risk factor for ischemic stroke. An integrative review 78(2): 73-75.
- Yellapu V, Ackerman D, Longo S, Stanislaw PS (2018) Septic embolism in endocarditis: Anatomic and pathophysiologic considerations. In Advanced Concepts in Endocarditis. IntechOpen 149.
-
AbdelMohsen Mostafa Aboualia, Mohamad Yousri Shaheen. Does Interleukin-2 Predict Success of Thrombolytic Therapy. On J Cardio Res & Rep. 4(2): 2020. OJCRR.MS.ID.000583.
-
Endocarditis, Bacterial infection, Heart disease, Endocardium, Heart valves, Intestinal pneumatosis, Prosthetic valve, Septic embolism, Predisposition, Fever, Vascular, Immunological phenomena, Microbiological, Echocardiographic evidence
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






