 Research Article
Research Article
Complications and Predictors of Postoperative Mortality in Patients Undergoing Valve Replacement Surgery
Alexander Valdés Martín1*, César Cáceres Roselio1, Lidia María Rodríguez Nande1, Nurys Bárbara Armas Rojas1, Ana Barbara González Espinosa1, Oscar Reynaldo Alave Apaza1 and Sol Rocío Rodríguez Alvarez1
Institute of Cardiology and Cardiovascular Surgery, Cuba
Institute of Cardiology and Cardiovascular Surgery, Cuba.
Received Date:April 07, 2022; Published Date:April 21, 2022
Abstract
Introduction: Valvulopathies continue to be an important cause of medical consultation and hospitalization. Objective: to identify the main complications and predictors of postoperative mortality in patients undergoing valve replacement surgery.
Methods: An observational, analytical and retrospective study was carried out. The universe consisted of 753 patients.
Results: The main complications reported were the need for electric shocks (29.2%), ventricular fibrillation (28.4%) and endocarditis (9.2%). Patients alive at hospital discharge predominated. The complications most related to mortality were cardiogenic shock (18.0%), low output (28.0%) and sepsis (18.0%). Age greater than or equal to 65 years almost tripled the risk of death. Women were 2.5 times more likely to die before hospital discharge. A glomerular filtration rate below 60 ml/min/1.73m2 is a predictor of mortality.
Conclusion: Extracorporeal circulation remains the technique of choice for valve replacements which together with good myocardial protection and short anoxic arrest, extracorporeal circulation and surgical times decrease perioperative morbidity and mortality. Surgery is a safe and viable option for these patients, although it is not free of complications. The last one includes the appearance of arrhythmias as a result of alterations in the internal environment and acid-base balance. Aging, the presence of comorbidities such as diabetes and impaired renal function in patients with valvular heart disease predispose to the development of complications and death in the postoperative period.
Keywords:Valvulopathies; Surgery; Mortality; Morbidity; Sepsis
Introduction
Valvulopathies continue to be an important cause of medical consultation and hospitalization worldwide [1]. The improvement in the prevention of rheumatic heart disease and the phenomenon of epidemiological transition has allowed mortality from degenerative heart valve disease to be higher in elderly patients [2]. In Cuba, at the end of 2020, the rate of deaths due to non-rheumatic valvulopathies was 2.7 per-100,000 inhabitants [3]. Early detection and grading of the severity of valvular heart disease has improved the criteria for selecting patients who are candidates for surgery. In addition, advances in surgical techniques and perioperative management have resulted in a higher success rate and lower morbidity and mortality [4]. Cardiac valve surgery (CVC) requires a specific operative procedure for its performance. The complexity of these procedures is related to patient and surgical factors such as the number of valves to be operated on, the existence of previous cardiac surgery, the association with revascularization or thoracic aortic surgery and the quality of myocardial protection provided during the surgical procedure, among other factors [5].
Prior identification of all the factors and conditions that favor postoperative complications, together with the availability of resources and access to health care in each region or country, influence the quality and success of the CVC [6]. The purpose of this study conducted at the Institute of Cardiology and Cardiovascular Surgery (ICCCV) was to identify the main complications and predictors of postoperative mortality in patients who underwent valve replacement surgery.
Method
An observational, analytical and retrospective study was carried out at the ICCCV in Havana from January 1, 2016 to December 31, 2019. The universe consisted of 753 patients who met the inclusion criteria of being patients of both sexes, aged over 18 years, diagnosed with any valvulopathy and approved as candidates for CVC. Patients with combined cardiac conditions (valvular heart disease and coronary artery disease), psychiatric patients with difficulties in responding to adequate questioning, patients with a poor acoustic window for echocardiography and patients with consumptive diseases, neoplasms, and acquired immunodeficiency syndrome were excluded.
Variables and their operationalization
The following variables were included in the study: sociodemographic (age and sex) and pre-surgical variables that were grouped into: Clinical variables: arterial hypertension, diabetes mellitus, stroke, chronic kidney disease, chronic obstructive pulmonary disease (COPD), pulmonary hypertension, arrhythmias, bronchial asthma, smoking habit. Laboratory variables: total proteins, creatinine, glomerular filtration rate (GFR). Echocardiographic variables: valvular lesions, left ventricular ejection fraction (LVEF).
Procedural techniques and data collection
The information was obtained from the medical records and echocardiography reports. The data were collected in a model elaborated for this purpose that collected the variables of interest.
Processing and analysis techniques
Frequency distribution tables were prepared and statistical methods were applied using SPSS (Stadistical Pachage for Social Sciences) version 18.0 for Windows. Summary measures were used for descriptive variables, mean, standard deviation and percentage according to the type of variable. Descriptive statistical techniques such as mean and standard deviation were used.
Ethical Aspects
The research was approved by the scientific board and the ethics committee of the participating institution. The integrity of the data obtained was jealously guarded. The ethical principles for medical research in humans established in the Declaration of Helsinki were complied with at all times.
Result
Patients aged 60 years or older accounted for 52.2% of the total sample. The male sex (52.3%) predominated over the female sex (47.7%). Among the main pathologic antecedents of these cases, arterial hypertension (53.5%), pulmonary hypertension (14.1%) and diabetes mellitus (11.9%) stood out. A total of 31.2% were reported to be former smokers. Aortic valve replacement (48.5%) was the most commonly used surgery, followed by mitral valve replacement (36.7%) and double replacement (14.5%). More than 60% of the patients had filtration values included in categories 1 and 2 and more than 90% of the cases had left ventricular ejection fraction values above 50%. (Table 1) shows variables related to the surgical procedure. The median arrest time was 80 minutes and that of extracorporeal circulation almost 2 hours, while the surgical time and anesthesia time were 4 hours and 5 hours, respectively.
Electrical complications were the most frequent. The use of electric shocks was necessary in 29.2% of the cases. Among the septic complications, endocarditis was the most frequent (9.2%) and the main causal microorganism was staphylococcus aureus (6.9%) (Table 2). 50 patients died in this study which represented 6.6% of the sample. The complications most related to mortality were the cardiogenic shock (34.0%), low output (28.0%) and sepsis (18.0%) (Table 3). It was of interest to know the possible associations between the variables collected and mortality. (Table 4) shows the patient´s distribution according to sociodemographic and clinical variables in relation to the patient’s condition at discharge. Statistically significant differences were observed for age both in mean values (58.9 vs. 63.9, p= 0.002) and in patients aged 65 years and older (34.4% vs. 60.0%, p = 0.0003). Diabetes mellitus was present in 32.0% of deceased patients in contrast to 10.5% of those discharged alive (p < 0.0001). Regarding renal function, although with normal values, creatinine was slightly higher in deceased patients (p=0.051) and glomerular filtration rate was decreased in this group (81.8 vs. 70.2, p= 0.025).
Table 1: Distribution of patients according to variables related to the surgical procedure.
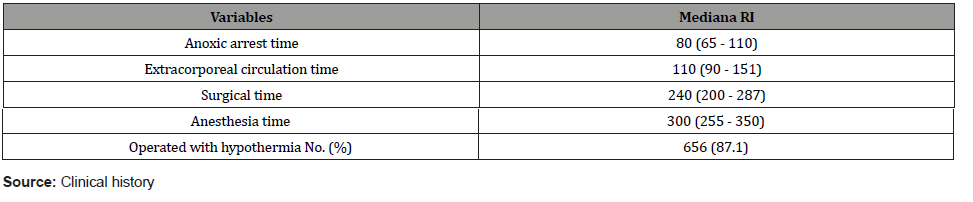
Table 2: Distribution of patients according to trans-operative complications.
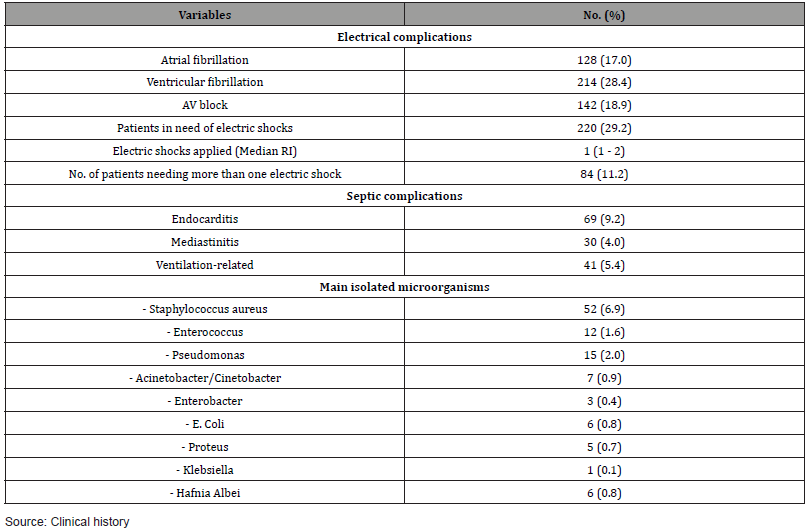
Table 3: Distribution of patients according to operative mortality.
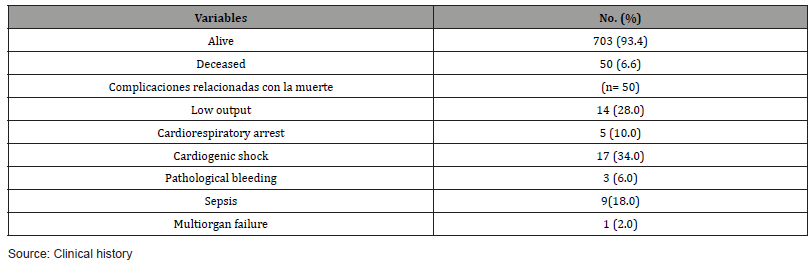
Table 4: Distribution of patients according to sociodemographic and clinical variables in relation to the patient’s condition at discharge.
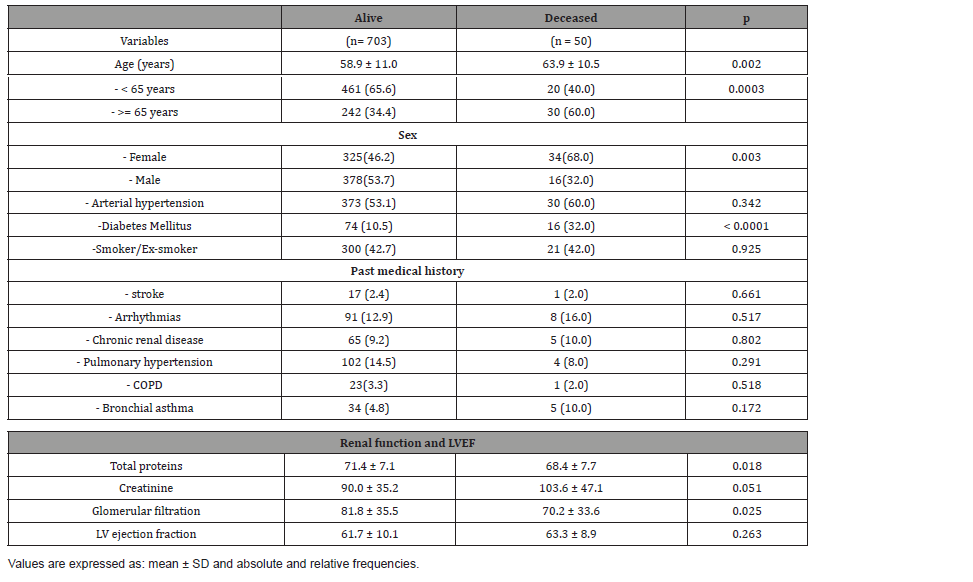
Table 5: Distribution of patients according to variables related to the surgical procedure in relation to the patient’s condition at discharge.
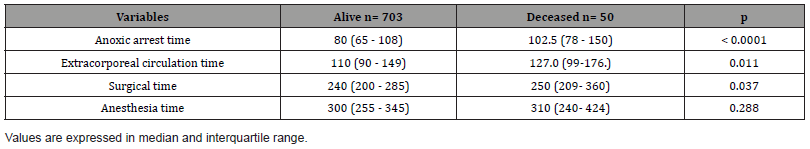
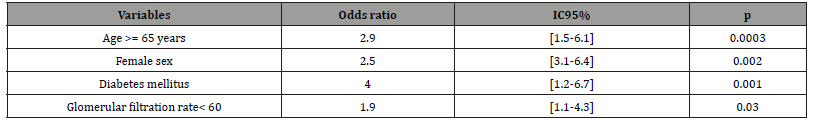
Table 6: Reasons for Disparity with respect to death.
A similar analysis was performed with respect to mortality with the variables related to the surgical procedure. (Table 5) shows the results, highlighting higher median values for anoxic arrest time (80 vs 102.5), extracorporeal circulation (110 vs 127) and surgical time (240 vs 250) all statistically significant.
Variables found to be significant in the above analyses with respect to mortality were included in a logistic regression analysis to obtain the disparity ratios shown in (Table 6). Age greater than or equal to 65 years almost tripled the risk of dying. Women were 2.5 times more likely to die before discharge after valve surgery. A glomerular filtration rate below 60 ml/min/1.73m2 is a predictor of mortality in these patients, almost doubling the risk of occurrence of this adverse event. Diabetes mellitus was a predictor of mortality since patients with this risk factor had a disparity ratio of 4.0, CI = (1.2 - 6.7), the highest in our series.
Discussion
The aging of the population brings with it an increase in the incidence of heart valve disease, particularly aortic valve disease. Therefore, the number of surgical interventions should benefit an increasing number of patients in the future [7-9]. Valve replacement is usually performed by cardiovascular surgeons with experienced Techniques [10]. This explains why, in this study, most of the valves were replaced with stopping times of less than or equal to 120 minutes. The literature consulted showed a correlation between insufficient myocardial protection, the onset of myocardial necrosis and prolonged arrest times in patients who suffered perioperative myocardial infarction and postoperative cardiogenic shock [11,12]. It was found that most of the valves in this study were replaced with an extracorporeal circulation time of 110 minutes. These times are relatively short and are related to the expertise of the surgeons involved. The use of extracorporeal circulation allows the surgeon to work in a still and bloodless field, but can cause varying degrees of myocardial stunning. This is why, when the patient has a pre-existing deterioration in systolic function, he is most likely to present low cardiac output due to a transient worsening in contractility due to the impact of the pump at the level of the cardiac muscle [13,14].
Increased time in circulation is recognized as a “life-threatening” condition that can lead, if unsuccessful, to intraoperative death. Blood contact with non-endothelialized surfaces can lead to thrombocytopenia, platelet dysfunction, consumption of clotting factors and activation of the fibrinolytic system. All these hematological disorders will be more accentuated the longer the pump time. The objective when weaning from extracorporeal circulation is that the cardiovascular apparatus should allow the patient to maintain sufficient oxidative metabolism and tissue perfusion to meet its own demand [15,16]. Electrical complications were the most frequent. The use of electric shocks was necessary in 29.2% of cases for the recovery of sinus rhythm, followed by ventricular fibrillation with 28.4%. The predominance of ventricular arrhythmias during the first moments of reperfusion is frequent and is conditioned by a series of mechanisms such as the duration of the ischemia period, the severity of the metabolic changes produced by ischemia, cytosolic calcium oscillations, the flow of catecholamines produced during ischemia and even the speed of reperfusion itself [17]. Other favorable circumstances could be the hydroelectrolytic alterations, the release of oxygen free radicals (superoxide O2, hydrogen peroxide H2O2 OH and hydroxyl OH), ventricular dysfunction and hemodynamic instability [18]. All these changes arising during the ischemia-reperfusion phenomenon linked to extracorporeal circulation act as facilitators of automaticity and/or modifiers of cell membrane properties.
Valvular prosthesis infective endocarditis (VPIE) occurs in about 1%-6% of patients with valve prostheses. It has an incidence of about 0.3-1.2% per patient per year. VPIE was the most frequent infectious complication in this investigation and occurred with a higher frequency than reported in the literature (9.2%) [19]. Early VPIE can develop as a result of nosocomial or health care-related bacteremia [20,21]. VPIE can be acquired in the operating room during surgery, by surgical wound infection or through intravascular catheters in the post-surgical care unit, so that microorganisms such as coagulase-negative and aureus staphylococci, enterococci, fungi and gram-negative bacilli predominate in its etiopathogenesis [21]. These approaches coincide with the results of this study where the main causal germ reported was staphylococcus aureus (6.9%) and another complication reported was mediastinitis (4%). It should be taken into account that perioperative antibiotic prophylaxis is very beneficial in reducing the incidence of infectious complications in patients undergoing cardiac Surgery [22].
In our study, 50 patients died, representing 6.6% of the population studied. The complications most related to mortality were cardiogenic shock (18.0%), low cardiac output (28.0%) and sepsis (18.0%). These results are partially concordant with the study by De la Peña Riveron and collaborators [23], who found postoperative low cardiac output syndrome, atrioventricular block and neurological complications as predictors of postoperative mortality. In the aforementioned research, cardiogenic and hypovolemic shock were reported in 6.7%, while acute myocardial infarction and pulmonary thromboembolism had one death each (3.3%) [23]. In this study performed at the ICCCV, age greater than or equal to 65 years, female sex, a glomerular filtration rate below 60 ml/min/1.73m2 and diabetes mellitus were predictors of mortality in patients who underwent valve disease surgery, almost tripling the risk of death. This is in correspondence with what has been reviewed in case series with similar characteristics to ours. Many variables have been pointed out as predictors of mortality, among which advanced age, female sex, urgent surgery, associated coronary revascularization, reoperation, depressed left ventricular ejection fraction, renal failure, and even the number of hospital interventions stand out [24, 25].
Morbidity and mortality associated with valve replacement surgery at a global level has decreased in recent years due not only to advances in surgical technique and myocardial preservation, but also to the fact that valve lesions are detected at earlier stages and that the selection of patients who undergo surgery is more appropriate [26, 27].
Conclusion
1. Extracorporeal circulation continues to be the technique of choice for valve replacements, which, together with good myocardial protection and short anoxic arrest, CPB and surgical times, reduces perioperative morbidity and mortality.
2. Complications in patients operated on for valvular disorders are low, with a predominance of arrhythmias that generally occur due to alterations in the internal environment and acid-base balance.
3. Aging, the presence of comorbidities such as diabetes and impaired renal function predispose to the development of complications that lead to death in these patients in the postoperative period.
4. Surgery is a safe and viable therapeutic option for patients with valvular apparatus diseases, although it is not free of complications, so adequate preparation and multidisciplinary discussion is necessary in each case.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Mulugeta T, Kumela K, Chelkeba L (2020) Clinical, Echocardiographic Characteristics and Management Practices in Patients with Rheumatic Valvular Heart Disease. Open Access Rheumatol 12: 233-239.
- Rostagno C (2019) heart valve disease in elderly. World J Cardiol 11(2): 71-83.
- Ministry of Public Health. Statistical Yearbook of Cuba (2020) Havana: National Directorate of Medical Records and Health Statistics.
- Remenyi B, ElGuindy A, Smith SC Jr, Yacoub M, Holmes DR Jr (2016) Valvular aspects of rheumatic heart disease. Lancet 387(10025): 1335-1346.
- Baikoussis NG, Papakonstantinou NA, Verra C Kakouris G, Chounti M, Hounti P, et al. (2015) Mechanisms of oxidative stress and myocardial protection during open-heart surgery. Ann Card Anaesth 18(4): 555-564.
- González Kadashinskaia GO, Bello Carrasco LM, Anchundia Alvia DA (2020). Cardiac surgery, immediate postoperative complications. University and Society Magazine.
- Bhatia N, Basra SS, Skolnick AH, Wenger NK (2016) Aortic valve disease in the older adult. J Geriatr Cardiol 13 (12): 941-944.
- Li G, Li T, Chen Y, Guo X, Li Z, et al. (2021) Associations between aortic regurgitation severity and risk of incident myocardial infarction and stroke among patients with degenerative aortic valve disease: insights from a large Chinese population-based cohort study. BMJ Open 11(8): e046824.
- Keymel S, Hellhammer K, Zeus T, Merx M, Kelm M, et al. (2015) Severe aortic valve stenosis in the elderly: high prevalence of sleep-related breathing disorders. Clin Interv Aging 10: 1451-1456.
- Head SJ, Çelik M, Kappetein AP (2017) Mechanical versus bioprosthetic aortic valve replacement. Eur Heart J 38(28): 2183-2191.
- Misra S, Srinivasan A, Jena SS, Bellapukonda S (2021) Myocardial Protection in Adult Cardiac Surgery With del Nido Versus Blood Cardioplegia: A Systematic Review and Meta-Analysis. Heart Lung Circ 30(5): 642-655.
- DiMarco RF Jr (2010) Postoperative Care of the Cardiac Surgical Patient. Surgical Intensive Care Medicine pp. 535-566.
- Epting CL, McBride ME, Wald EL, Costello JM (2016) Pathophysiology of Post-Operative Low Cardiac Output Syndrome. Curr Vasc Pharmacol 14(1):14-23.
- Muir WW and Hamlin RL (2020) Myocardial Contractility: Historical and Contemporary Considerations. Front Physiol 11: 222.
- Beyersdorf F, Trummer G, Benk CH, Pooth JS (2021) Application of cardiac surgery techniques to improve the results of cardiopulmonary resuscitation after cardiacarrest: Controlled automated reperfusion of the whole body. JTCVS Open 8: 47-52.
- Beyersdorf F (2017) New dimensions for extracorporeal circulation. Interact CardioVasc Thorac Surg 24: 479-481.
- Salazar Ramírez F, Ramos Mondragon R, Garcia Rivas G (2021) Mitochondrial and Sarcoplasmic Reticulum Interconnection in Cardiac Arrhythmia. Cell Dev. Biol 8: 623381.
- Hancock JT (2021) Oxygen Is Instrumental for Biological Signaling: An Overview. Oxygen 1: 3-15.
- Koneru S, Huang SS, Oldan J, Betancor J, Popovic ZB, et al. (2018) Role of preoperative cardiac CT in the evaluation of infective endocarditis: comparison with transesophageal echocardiography and surgical findings. Cardiovasc Diagn Ther 8(4): 439-449.
- Hryniewiecki T, Zatorska K, Abramczuk E, Zakrzewski D, Szymański P, et al. (2019) The usefulness of cardiac CT in the diagnosis of perivalvular complications in patients with infective endocarditis. Eur Radio 29(8): 4368-4376.
- Galar A, Weil AA, Dudzinski DM, Muñoz P, Siedner MJ (2019) Methicillin-Resistant Staphylococcus aureus Prosthetic Valve Endocarditis: Pathophysiology, Epidemiology, Clinical Presentation, Diagnosis, and Management. Clin Microbiol Rev 32(2): e00041-18.
- Tchana Sato V, Hans G, Frippiat F, Zekhnini I, Dulgheru R, et al. (2020) Surgical management of Staphylococcus capitis prosthetic valve infective endocarditis: Retrospective review of a 10-year single center experience and review of the literature. J Infect Public Health 13(11): 1705-1709.
- De la Peña Riverón E, Machín Rodríguez JC, Torralbas Reverón FE, De la Torre Fonseca CA, Martínez Muniz JO (2012) Predictors of mortality in aortic valve replacement. Oriental Network Cardiovascular Surgery Center, "Saturnino Lora Torres" Surgical Clinical Teaching Provincial Hospital, Santiago de Cuba, Cuba MEDISAN [internet] 16(10): 1504.
- Santangelo G, Rossi A, Toriello F, Badano LP, Messika Zeitoun D, et al. (2021) Diagnosis and Management of Aortic Valve Stenosis: The Role of Non-Invasive Imaging. J Clin Med 10(16): 3745.
- Christensen JL, Tan S, Chung HE, Ghosalkar DS, Qureshi R, et al. (2020) Aortic valve calcification predicts all-cause mortality independent of coronary calcification and severe stenosis. Atherosclerosis 307: 16-20.
- Kawsara A, Alqahtani F, Nkomo VT, Eleid MF, Pislaru SV, et al. (2021) Determinants of Morbidity and Mortality Associated with Isolated Tricuspid Valve Surgery. J Am Heart Assoc 10(2): e018417.
- Gammie JS, Chikwe J, Badhwar V, Thibault DP, Vemulapalli S, et al. (2018) Isolated mitral valve surgery: the society of thoracic surgeons’ adult cardiac surgery database analysis. Ann Thorac Surg 106(3): 716-727.
-
Alexander Valdés Martín, César Cáceres Roselio, Lidia María Rodríguez Nande, Nurys Bárbara Armas Rojas etc all. Complications and Predictors of Postoperative Mortality in Patients Undergoing Valve Replacement Surgery. On J Cardio Res & Rep. 6(4): 2022. OJCRR. MS.ID.000643.
-
Valvulopathies, Surgery, Mortality, Morbidity, Sepsis, Arrhythmias, Cardiac valve surgery, Myocardial protection, Echocardiography, Valvular heart disease, coronary artery disease, Arterial hypertension, Diabetes mellitus, Stroke, Chronic kidney disease, Chronic obstructive pulmonary disease, Pulmonary hypertension, Arrhythmias, Bronchial asthma
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






