 Case Report
Case Report
Complete Atrioventricular Block in a 22-Year-Old Woman: Case Report
Torres-Martel J1*, Valladares-Yañez C2, Sánchez-Guevara E3, Flores J4, Barrera-De Leon JC5, Garcia-Tejada BA6 and Begazo-Paredes JE7
1Professor, Faculty of Medicine, Autonomous University of Queretaro, Mexico
2University of the Valley of Mexico, Queretaro, Mexico
3Star Medica Hospital, Querétaro, Mexico
4General Zone Hospital of the Mexican Institute of Social Security (IMSS), Irapuato, México
5University Center for Health Sciences, University of Guadalajara, Maternal and Child Hospital Esperanza López Mateos, Jalisco Health Secretary, Mexico
6Goyeneche, Hospital III, Arequipa, Peru
7Yanahuara, Hospital III, Arequipa, Peru
Torres-Martel J, Professor, Faculty of Medicine, Autonomous University of Queretaro, Mexico.
Received Date: March 09, 2024; Published Date: March 25, 2024
Abstract
Complete atrioventricular block is a rare but significant heart condition in young adults and adolescents. We explain the case of a 22-year-old woman who presented with a complete AV block, analyzing the etiology, clinical presentation, diagnosis, and management of CAVB in this specific population.
Keywords:Bradycardia; Atrioventricular block; Pacemaker
Abbreviations:AV: Atrioventricular; CAVB: Congenital atrioventricular block; DDD: Dual chamber
Introduction
Complete atrioventricular block is a cardiac disorder in which electrical conduction between the atria and ventricles is completely interrupted, causing symptoms in most patients due to decreased or total absence of coordination of heartbeats, which can have significant consequences for cardiovascular health. Although complete AV block can affect people of all ages, in this article we will focus on its occurrence in young adults. The objective is to analyze and understand the underlying causes of this condition, which is essential for proper diagnosis, management, and prognosis in this population, and review of the literature.
Case Presentation
We present a case of a 22-year-old woman with no known chronic conditions. Among her important history, hepatitis A at 5 years without complications, she has 3 vaccinations for SARS-COV 2 and a second-degree family history of heart murmur in unspecified treatment without follow-up 5 years ago. During the questioning, the patient reported a flu-like condition accompanied by fever, headache, and recurrent stabbing chest pain. Subsequently, she impaired functional capacity, feeling faint and fatigued with basic activities of daily living. On physical examination, aortic ejection focus murmur, HR 50 bpm, the rest without significant findings.
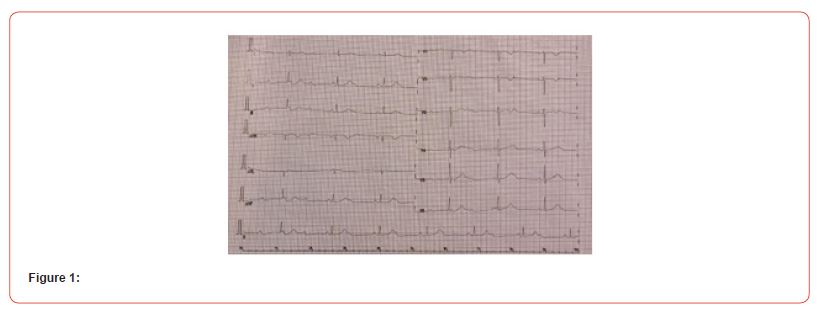
A transthoracic echocardiogram was requested, which reported acceleration in the aorta and a peak gradient of 20 mmHg. The electrocardiogram showed sinus rhythm, heart rate of 42 bpm, QRS axis at 67° with variable PR interval, corrected QT interval of 414 ms, ST segment with normal morphology, non-congruent P waves, QRS complex of 0.04s, demonstrating a complete atrioventricular block (Figure 1).
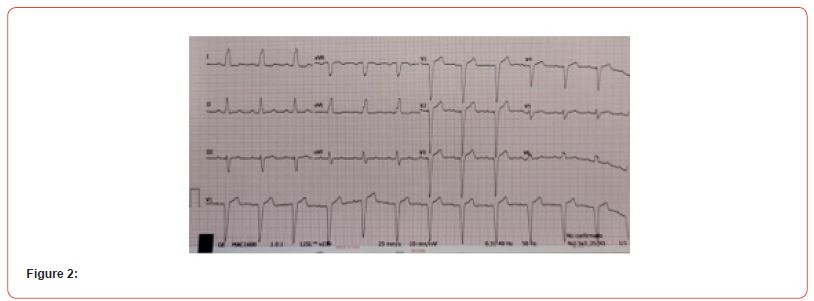
Management with a DDD pacemaker was decided, and the procedure was without complications. It remained monitored without presenting device failure. Two months after placement, the proper functioning of the pacemaker and total improvement of the symptoms were confirmed. Physical examination without alterations. A new echocardiogram and electrocardiogram without alterations were performed (Figure 2).
Discussion
Complete AV block in young adults can have various etiologies, from congenital anomalies to acquired diseases, intrinsic and extrinsic disorders, In the former there are direct alterations in the sinus node or the sinoatrial structure, the extrinsic refers to the use of cardiovascular drugs or systemic diseases. The main causes associated with this condition are congenital anomalies, sometimes people are born with malformations in the electrical conduction system of the heart that predispose them to complete AV block. These anomalies may include defects in electrical pathways or structural malformations of the heart such as transposition of the great arteries, single ventricle, and myocardial tumors. A large percentage lacks structural malformations and the defect is secondary to abnormal maternal isoimmunization with autoproduction of antinuclear anti-SSA/Ro and anti-SSB/La IgG antibodies, causing irreversible immunological damage in cardiac tissue. It is generally located superior to the His-Purkinje system, which is expressed electrocardiographically with a narrow QRS and a heart rate between 40 and 60 bpm. Autoimmune diseases, like systemic lupus erythematosus, manage to affect the electrical conduction system of the heart and cause complete AV block in young adults. Damage or inflammation of the myocardium, whether due to viral infections, inflammatory heart disease, or cardiomyopathies, can cause complete AV block in young adults. Cases of acute atrioventricular block after viral infections by SARS-CoV-2 have recently been reported, although the infection is dominated by respiratory symptoms, there are newcomers with primary symptoms of cardiovascular damage such as acute complete AV block in adults and young adults, with atypical manifestations. Beta blockers, calcium antagonists, and antiarrhythmic drugs interfere with the normal electrical conduction of the heart and can trigger complete AV block. Injury or trauma to the heart, from car accidents, sports injuries, or other causes, can cause complete AV block in young adults. Certain acquired factors are responsible for AV blocks, such as idiopathic progressive degeneration of the cardiac conduction system, progressive AV conduction disorders seen in neuromuscular diseases, systemic diseases such as amyloidosis, cardiac sarcoidosis, or neoplastic disorders. Lyme disease should be suspected as a possible cause of reversible AV block.
It is important to note that these are some of the most common causes of complete AV block in young adults and that each case may require individualized evaluation to determine the underlying cause. An accurate diagnosis will help guide the proper treatment and management of this condition in this population. The clinical presentation of a complete AV block can vary depending on the severity of the block and the presence of comorbidities. Bradycardia is one of the characteristic signs, it can be less than 60 bpm, and in some cases, it can be extremely low, especially in high-grade AV block. Fatigue and weakness, due to the slowing of the heart rate, generalized fatigue and weakness are experienced. Reduced blood flow and a lack of proper synchronization of the heartbeat affect the body’s ability to meet normal physical demands. Decreased cerebral blood flow due to bradycardia causes dizziness and fainting spells. These symptoms occur when a complete AV block occurs suddenly or during strenuous physical activities. Syncope, in more severe cases, especially when complete AV block is of sudden onset and occurs in young adults, vasovagal syncope may occur due to a lack of adequate blood supply to the brain for a prolonged period due to bradycardia. Chest pain or discomfort may be experienced due to decreased blood flow to the heart muscle. However, it is important to note that many patients with complete AV block are often asymptomatic.
Diagnosis is based on clinical evaluation and specific tests to confirm the presence and severity of the block. The diagnostic methods used are electrocardiogram, it is the fundamental tool for diagnosis. A lack of correlation is observed between the P waves and QRS complexes. This is evidenced by an absence of atrioventricular conduction in prolonged PR intervals or with the absence of a relationship between P waves and QRS complexes. Holter monitoring allows detection, evaluation of the frequency and duration of complete AV block episodes, especially in those cases in which the symptoms are not evident during a specific clinical evaluation. Stress tests may be performed to assess the heart’s response to exercise. These tests would reveal the presence of a complete AV block that only manifests itself during physical exertion. Echocardiography helps identify possible structural abnormalities of the conduction system or underlying diseases that may cause complete AV block. In some cases, especially when a specific etiology is suspected or when the block is of sudden onset in young adults, an invasive electrophysiological study is considered. This procedure uses catheters to map the electrical activity of the heart and assess the function of the conduction system.
A complete and thorough evaluation, including history, physical examination, and appropriate laboratory studies, is important to confirm the diagnosis of complete AV block and thus determine its underlying cause. The specialized medical team will determine what tests are necessary in each particular case.
Treatment of complete atrioventricular block is based on several factors, including the severity of symptoms, the presence of comorbidities, the age of the patient, and the underlying cause of the block. The most common and effective treatment for complete AV block, it restores the electrical conduction function of the heart by sending electrical impulses to regulate the heart’s rhythm. The type of pacemaker and its configuration are adapted to the individual needs of each patient. In less symptomatic cases, when implantation of a pacemaker is not possible or contraindicated, medications can be used to increase heart rate and improve conduction. Medications used include positive chronotropic agents, such as atropine or sympathomimetic agents. If the complete AV block is due to an underlying disease or condition, it is essential to treat and control that cause. This may include treatment of heart conditions, such as myocarditis or ischemic heart disease, or management of autoimmune or metabolic disorders. In specific cases, such as complete AV block refractory to medical therapy and pacemaker implantation, invasive interventions may be considered. These include atrioventricular node ablation or His bundle pacing, which involves placing electrodes at specific sites in the cardiac conduction system to restore normal conduction.
Treatment of complete AV block must be individualized according to the characteristics and needs of each patient. It is essential to have a specialized medical team and follow established clinical guidelines and recommendations.
The exceptionality of the case focuses on the type of patient, since in young people with the presence of bradycardia or low output, a differential diagnosis with complete atrioventricular block is not made. The previously healthy patient, with no history of cardiac, surgical, pharmacological, autoimmune, oncological, or structural malformations and having a sedentary life, causes of blockages that are observed in athletes or in congenital blocks are ruled out. In our patients, the presence of fatigue with ordinary activity led to the suspicion that it could have a cardiac origin. The electrocardiogram showed changes characteristic of a complete atrioventricular block. BAVC is a medical emergency, so its early identification and treatment determine a good prognosis.
Conclusion
Complete AV block is a rare finding in young individuals, all patients with cardiovascular symptoms must have an adequate assessment, with clinical review and electrocardiogram to be able to make an accurate diagnosis of cardiac conduction pathologies and be able to receive timely treatment.
Acknowledgement
None.
Conflict of Interest
The authors declare no conflict of interest.
References
- Chavan A, Mumtaz Z, Golangade R, Mahajan A, Nathani P (2021) Etiology of chronic atrioventricular block in young adults in a public university hospital in India. Indian Heart Journal 73(6): 754-756.
- Barra SNC, Providencia R, Paiva L, Nascimento J, Marques AL (2012) A review on advanced atrioventricular block in young or middle‐aged adults. Pacing and Clinical Electrophysiology 35(11): 1395-1405.
- Dideriksen JR, Christiansen MK, Johansen JB, Nielsen JC, Bundgaard H, et al. (2021) Long-term outcomes in young patients with atrioventricular block of unknown etiology. European Heart Journal 42(21): 2060-2068.
- Cortes-Ramírez JM, de Jesús Cortés-de JM, Cortés-de la Torre RA, Reyes-Méndez BJ, Salazar-de Santiago A, et al. (2013) congenital complete atrio ventricular block. Medicina Interna de México 29(6): 625-627.
- Hindi Z, Hindi Y, Batarseh R (2018) A rare case of complete heart block in a young patient. Case Reports in Cardiology 2018: 1493121.
- Yang YC, Pata RK, Aung TT (2018) A case of complete heart block with diagnostic challenge and therapeutic dilemma. Journal of Investigative Medicine High Impact Case Reports 6: 2324709618788110.
- Brotons DCA, Rotés AS, Gay LG, Mitjans AM Congenital atrioventricular block. the point of view of the pediatric cardiologist.
- Vallbona NB, Llopart JM, Burgui JM (2004) Asymptomatic third degree or complete atrioventricular block. Semergen: Spanish journal of family medicine (8): 414-416.
- López-Patiño HG, Serna-Posada MDM, Duque-González L, Uribe-Arango W, Duque-Ramírez M (2021) Syncope as a clinical manifestation of paroxysmal atrioventricular block and response to dual-chamber pacemaker implantation. CES Medicine 35(2): 156-164.
- Puga Bravo MV, Jimbo Jimbo AC, Gallardo Medina Y, Mora Orellana EJ, Puga Bravo EE (2018) Isolated complete atrioventricular block: a case report. Pediatric Rev electron pp: 23-28.
- Cabañas Morafraile J, Arcega Baraza A, Alarcón Escalonilla AI, Díaz Ríos R (2020) Third degree atrioventricular block: care and management in Primary Care. Clinical Journal of Family Medicine 13(3): 223-225.
- Toscano AMA, García LFP, Bermúdez CAH, Castro CSE (2021) Indications for the use of permanent pacemakers in atrioventricular block. Reciamuc 5(2): 36-44.
- Páez JLV, Villagomez MPM, Mogro EBI, Vasquez PAM (2020) Advanced atrioventricular block and extreme bradycardia as initial symptoms of Covid-19: case report.
-
Torres-Martel J*, Valladares-Yañez C, Sánchez-Guevara E, Flores J, Barrera-De Leon JC, Garcia-Tejada BA and Begazo-Paredes JE. Complete Atrioventricular Block in a 22-Year-Old Woman: Case Report. On J Cardio Res & Rep. 7(5): 2024. OJCRR.MS.ID.000671.
-
Cardiac conduction pathologies, Cardiac, Surgical, Pharmacological, Autoimmune, Oncological, Structural malformations, Sedentary life, Medical emergency, Atrioventricular, Chronotropic agents
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






