Mini Review
Mini Review
Bacterial Endocarditis A Brief Perspective
Júlia Souza Arraes1, Anne Gabrielle Fátima Rocha Coelho1, Nathalia Alves Vieira1, Yarla Resende Oliveira1, Laura Gomes Lima3 and Eriston Vieira Gomes1,2*
1Morgana Potrich College, FAMP, Medical School, Brazil
2Ribeirão Preto Medical School, FMRP, University of São Paulo, Brazil
3University of Rio Verde, Medical School, Brazil
Eriston Vieira Gomes, Department of Biofunctional, Morgana Potrich College, Mineiros, Brazil.
Received Date: May 29, 2020; Published Date: June 12, 2020
Abstract
Endocarditis is a cardiovascular condition that affects a small part of the population. It is characterized by affecting the internal membrane of the heart leading to inflammation, which may be caused by the accumulation of pathogenic microorganisms that may form microbial vegetation, reaching the heart valves. It is possible to diagnose the inflammation of the endocardium and prove the pathogenesis, which may be symptomatic or asymptomatic using the Duke criteria and the echocardiogram exam. Once diagnosed, a therapeutic approach is individualized, such as drug treatment using antibiotics, and/or in the case of major impairment of the cardiac organ, surgical intervention. However, there are some possible complications, such as neurological problems, intestinal pneumatosis, impairment of the prosthetic valve, and septic embolism, which may lead to death. Therefore, late diagnoses and treatment lead to a high mortality rate; therefore, an early and assertive diagnoses as well as an adequate treatment in accordance with the characteristics of each case are vital.
Keywords: Endocarditis; Bacterial infection; Heart disease; Endocardium; Heart valves
Abbreviations: IE: Infectious Endocarditis; BE: Bacterial Endocarditis; DNA: Deoxyribonucleic Acid; IPVE: Infectious Prosthetic Valve Endocarditis; SE: Septic Embolism
Introduction
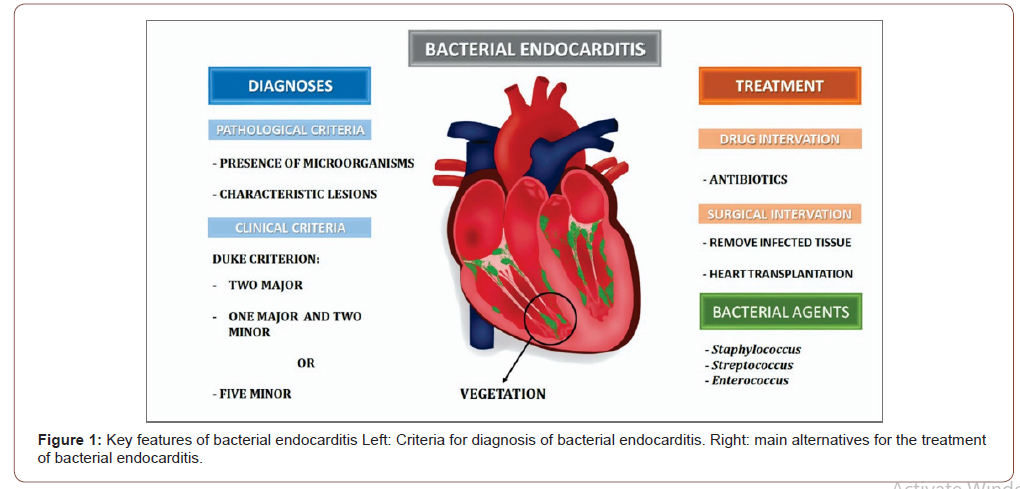
Endocarditis (inflammation of the endocardium) is a rare condition that may involve the heart valves [1]. It is classified according to primary causes into infectious and noninfectious endocarditis. Infectious endocarditis (IE) is the most common and severe cause of endocardium illness, with intracardiac vegetation formation as the main feature. The major causes of infection are bacterial agents such as Staphylococcus, Streptococcus, and Enterococcus [2]. Although it is an uncommon disease, its mortality rates are high due to its rapid evolution, late diagnosis, and inefficient treatment [3]. The present review aims to address and update the therapeutic methods and emphasize the importance of an early diagnosis for reducing the lethality and/or comorbidities of this serious disease.
Clinical Features and Diagnoses
The high risk of morbidity and mortality requires an early diagnosis to intervene with an appropriate and assertive treatment for endocarditis. Therefore, the pathology consists of an episode of systemic infection in which the endocardium is affected. Generally, the diagnosis is made using the DUKE criterion, which is divided into major criteria such as a positive blood culture and the evidence of endocardial involvement and minor criteria such as predisposition, fever, vascular and immunological phenomena, and microbiological and echocardiographic evidence. For the definitive diagnosis of IE, pathological criteria including the presence of microorganisms, characteristic lesions and clinical criteria must be included, which may be, two major, one major, and two minor, or five minor criteria [3-5]. The clinical manifestations related to the diagnosis are extremely important to highlight the pathophysiological mechanism, which is directly interconnected with the lesion in the endothelium, by altering the blood flow from laminar to the vortex. Consequently, activation of the coagulation cascade occurs to allow the adhesion of platelets, fibrin, and microorganisms, assuming the development of the inflammatory stage typical of the pathology in question [3, 6].
Treatment
The treatment for bacterial endocarditis (BE) must be individualized by analyzing the mechanisms of infection and the type of causative bacteria. The different forms of therapy are divided into two main methods: drug therapy and/or surgical intervention. Drug treatment is dependent on combating the microbial infection using antibiotics and controlling the growth of intracardiac vegetation, which is specific to the types of bacteria and used according to the risk factors [6]. This method is indicated for vulnerable patients such as with valve prostheses, with any type of congenital cyanotic heart disease and other conditions, individual who have undergone high-risk procedures such as the manipulation of the respiratory and genitourinary tracts, and invasive dental procedures with gingiva and perforation of the oral mucosa [2, 7]. Treatment through surgery is an option for approximately half of the patients with the disease, due to aggravating factors such as heart failure. Surgery can be chosen as an emergency (immediately) or as an urgency (within a seven-day interval), in cases of late diagnoses or inefficiency of antibiotics, progressing to a worsening of the condition. Surgical procedures achieve significant improvement, as they remove all infected tissues with large excisions, and reestablishing the heart’s completeness with valve replacement [8]. This type of treatment, when early, can prevent congestive heart failure, sepsis, and may even prevent embolism [9].
As a last option, heart transplantation should be chosen when antibiotic therapy is inefficient (Figure 1), due to resistant bacteria and when the surgical method does not yield significant results [6].
Complications
BE may trigger complications related to the proposed treatments [10]. Morbidity is a precursor to longer hospital stays, complementary cardiac surgery, and increased financial expenses. Various complications related to this disease have been reported, including infectious prosthetic valve endocarditis (IPVE), which often causes valve imbalance and unusability [11]. In addition, BE may cause neurological problems that affect approximately one-quarter of patients with the disease, and in most cases, asymptomatic lesions are detected [12]. However, in symptomatic lesions, the cerebral vascular accident (CVA) stands out because of its importance and severity, which is due to the displacement of the vegetation found in the intracardiac structures obstructing the intracranial arteries [13]. An additional complication caused by bacteria of the genus Enterococcus, which belongs to commensal flora, is intestinal pneumatosis. The most relevant traces are perivalvular prominences, leading to the perforation of the myocardium and valve aneurysms [14]. Another common and severe consequence is a septic embolism (SE). Septic emboli are usually formed by the aggregation of the thrombus and infectious material, which can be caused by hematogenous propagation, usually initiated in the heart valves. This phenomenon can manifest in any anatomical location and may also affect several organs, including the liver, spleen, and brain [15].
Conclusion
BE is a serious condition that can cause severe complications if not diagnosed and treated early. It leads to heart damage and difficulty in the pumping of blood, causing heart failure. This condition may cause damage to certain tissues, septic emboli, which are carried by the bloodstream to other organs, which can cause embolism and increase the risk of stroke, which are often fatal. However, in order to reduce the mortality rate, antibiotic therapy treatments are of paramount importance as a precaution for vulnerable patients such as those under high-risk procedures or emergency surgery for patients with late diagnoses. In addition, an understanding of the risk factors and the evolution of the disease is necessary for the prevention and early diagnosis, reducing damage and complications, and thus, improving the quality of life of the population affected by this serious disease.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Melo L, Duarte J, Roque D, de Oliveira IF, Faustino A, et al. (2017) Infectious Endocarditis: Sample from the Department of Internal Medicine of a Hospital. Internal Medicine 24 (1): 19-23.
- Teixeira J, Marques A (2019) Prophylaxis of Bacterial Endocarditis: State of the Art. Journal of the Portuguese Society of Anesthesiology 28(3): 174-180.
- Sobreiro D, Sampaio R, Siciliano R, Brazil C, Branco C, et al. (2018) Early Diagnosis and Treatment in Infective Endocarditis: Challenges for a Better Prognosis. Arquivos Brasileiros de Cardiologia 112(2): 201-203.
- Gutierrez P, Calderaro D, Caramelli B (2004) Infectious endocarditis. Magazine of the Brazilian Medical Association 50(2): 118-119.
- Madeira MP (2018) Profile of inpatients diagnosed with Infectious Endocarditis in the Internal Medicine service of a Tertiary Hospital in Ceará.
- Bravo DPL, Coelho APP, Dahia CB, Bicudo FB, Santos JEP (2018) Treatment of Infectious Endocarditis with Valve Replacement. Notebooks of Medicine-UNIFESO 1(1).
- Garrido RQ (2016) Risk factors for early infectious endocarditis of prosthetic valves: a case-control study.
- Lamas C (2020) Infective Endocarditis: Still a Deadly Disease. Brazilian Archives of Cardiology 114(1): 9-11.
- Galvao JLFM (2016) Endocarditis infection: a review of the microorganism for treatment.
- Marques A, Cruz I, Caldeira D, Alegria S, Gomes AC, et al. (2019) Risk Factors for In-Hospital Mortality in Infective Endocarditis. Brazilian Archives of Cardiology.
- Marti-Carvajal AJ, Dayer M, Conterno LO, Garay AGG, Marti-Amarista CE (2020) A comparison of different antibiotic regimens for the treatment of infective endocarditis. Cochrane Database Syst Rev (5).
- Sotero FD, Rosario M, Fonseca AC, Ferro JM (2019) Neurological complications of infective endocarditis. Curr Neurol Neurosci 19(5): 23.
- De goes Marques CR (2018) Infectious endocarditis as a risk factor for ischemic stroke: an integrative review. Research Week at Tiradentes University-SEMPESq (18).
- Mondragao A, Ramos AR, Barbedo M (2017) Infectious endocarditis as a risk factor for ischemic stroke. An integrative review 78(2): 73-75.
- Yellapu V, Ackerman D, Longo S, Stanislaw PS (2018) Septic embolism in endocarditis: Anatomic and pathophysiologic considerations. In Advanced Concepts in Endocarditis. IntechOpen 149.
-
Nathalia Alves Vieira, Yarla Resende Oliveira, Laura Gomes Lima, Eriston Vieira Gomes....etc al. Bacterial Endocarditis A Brief Perspective. On J Cardio Res & Rep. 4(2): 2020. OJCRR.MS.ID.000582.
-
Endocarditis, Bacterial infection, Heart disease, Endocardium, Heart valves, Intestinal pneumatosis, Prosthetic valve, Septic embolism, Predisposition, Fever, Vascular, Immunological phenomena, Microbiological, Echocardiographic evidence
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.