 Review Article
Review Article
A Comparison of Cardiac Ultrasound Instructional Methodologies in Undergraduate Medical Education
Pappanroop Sandhu*, Corey Young, Fauzia Nausheen and Jason Crowley
California University of Science and Medicine–School of Medicine, United States
Pappanroop Sandhu, California University of Science and Medicine–School of Medicine, United States.
Received Date:May 22, 2021; Published Date:June 10, 2021
Abstract
A growing part of medical education is ultrasound as it allows students to integrate basic sciences with the clinical. Recently, there has been an increasing effort among medical schools to integrate ultrasound technology into preclinical medical education. Many medical schools are developing POCUS (Point of Care Ultrasound) based ultrasound curriculums. The objective of this study was to determine the most effective method of teaching 1st year medical students cardiac anatomy and clinical skills through POCUS. We hypothesized that the best way of learning cardiac POCUS is by an in-person demonstration by a sonographer, when compared to watching video demonstrations. The participants included 20 1st-year medical students from the California University of Science and Medicine - School of Medicine (CUSM - SOM). Students were divided into two groups: video group and the in-person demonstration group. There were 10 students in each group. The participants had no previous experience with POCUS. Results showed that a more effective method of teaching 1st-year medical students cardiac POCUS is through in-person demonstrations, rather than watching online modules, as students in this group were better able to identify correct probe placement and heart chambers in short axis.
Keywords:Medical education; Ultrasonography; Point-of-care ultrasound
Introduction
Ultrasound is a growing part of medical education and is perceived as an enhancing modality to integrate basic medical education with the clinical sciences [1]. Recently, there has been an increasing effort among medical schools to integrate ultrasound technology into preclinical medical education [2, 3]. Many medical schools are developing POCUS (Point of Care Ultrasound) based ultrasound curriculums [4]. Some schools are still in the process of implementing POCUS programs using the multidisciplinary approach across the medical specialties. Areas that need to be focused on are the availability of the trained POCUS staff to provide the hands-on training and standard methods to evaluate the required ultrasound competencies and knowledge. A trained POCUS physician for different medical specialties is difficult to get for many medical schools.
Longitudinal experiences are considered to be the preferred methods for developing skills, attitudes, knowledge and behaviors as indicated in the competencies defined by the Accreditation Council for Graduate Medical Education (ACGME) [5]. The program that we offer at our medical school is based on a similar methodology of longitudinal experience during the system-based courses of the pre-clerkship curriculum. Since cardiac ultrasound is one of the required experiences in our ultrasound curriculum for medical students, students in year 1 are not expected to diagnose pathological conditions, but they are required to learn the proper techniques to image the heart. The most difficult part is the familiarity with echocardiography windows and 3-dimenional mental construct of the heart while looking at the 2-dimensional imaging. Most studies show that students perceive ultrasound as a very valuable learning and teaching tool to have an improved understanding of cardiac anatomy and physiology. The current study was also conducted as part of a longitudinal ultrasound experience during the last year 1 cardiovascular course [6,7]. The objective of this study was to determine the most effective method of teaching 1st-year medical students cardiac anatomy and clinical skills through POCUS. We hypothesized that the best way of learning cardiac POCUS is by an in-person demonstration by a sonographer when compared to watching video demonstrations.
Material and Method
The study was approved by the institutional review board and was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving human subjects. The participants included 20 1st-year medical students from the California University of Science and Medicine - School of Medicine (CUSM - SOM). Students were divided into two groups: video group and the in-person demonstration group. There were 10 students in each group. The participants had no previous experience with POCUS. The video group watched cardiac-ultrasound modules provided by the Society of Ultrasound in Medical Education (SUSME). A sonographer gave the in-person demonstration group a live POCUS demonstration. Afterward, the participants from each group were asked to obtain 3 cardiac ultrasound views on a simulated patient: long axis, short axis, and subcostal. They were asked to identify the particular anatomy of the heart. A 3-point grading scale was used by the sonographer to evaluate each participant’s ability. Statistical analysis was done using Student’s t-test, and a p-value < 0.05 was taken as significant. Additionally, both groups had to complete a 15 question quiz before and after their respective interventions. Each group was given 20 minutes to complete each quiz.
Result
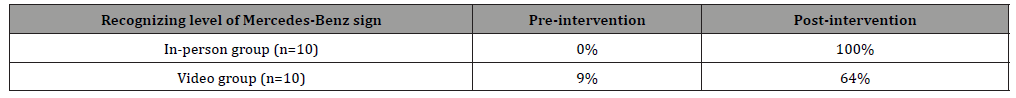
Our results showed that the in-person demonstration group was able to better identify the correct anatomical location for probe placement when compared to the video group (p < 0.05) (Figure 1). Additionally, the in-person demonstration group was able to better identify the heart chambers in a short axis view of the heart (p < 0.05) (Figure 1). There was no statistically significant difference between the groups when asked to identify the heart chambers in long axis view, aortic valve in the short axis view, mitral valve in the short axis view, and pericardium. A repeated measures ANOVA with a Greenhouse-Geisser correction determined the mean overall quiz scores for both groups differed from pre- to post-test (F(1,17) = 110.47, p < .05); however, there were no significant interaction effect between groups (F(1,17) = 2.754, p = .115) (Table 1). The same analysis was performed to determine mean differences for each question asked. When asked to identify the four levels of a short axis view of the heart, the pre-test to post-test change in the video group was 9% to 0% correct whereas correct answers in the in-person demonstration group improved from 25% to 88% correct (F(1,17) = 8.435 p = 0.01) (Table 2). When asked to recognize the level of Mercedes-Benz sign, the pre-test to post-test change in the video group was 9% to 64% correct, and in the inperson demonstration group was 0% to 100% correct (F(1,17) = 5.965, p = 0.03) (Table 3).

Table 1: 15 question multiple choice quiz results.
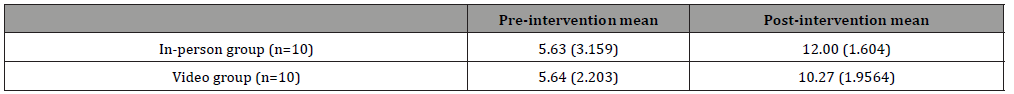
Table 2:Percentage of students correctly identifying 4 levels of cardiac short axis on quiz.
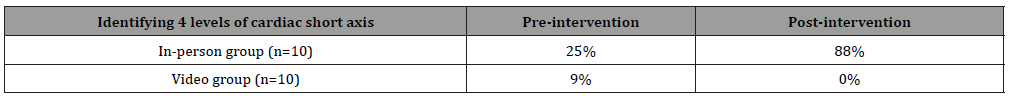
Table 3: Percentage of students correctly recognizing the level of the Mercedes-Benz on a quiz.
Discussion
There have been many ways to teach ultrasound knowledge and competencies. Some medical schools sometimes use hybrid courses for training their graduates. POCUS online courses mostly consist of structured modules of videos, cases, and quizzes. In our study, we also incorporated a similar type of online module taken from the society of ultrasound in medical education [8]. We compared the learning of participants with in-person teaching of the same content. At the end of the 2 strategies, the hands-on sessions were conducted, and retention of knowledge and attainment of skills compared. One reason that students lack the confidence to perform ultrasound is that most schools use hands-on training only without any pre-workshop training. Some schools exclusively use the online module and then conduct hands-on training that can also lead to some misconceptions. Our study was conducted to see which areas of knowledge are weak in the online module training that was compared with the hands-on training. Consistent with our study are many studies that show the benefits of hybrid courses and technologies. In a similar study, the clerkship students during their emergency medicine training received demonstration and training on human models and simulators. The results of the study were consistent with some aspects of our study. They concluded that in knowledge, the groups showed no difference, and both groups were equally comfortable with ultrasound skills of FAST examinations [9]. We found that there are some advantages of preparatory videos in gaining knowledge but confidence of placing the probes at the correct location is best learned with an in-person demonstration. Our study’s main focus was imaging the heart with ultrasound and testing heart anatomy knowledge on ultrasound by a short video and in-person intervention.
We followed the standard display of cardiac anatomy in the long and short axis, subxiphoid and apical views for the imaging of the heart. The anatomy of the heart on ultrasound imaging is somewhat confusing for medical students to interpret since the heart is positioned in the chest in many orthogonal planes. The probe’s position and orientation of heart images are different from traditional methods learned for ultrasound imaging. For imaging of the heart, the probes have to point to the right shoulder to get the long axis parasternal view and the left shoulder to get the view in the short parasternal axis. These difficulties in imaging the heart and placing the probe are best understood by in-person demonstrations [10].
A more effective method of teaching 1st-year medical students cardiac POCUS is through in-person demonstrations, rather than watching online modules, as students in this group were better able to identify correct probe placement and heart chambers in short axis. Thus, we believe the in-person teaching method to be the superior ultrasound teaching method. The results of this study will serve as evidence to create future ultrasound sessions at CUSM - SOM. Further studies can expand to other organ systems.
Acknowledgement
We’d like to acknowledge the many students, faculty, and support staff that made this study possible.
Conflict of Interest
No conflict of interest.
References
- Inoyat Jumayev, Pulat Usmanov, Shavkat Rustamov, Sherzod Zhurakulov (2020) Comparative inotropic effects of the some isoquinoline alkaloids. Biomedical and Pharmacology Journal 13(1): 325-333.
- Andrew A Grace, A John Camm (2000) Voltage-gated calcium-channels and antiarrhythmic drug action. Cardiovasc Res 45(1): 43-51.
- Gerald W Zamponi, Joerg Striessnig, Alexandra Koschak, Annette C Dolphin (2015) The Physiology, Pathology, and Pharmacology of Voltage-Gated Calcium Channels and Their Future Therapeutic Potential. Pharmacol Rev 67(4): 821-
- Ahmad Amin, Majid Maleki (2012) Positive inotropes in heart failure: a review article. Heart Asia 4(1): 16-
- Zhurakulov ShN, Levkovich MG, Vinogradova VI (2014) Synthesis of Hydroxyethyl Perivatives of 1-aryltetrahydroisoquinoline alkaloids. Chemistry of Natural Compounds 49: 1095-1098.
- Zhurakulov ShN, Vinogradova VI, Levkovich MG (2013) Synthesis of 1-aryltetrahydroisoquinoline alkaloids and their analogs. Chemistry of Natural Compounds 49: 70-74.
- Bo Sun, Jinhong Wei, Xiaowei Zhong, Wenting Guo, Jinjing Yao, et al. (2018) Alexander Vallmitjana, Raul Benitez, Leif Hove-Madsen, S R Wayne Chen. The cardiac ryanodine receptor, but not sarcoplasmic reticulum Ca 2+-ATPase, is a major determinant of Ca 2+ alternans in intact mouse hearts. J Biol Chem 293(35): 13650-13661.
- Åsmund T Røe, Michael Frisk, William E Louch (2015) Targeting Cardiomyocyte Ca2+ Homeostasis in Heart Failure. Curr Pharm Des 21(4): 431-
- Burkert Pieske, Melanie Sütterlin, Stephan Schmidt-Schweda, Kitzatomo Minami, Markus Meyer, et al. (1996) Diminished Post-Rest Potentiation of Contractile Force in Human Dilated Cardiomyopathy. J Clin Invest 98(3): 764-776.
-
Pappanroop Sandhu, Corey Young, Fauzia Nausheen, Jason Crowley. A Comparison of Cardiac Ultrasound Instructional Methodologies in Undergraduate Medical Education. On J Cardio Res & Rep. 5(3): 2021. OJCRR.MS.ID.000612.
-
Medical education, Ultrasonography, Point-of-care ultrasound, Cardiac anatomy, Echocardiography, Physiology, Heart chambers, Pathological conditions, Cardiac POCUS
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






