 Case Report
Case Report
“Wellens Syndrome” an Underdiagnosed and Potentially Catastrophic Entity. Regarding a Case
Perez-Arias Fidel Alejandro1*, Figueroa-Garcia Omar Isaac1, Galicia-Gutierrez Axel Noe1, Machain-Gonzalez David Alejandro2, Aviles-Lucero Emilio1, Acosta-Romero Ernesto3, Navarro-Gomez David3
1Universidad de Guadalajara, Centro Universitario de Ciencias de la Salud, Mexico
2Universidad de Guadalajara, Centro Universitario de Tonalá, Mexico
3Instituto Méxicano del Seguro Social, Hospital General Regional No 46, Mexico
Fidel Alejandro Perez Arias, Universidad de Guadalajara, Centro Universitario de Ciencias de la Salud, Mexico
Received Date:June 24, 2025; Published Date:July 01, 2025
Abstract
Wellens syndrome (WS) or left anterior descending artery (LAD) T wave inversion syndrome is a cardiological entity first described in 1982 by Wellens and Zwaan1 in patients with unstable angina and critical stenosis of the LAD, which corresponds to a subtype of unstable angina with a high risk of progressing to acute myocardial infarction of the anterior face. Characterized by the presence of inverted or biphasic T waves in the right precordial leads. These findings predict with high sensitivity and specificity the involvement of the proximal portion of the anterior descending artery, requiring an early invasive strategy in order to avoid its complications.
Keywords:NSTEMI; anterior wall myocardial infarction; wellens’ syndrome; electrocardiography; electrocardiography abnormalities.
Introduction
Wellens Syndrome (WS) is a cardiological entity clinically identified as a subtype of unstable angina, resulting from critical stenosis of the left anterior descending artery (LAD), which carries a high risk of progression to acute myocardial infarction (AMI). It is characterized by an electrocardiographic pattern of T-wave inversion in the precordial leads [1]. Early identification allows for an optimal diagnostic and therapeutic approach to prevent progression to its most feared outcome, AMI. We present the case of a male patient with significant medical history, who sought care due to an episode of chest pain likely of cardiac origin. He underwent a diagnostic work-up, including an electrocardiogram that revealed findings compatible with type B WS. A blood sample was taken for cardiac biomarker testing to rule out acute myocardial infarction, and the diagnosis of WS was integrated based on these findings, further confirmed by evidence of occlusion on coronary angiography. This clinical case follows the CARE guidelines.
Case Presentation
A 74-year-old male patient with high cardiovascular risk (ASCVD 16.1%, Framingham 11%), with systemic arterial hypertension under control according to ESH 2021 guidelines, and a 3-month history of unstable angina classified as NYHA class III, managed with antianginal and cardioprotective medications. He presented with chest pain of probable cardiac origin, with 4 hours of evolution. Thirty-six hours prior to admission, he experienced a similar episode. On physical examination: blood pressure 115/78 mmHg, heart rate 65 bpm, respiratory rate 17 bpm, oxygen saturation 94% on room air. No jugular vein distention, hepatojugular reflux, or pulmonary crackles were present. No S3 gallop or added murmurs were detected.
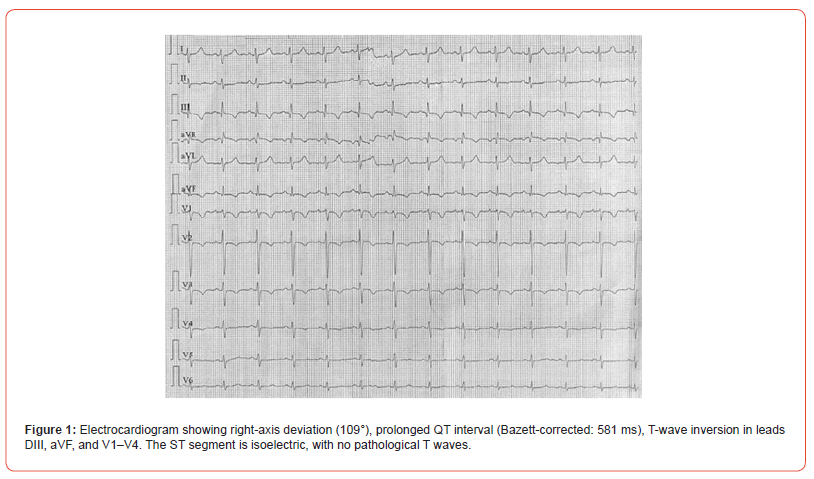
An electrocardiogram (ECG) was performed, showing T-wave inversion in leads DIII, aVF, and V1–V4, along with a Troponin I level of 21.4 ng/L, with no delta change on follow-up tests. Based on these findings, type B Wellens Syndrome was diagnosed. Antiplatelet, anticoagulant, lipid-lowering, and antianginal treatment was initiated. The patient was subsequently prepared for referral to a tertiary care center, with no further chest pain episodes or anginal equivalents reported [1].
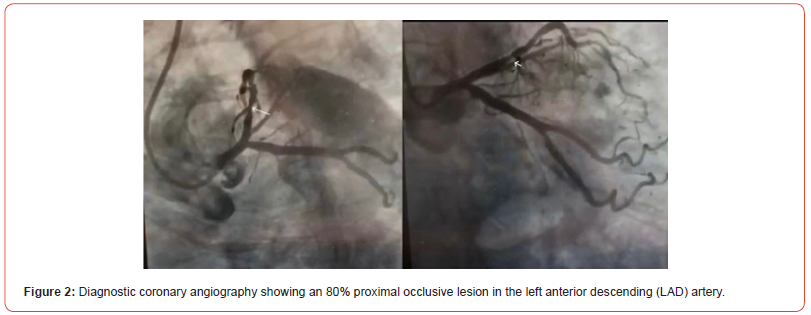
Subsequently, the patient was admitted to our unit and underwent diagnostic coronary angiography, which reported the following findings: Left main coronary artery: no angiographic lesions; Left anterior descending artery (LAD): 80% proximal stenosis, remainder without lesions, diagonal branches without lesions; Circumflex artery and distal branches: no lesions; Right coronary artery: dominant and without lesions; Posterior descending artery: no lesions. A 30x33 mm Ultimaster stent was placed at the site of the lesion, and the proximal segment was optimized with a 3.5x15 mm balloon. Follow-up angiography showed TIMI flow grade 3 and myocardial perfusion grade TMP 3. The patient remained under hemodynamic monitoring without complications. He had a favorable post-procedural course with no clinical repercussions and was discharged after five days. Upon discharge, he was prescribed dual antiplatelet therapy, dual lipidlowering therapy, an ACE inhibitor, a beta-blocker, and an SGLT2 inhibitor (Figures 1&2).
Discussion
Wellens Syndrome (WS) is an uncommon cardiological entity, accounting for only 5.7% of patients with acute coronary syndrome (ACS) [2]. However, it holds significant clinical importance due to its strong correlation with critical stenosis of the left anterior descending artery (LAD), representing a pre-infarction state that may precede an extensive acute myocardial infarction. Timely recognition by the first-contact physician is therefore essential to initiate early management and improve patient outcomes. Its diagnosis is primarily electrocardiographic, characterized by biphasic T waves in leads V2-V3 (type A) or deeply inverted T waves in leads V2-V4 (type B), both patterns occurring in the absence of ST-segment elevation or significant elevation of myocardial necrosis biomarkers [3]. The presented patient was diagnosed with type B Wellens Syndrome, characterized by symmetrical T-wave inversion in the precordial leads. His initial evaluation included an ECG with findings consistent with this entity, and troponin levels were slightly elevated but showed no rise in serial measurements, aligning with the classical description of Wellens Syndrome. Early identification of Wellens Syndrome (WS) is crucial due to the high risk of progression to extensive myocardial infarction if timely intervention is not performed [4]. Compared to other acute coronary syndromes, WS does not present with ST-segment elevation, which may lead to underestimation if a detailed ECG evaluation is not conducted. Unlike other ischemic patterns, the characteristic T waves in WS indicate critical occlusion of the LAD, with a specificity of 96.2% and a sensitivity of 24.6% [5].
Therefore, clinical suspicion and prompt electrocardiographic recognition are of vital importance. The treatment of WS differs from that of other non-ST-elevation acute coronary syndromes, as exclusive medical therapy without early invasive intervention may result in total LAD occlusion, with catastrophic consequences for the myocardium. Thus, the treatment of choice is early percutaneous coronary intervention. In this case, the adopted strategy included the administration of antiplatelet agents, anticoagulants, lipid-lowering drugs, and antianginal therapy, followed by diagnostic coronary angiography, which identified a significant 80% proximal LAD stenosis, confirming the high risk of progression to extensive anterior infarction. Angioplasty with stent placement was performed as definitive treatment, with subsequent optimization of coronary flow documented by TIMI 3 / TMP 3 flow grades, indicating successful revascularization without immediate complications⁶. Dual antiplatelet therapy, along with intensive lipid-lowering treatment and modification of risk factors, are key pillars in the prevention of recurrent cardiovascular events in this type of patient [6].
Conclusion
Early identification of Wellens Syndrome is essential due to its prognostic significance. This syndrome strongly indicates critical stenosis - primarily of the left anterior descending (LAD) artery - which highlights the importance of early detection. Lack of timely management exposes patients to the risk of developing a large anterior wall myocardial infarction. Moreover, this case underscores the crucial role of timely, multidisciplinary, and stepwise medical care, as well as the impact of combined pharmacological therapy and coronary intervention in preventing major cardiovascular events. Therefore, Wellens Syndrome should be regarded as a diagnostic emergency within the spectrum of non-ST-elevation acute coronary syndromes, requiring close monitoring, prompt angiographic evaluation, and timely invasive treatment to alter the natural course of the disease and significantly improve patient prognosis.
Financing and Conflicts of Interest
This study did not receive any funding from public or commercial sources.
Informed Consent
The patient referenced in this article provided informed consent for the case to be shared, after being thoroughly informed about the publication.
Contribution Statement
All authors contributed equally to the production of this article according to the CRediT taxonomy.
References
- De Zwaan C, Bär FW, Wellens HJ (1982) Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J 103(4): 730-736.
- Zhou L, Gong X, Dong T, Cui HH, Chen H, et al. (2022) Wellens' syndrome: incidence, characteristics, and long-term clinical outcomes. BMC Cardiovasc Disord 22(1): 176.
- Okobi OE, Bakare IO, Evbayekha EO, Olawoye A, Umeh CC, et al. (2022) Wellens Syndrome: A Possible Precursor. Cureus 14(11): e31963.
- Avram A, Chioncel V, Iancu A, Guberna S, Cuciureanu I, et al. (2021) Wellens Sign: Monography and Single Center Experience. Maedica (Bucur) 16(2): 216-222.
- Kobayashi A, Misumida N, Aoi S, Kanei Y (2019) Prevalence and Clinical Implication of Wellens' Sign in Patients With Non-ST-Segment Elevation Myocardial Infarction. Cardiol Res 10(3): 135-141.
- Zhou L, Gong X, Chen H, Dong T, Cui H, et al. (2023) Characteristics of Wellens’ syndrome in the current PCI era: a single-center retrospective study. Emerg Med Int 2023: 8865553.
-
Perez-Arias Fidel Alejandro*, Figueroa-Garcia Omar Isaac, Galicia-Gutierrez Axel Noe, Machain- Gonzalez David Alejandro, Aviles-Lucero Emilio, Acosta-Romero Ernesto, Navarro-Gomez David. “Wellens Syndrome” an Underdiagnosed and Potentially Catastrophic Entity. Regarding a Case. On J Cardio Res & Rep. 8(1): 2025. OJCRR.MS.ID.000679.
-
NSTEMI; anterior wall myocardial infarction; wellens' syndrome; electrocardiography; electrocardiography abnormalities; iris publishers; iris publishers’ group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
- Abstract
- Introduction
- Precision Lifestyle Medicine: AI-Guided WFPBD Care
- AI in Interventional Cardiology: Procedural Precision through Data
- Clinical Decision-Making and Medicolegal Protection
- Future Directions: The Road Ahead for AI in Cardiology
- Conclusion
- Author Contributions
- Funding
- Institutional Review Board Statement
- Informed Consent Statement
- Data Availability Statement
- Conflict of Interest
- References






