 Research Article
Research Article
Feasibility of Pharmacoinvasive Strategy in ST Segment Elevation Myocardial Infarction STEMI in the Tunisian Context: Monocentric Experience
Hichem Denguir1,2*, Mohamed Derwiche1,2, Slim Abidi1,2, Saher Gmiha1,2, Marouene Haloui1,3, Ahmed Elbatrawi1,3 and Marouene Gorii1,3
1Cardiology Department, CHU, Gabes, Tunisia
2Faculty of medicine of Sfax, Tunisia
3Faculty of Medicine of Monastir, Tunisia
Hichem Denguir, Associate professor in Cardiology, Faculty of Medicine of Sfax, Tunisia.
Received Date:June 01, 2023; Published Date:June 14, 2023
Abstract
Background:ST Elevate Myocardial Infarction (STEMI) is a serious pathology that requires rapid and effective coronary reperfusion. Current guidelines recommend primary angioplasty (PAMI) as the first-line strategy. However, this requires the availability of a functional cath lab 24 hours a day, 7 days a week and an access time of less than 120 minutes, which is not always possible. Apart from these conditions, the pharmaco-invasive strategy (PIs) remains an effective alternative to consider. We chose to evaluate the two reperfusion strategies in our Tunisian context.
Methods:In a case control study, we assigned all patients with STEMI presenting within 12 hours of onset of symptoms and having undergone coronary angiogram during their initial hospitalization at the University Hospital of Gabes (southeastern Tunisia), from September 2019 to September 2021.
Conclusions: In our Tunisian context, the short and midterm clinical outcomes are comparable for the two reperfusion strategies in STEMI. The PIs strategy is associated with a significant reduction in ischemic time and a tendency to reduce the occurrence of heart failure compared to the primary angioplasty.
Keywords:ST elevated myocardial infarction; Therapy; Thrombolysis; Angioplasty; Outcomes; Mortality
Abbreviations:CAD: Coronary Artery Disease; CKD: Chronic Kidney Disease; EMS: Emergency Medical Assistance Service; IQR: Interquartile Range; LAD: Left Anterior Descending Artery; LVEF: Left Ventricular Ejection Fraction; MACE: Major Adverse Cardiovascular Events; MI: Myocardial Infarction; NSTEMI: Non-ST-Elevation Myocardial Infarction; PAMI: Primary Angioplasty in Myocardial Infarction; PCI: Percutaneous Coronary Intervention; PIs: Pharmaco-Invasive Strategy; STEMI: ST-Segment Elevation Myocardial Infarction; TIMI: Thrombolysis in Myocardial Infarction
Introduction
ST-segment elevation myocardial infarction (STEMI) is a life-threatening condition. It requires urgent, complex and wellcoordinated treatment. Although the main goal of treatment is simple to describe “reperfusion as quickly as possible to restore coronary patency”, the process remains complicated, and dependent on several technical, logistical and geographical factors [1, 2]. Current guidelines recommend angioplasty as the first-line strategy. However, the mechanical reperfusion strategy requires the availability of a functional cath lab 24 hours a day, 7 days a week and an access time of less than 120 minutes, which is not always obvious [3]. Apart from these conditions, thrombolysis and immediate medical transfer to an interventional cardiology center remains an effective alternative to consider [3].
The modality of pharmaco-invasive therapy consists of early reperfusion by fibrinolysis and transfer to an interventional center which provides salvage angioplasty or routine coronary angiography in the event of successful lysis. This strategy has gained more interest in recent years in cardiology departments which do not have the possibility of performing coronary angioplasty 24 hours a day, for lack of personnel or the appropriate technical platform, knowing that the immediate prognosis and the medium term of the two strategies is identical according to the latest studies [4,5]. These two reperfusion strategies are well applied in Tunisia, the choice of one or the other depends on the conditions of each center and each logistical context. To date, no study
evaluating the results of the two strategies has been conducted in Tunisia. To assess the effectiveness of our practices, we decided to conduct this study comparing the immediate success rate and the immediate and mid-term outcomes of these two reperfusion strategies.
Methods
We carried out a monocentric, case-control, descriptive and analytical study during a period of 2 years between September 2019 and September 2021 in the Mohamed Sassi University Hospital Center of Gabes in the South-East of Tunisia. Patients were included using the “Cardioreport” software and the corresponding patient files.
We included all STEMI patients who underwent primary angioplasty or fibrinolytic treatment with Tenecteplase followed by coronary angiogram during the same hospitalization. We excluded all patients with no reperfusion treatment during the first 12 hours of progression and those with only fibrinolysis protocol. We collected epidemiological data, cardiovascular risk factors, clinical and angiographic data. The study population was then divided into two groups according to the reperfusion strategy adopted.
The primary endpoints were the immediate success rate defined by (a final TIMI III flow, a residual stenosis < 30%, the absence of images of dissection at the ends of the stent and the absence of images of thrombus), hospital mortality and the occurrence of early (< 1 month) major cardiovascular events (MACE) including death, non-elevated ST segment elevation myocardial infarction (NSTEMI), rehospitalisation for heart failure, stroke and hemorrhagic events). The secondary endpoints were the amount of the left ventricular ejection fraction (LVEF) at discharge from hospital, one-year deaths and one-year occurrences of MACE..
Statistic study
The data was entered and analyzed by SPSS 23.0 software, which made it possible to carry out all the statistical analyses. We carried out a descriptive study of the total population and of the two PAMI and PIs subgroups by describing the clinical, paraclinical and therapeutic characteristics as well as the evolution during hospitalization and during follow-up. Continuous data were presented as mean and standard deviation while categorical variables were presented as numbers and percentages. The comparison of the percentages on independent series was carried out by the Pearson chi 2 test and the comparison of the continuous data was carried out by the Student test. Survival curves were constructed using Kaplan-Meier estimates and compared using the log-rank test. We set the date of the ischemic event as the original date. In all statistical tests, the significance level was set at 0.05.
Results
The study population
During the period of our study, 201 patients were hospitalized for management of an STEMI (26 patients/100,000 inhabitants/ year). Among which: 121 patients had an evolution < 12 hours at the time of diagnosis; 15 patients had thrombolysis alone or were transferred to another angioplasty center; 3 patients with lost or with incomplete records. Only 103 patients met the inclusion criteria (Figure 1).
Study groups
Our population is divided into two groups according to the reperfusion strategy adopted. The first group of 28 patients, or 27.1% of patients, were repercussed by primary angioplasty (PAMI group). The second group of 75 patients 72.8% of patients received fibrinolytic treatment with Tenecteplase followed by angiography as part of a pharmaco-invasive strategy (PIs group) (Figure 1).
The demographic and clinical characteristics of the population
The average age of our population was 60.8 years with a male predominance 79%, 51.4% were diabetic, 55% smokers, 35% hypertensive with no significant difference between the two groups (Table 1).
Primary endpoints Immediate success
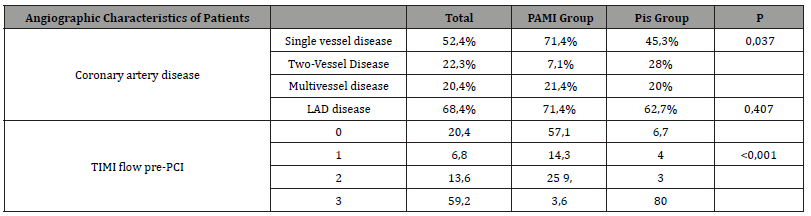
The angiographic success of the procedure was around 85.7% of cases in the PAMI group and 94.7% of cases in the PIs group, with no significant difference between the two groups (p=0.131) (Table 2). Clinical success was observed in 24 patients in the PAMI group (85.7%) and 70 patients in the PIs group (93.3%), with no difference between the two groups (p = 0.223).
Table 1:Epidemiological and clinical characteristics and the burden of cardiovascular diseases, diabetes mellitus, liver cirrhosis and MS predictors groups 1 and 2 of countries differing (Manna Whitney U-criterion).
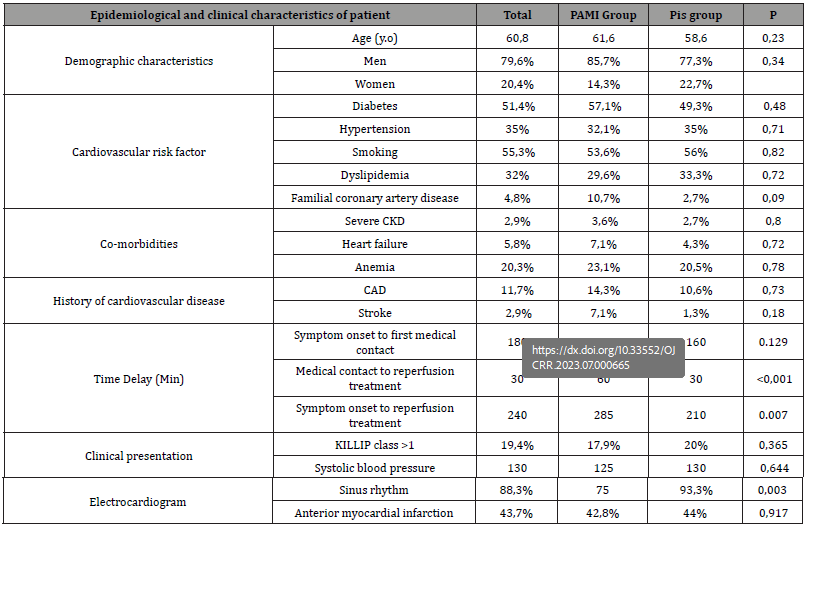
Table 2:Angiographic characteristics.
Early results
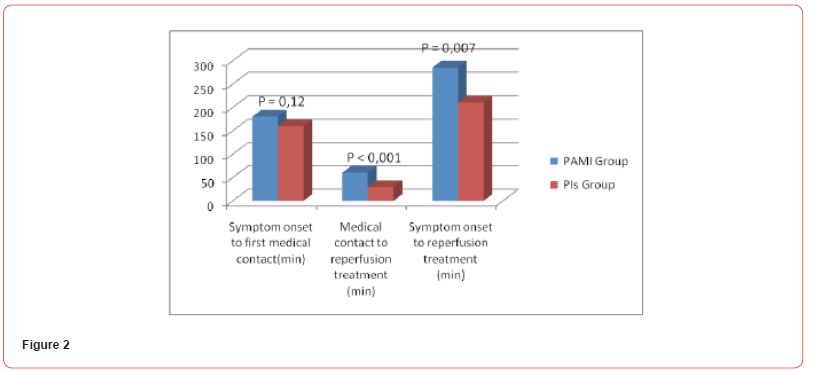
The mean time between the onset of symptoms and the first medical contact is 160 min [IQR: 110-300 min] in the PIs group and 180 min [IQR: 180-405 min] in the PAMI group with a p =0.129. The mean reperfusion time is 30 min [IQR: 10-30 min] in the PIs group and 60 min [IQR: 60-120 min] in the PAMI group with a p < 0.001.
The mean ischemic time is 210 min [IQR: 120-330 min] in the PIs group and 285 min [IQR: 217-540 min] in the PAMI group with p = 0.007 (Figure 2).
In intra-hospital we found no significant difference in terms of mortality: 5 deaths; 3.6% in the PAMI group and 5.3% in the Pis group p=0.711. Same for major events; 17 cases of heart failure 17.9% vs 16%, P= 0.8, NSTEMI in 1 case, 0% vs 1.3%, p=0.1, one case of major bleeding 3.6% vs 0%, P=0.1 and 7 cases of cardiogenic shock 7.1% vs 6.7%, p=0.9. For combined MACE no significant difference between the two groups at thirty days; 21.4% for the PAMI group vs 16% for the Pis group, P=0.5. The median hospital stay was 5 days, [IQR: 3 - 6 days]. in the PIs group; and 4 days, [IQR: 3-5] and in the PAMI group; p = 0.526.
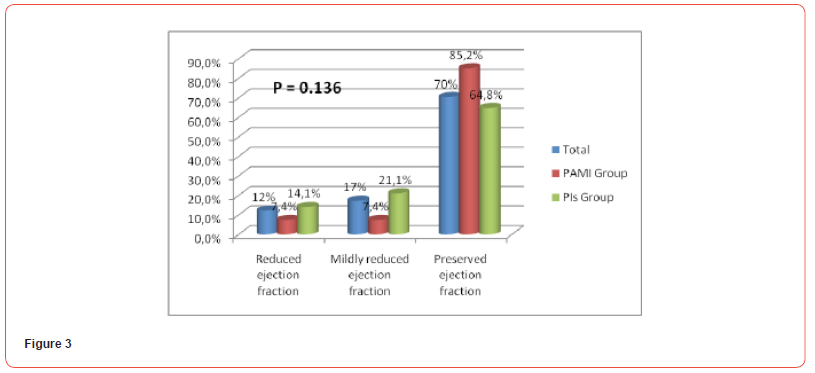
Secondary endpoints Cardiac function at discharge
The echocardiographic study of LVEF before discharge from hospital was comparable in the two groups with no significant difference (average LVEF 55% vs 55%; p = 0.123) (Figure 3).
One-year results
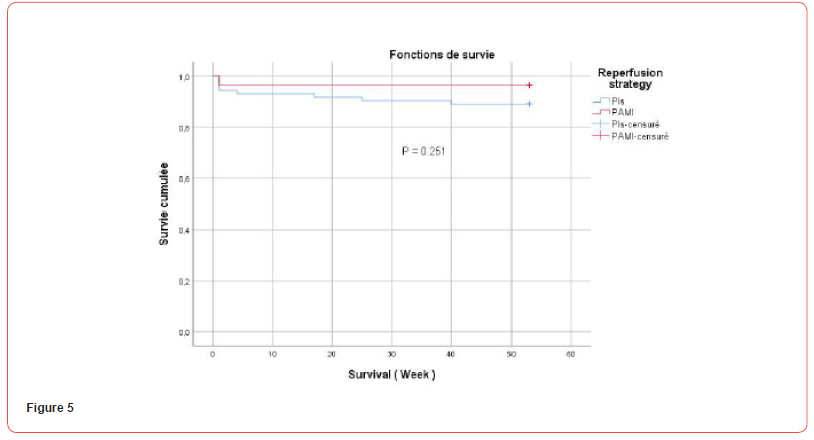
At one year of follow-up, we did not note any significant difference in terms of Mortality: 9 deaths; 3.6% in the PAMI group and 11% in the Pis group p=0.24. The same for major events 14 cases of heart failure, 14.3% vs 13.7%, P= 0.9, NSTEMI in 2 cases, 0% vs 2.7%, p=0.37, one case of major bleeding 3.6% vs 0%, P=0.1 and 1 case of ischemic stroke 0% vs 1.4%, p=0.54. For combined MACE no significant difference between the two groups at 12 months of follow-up; 21.4% for the PAMI group vs 21.9% for the Pis group, P=0.47. There was no difference in terms of survival at one year or survival without occurrence of MACE between the two groups as represented by the survival curves according to the Kaplan Meier method (Figures 4 & 5).

Discussion
The treatment of the STEMI aims to restore the patency of occluded coronary artery responsible for the MI as quickly and durably as possible. Two methods are recognized: intravenous fibrinolysis and primary angioplasty. The choice of strategy depends on the availability of an invasive technical platform, the patient presentation times and the possibility of rapid medical transfer to an interventional cardiology center. This choice should be discussed at the level of each institution initially, then at the regional level involvement of EMS (Emergency medical assistance service) teams, on-call schedule of interventional cardiologists and paramedical staff working in public or private structures). Percutaneous coronary intervention appears to be superior to thrombolysis. However, this requires immediate transfer to an experienced response center, which often poses logistical problems and waste of time.
Fibrinolytic therapy has a significantly greater beneficial effect in patients presenting within 2 hours of symptom onset [1]. This suggests the importance of prehospital thrombolysis in reducing mortality [2]. A pharmaco-invasive strategy can be defined as pharmacological reperfusion (using fibrinolytic agents) with “invasive back-up”, which means that patients are transferred to an interventional cardiology center for either angioplasty of immediate rescue in the event of failure of fibrinolysis, or nonemergency coronary angiography to determine the need for additional treatment of the culprit lesion (angioplasty or bypass) [3].
This strategy proved to be superior to a very conservative approach of hospital fibrinolysis with transfer to an angioplasty center only in the event of failure of thrombolysis. The NORDI-STEMI study and the TRASFR-in-AMI study showed a significant reduction in ischemic events at 30 days and 1 year for patients with rapid transfer to an angioplasty center compared to the conservative approach [4, 5]. In this study we evaluated this strategy compared to primary angioplasty in our local conditions. We found no difference in short- and mid-term clinical outcomes between STEMI patients treated with primary angioplasty (PAMI) or pharmaco-invasive strategy (PIs). This can be attributed to the short delay between the onset of ischemia and reperfusion observed in the PIs group.
This is the first study on this subject in Tunisia, in which we focused on practices in regions with difficult access to cath lab. Our past national data shows that 61.8% of STEMI patients receive reperfusion therapy: 30% with primary angioplasty and 31.8% with intravenous fibrinolysis. Nearly a third of patients receive no reperfusion treatment and the majority of them in regional hospitals (52.9% of STEMI patients in regional hospitals remain without reperfusion treatment) [6]. As observed in previous national studies, diabetes is the most frequently reported cardiovascular risk factor [6]. In addition, as in the (TRANSFER-AMI) study [5], anterior location and Killip-Kimball stage I were the main forms of presentation in the present study. The average age of patients undergoing PAMI was similar to those undergoing PIs, this decision was encouraged by the results of the STREAM study with the reduction of doses of Tenecteplase for patients over 75 years of age [7]. We noted only one case of major bleeding, in the PAMI group.
Time from symptom onset to First medical contact and time to reperfusion were significantly shorter in the PIs group. This result is consistent with the results of the French registry of acute myocardial infarction with and without ST segment elevation (FAST-MI) [8] which included 1714 patients, where the median reperfusion time was 130 min for the group PIs and 300 min for the PAMI group, with no difference in mortality after 1 to 5 years of follow-up [9]. In the FAST MI Tunisia national register, the ischemia time was 180 min for the fibrinolysis group and 360 min for the PAMI group. These are longer durations than those recommended by international guideline goals [10,11], which may be explained by failures in rapid diagnosis, lack of access to fibrinolytic agents, traffic conditions or geography, the absence of EMS in certain regions, the overload of emergency services and the scarcity of centers with a functional cath lab 24 hours a day, 7 days a week. All these limitations suggest and support the hypothesis that PIs could be considered the most timely and feasible option for the majority of patients in Tunisia.
In our study, the time to thrombolysis was significantly faster than the time to primary angioplasty, which could decrease the benefit of primary angioplasty compared to thrombolysis in our local conditions. The results of the occurrence of complications in the STREAM study were proportional to the time to angioplasty ≤ 55 min, > 55-97 min and > 97 min. The endpoint occurred in the IP and PAMI arm in 10.6 % versus 10.3% (≤55 min, p=0.910); 13.9% versus 17.9% (>55-97 min, p=0.148) and 13.5% versus 16.2% (>97 min, p=0.470), respectively. Although there was no worsening of outcomes in the PIs arm, it did occur in the PAMI arm (p (trends) = 0.038) [12]. The PIs group exhibited greater patency of the culprit artery at baseline angiography which could lead (assuming there is more previously salvaged myocardium) to clinical benefits during follow-up. Moreover, higher success rates (TIMI flow 3) after angioplasty were obtained in the PIs group, which could have an impact on the reduction of mortality. Previous studies had already reported that the degree of TIMI coronary flow after the procedure is independently correlated with mortality in the year following myocardial infarction [13].
These results are similar to those in the study (STREAM), where the final TIMI 3 flow rate was lower in patients who underwent PAMI and salvage angioplasty than in patients who underwent scheduled angiography (within 6 to 24 hours) [14]. These results are similar to those of a study conducted during the pandemic in China [15] reporting that patients who underwent fibrinolysis combined with delayed angioplasty (within the first 24 h) had better TIMI flow after the procedure than those who underwent undergone PAMI, with a similar rate of in-hospital adverse events. These results can be explained by two phenomena the first is a probable effect of thrombolysis which reduces the thrombotic load thus improving the result of coronary angioplasty. Secondly, it is the choice of the invasive strategy from the outset for certain patients considered to be at higher risk for a PIs strategy. Other previous studies [9, 16-18] have described similar safety and efficacy of the two PI strategies and PAMIs in terms of mortality and morbidity. Bainey, et al. [19] observed better outcomes with PIs and similar rates of major bleeding in the Canadian study.
These reports indicate that PIs are an appropriate and reasonable alternative, with similar results to PAMI, especially for countries where access to PAMI is limited. In our study, the two strategies showed no difference in hospital mortality, cardiovascular mortality and cardiovascular events. However, we noted a trend towards a reduction in the occurrence rate of post-infarction heart failure in the PIs group. This leads to the conclusion that the longer delay in PAMI reperfusion worse the outcome [1, 10]. Other studies have even observed that fibrinolysis was associated with a decrease in one-year mortality in early presenters [20]. Additionally, a metaanalysis of patients in hospitals without access to PAMI found that early reperfusion in the PIs group significantly reduced short-term mortality compared to the PAMI group with 200 or more minutes from symptom onset to reperfusion [21].
Solhpour, in 2016 compared the effect on LVEF of prehospital thrombolysis with urgent angioplasty versus primary angioplasty as a function of ischemia time. This study found that in STEMI patients with ischemia time <180 minutes, a pharmaco-invasive strategy can reduce myocardial scar size compared to primary angioplasty. And for an ischemia time ≥180 minutes, the size of the myocardial scars was equivalent in the two groups [22].
In our population, the LVEF is comparable in the two groups. Indeed, the prolonged ischemia time in our study attenuated the beneficial effect of early thrombolysis on LVEF. The Canadian VHR registry showed superior one-year clinical outcomes in the Pharmacoinvasive group. This advantage is related to the speed of management in the PIs group, 68.7% of patients in this group had reperfusion within 3 hours compared to 40.6% of PAMI patients with a time related to angioplasty estimated at 84 minutes [19].
In our study, the mid-term clinical results are comparable in the two groups. Reperfusion within 3 hours was only observed in 21.4% of PAMI patients and 48% of PIs patients. Improving treatment times can lead to improved clinical results in our population. In this study, even though the PIs group had shorter total ischemia time and better TIMI flow after angioplasty, there were no significant differences in in-hospital and one-year follow-up outcomes, which may be due to small sample size and could shift in favor of PIs strategy in long-term follow-up or in high-risk subgroups.
In our study, we objectified a more frequent indication of coronary bypass in patients of the PIs group (10.6% vs 0%). This is probably related to the non-emergency circumstances in which the angiogram was performed and the revascularization decisions were made, this is an important point that can be credited positively to the pharmaco-invasive arm especially in view of the high prevalence of diabetes and therefore complex lesions in our population. Despite the encouraging results, our study suffers from some shortcomings; first of all, the monocentric and retrospective nature evokes a lack of data and a limited sample, especially in the PAMI group. Then the period of the study coincided with the Coronavirus COVID19 pandemic, several patients have caught covid19 which may influence the results on mortality and morbidity in the short and medium term. In the end, the maximum follow-up of 12 onths was insufficient for the long-term prognosis.
In perspective, our results are important for low- and middleincome countries such as Tunisia because they demonstrate that, regardless of the health system, in the PIs group, lytic treatment and medical therapy associated with immediate or rapid transfer for angioplasty (rescue or systematic) are beneficial and necessary and improve clinical outcomes. The ease of use, efficacy and safety of the new thrombolysis molecules further validate the feasibility and benefit of the PIs strategy. Therefore, our study supports the need for greater emphasis on improving fibrinolysis and transfer network systems in low- to middle-income countries without widespread availability of timely primary angioplasty.
Conclusion
In our Tunisian context, the short and midterm clinical outcomes are comparable for the two reperfusion strategies in STEMI. The PIs strategy is associated with a significant reduction in ischemic time and a tendency to reduce the occurrence of heart failure compared to the primary angioplasty. Other multicenter studies are necessary to validate and approve the feasibility and safety of the PIs strategy in the treatment of STEMI everywhere.
Ethical considerations
Data analysis was carried out in compliance with the values of medical ethics, anonymity and confidentiality. Prior oral consent was obtained from each patient participating in this study.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Boersma E, Maas ACP, Deckers JW, Simoons ML (1996) Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet (London, England) 348(9030): 771-775.
- Morrison LJ, Verbeek PR, McDonald AC, Sawadsky B V, Cook DJ (2000) Mortality and prehospital thrombolysis for acute myocardial infarction: A meta-analysis. JAMA 283(20): 2686-2692.
- Van De Werf F (2009) CardioPulse Articles. Eur Heart J 30(23): 2817-2828.
- Bøhmer E, Hoffmann P, Abdelnoor M, Arnesen H, Halvorsen S (2010) Efficacy and safety of immediate angioplasty versus ischemia-guided management after thrombolysis in acute myocardial infarction in areas with very long transfer distances results of the NORDISTEMI (NORwegian study on DIstrict treatment of ST-elevation myocardial infarction). J Am Coll Cardiol 55(2): 102-110.
- Cantor WJ, Fitchett D, Borgundvaag B, Ducas J, Heffernan M, et al. (2009) Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med 360(26): 2705-2718.
- Addad F, Mahdhaoui A, Gouider J, Boughzela E, Kamoun S, et al. (2019) Management of patients with acute ST-elevation myocardial infarction: Results of the FAST-MI Tunisia Registry. PLoS One 14(2): e0207979.
- Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Danays T, et al. (2013) Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med 368(15): 1379-1387.
- Hanssen M, Cottin Y, Khalife K, Hammer L, Goldstein P, et al. (2012) French Registry on Acute ST-elevation and non ST-elevation Myocardial Infarction 2010. FAST-MI 2010. Heart Mai 98(9): 699-705.
- Danchin N, Puymirat E, Steg PG, Goldstein P, Schiele F, et al. (2014) Five-year survival in patients with ST-segment-elevation myocardial infarction according to modalities of reperfusion therapy: the French Registry on Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) 2005 Cohort. Circulation 129(16): 1629-1636.
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, et al. (2018) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39(2): 119-177.
- Denktas AE, Anderson HV, McCarthy J, Smalling RW (2011) Total Ischemic Time: The Correct Focus of Attention for Optimal ST-Segment Elevation Myocardial Infarction Care. JACC Cardiovasc Interv 4(6): 599-604.
- Gershlick AH, Westerhout CM, Armstrong PW, Huber K, Halvorsen S, et al. (2015) Impact of a pharmacoinvasive strategy when delays to primary PCI are prolonged. Heart 101(9): 692-698.
- Ndrepepa G, Mehilli J, Schulz S, Iijima R, Keta D, et al. (2008) Prognostic Significance of Epicardial Blood Flow Before and After Percutaneous Coronary Intervention in Patients With Acute Coronary Syndromes. J Am Coll Cardiol 52(7): 512-517.
- Welsh RC, Van De Werf F, Westerhout CM, Goldstein P, Gershlick AH, et al. (2014) Outcomes of a pharmacoinvasive strategy for successful versus failed fibrinolysis and primary percutaneous intervention in acute myocardial infarction (from the strategic reperfusion early after myocardial infarction [STREAM] study). Am J Cardiol 114(6): 811-819.
- Nan J, Meng S, Hu H, Jia R, Jin Z (2021) Fibrinolysis Therapy Combined with Deferred PCI versus Primary Angioplasty for STEMI Patients During the COVID-19 Pandemic: Preliminary Results from a Single Center. Int J Gen Med 14: 201-209.
- Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Danays T, et al.(2013) Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med 368(15): 1379-1387.
- Sim DS, Jeong MH, Ahn Y, Kim YJ, Chae SC, et al. (2016) Pharmacoinvasive Strategy Versus Primary Percutaneous Coronary Intervention in Patients with STSegment-Elevation Myocardial Infarction: A Propensity Score-Matched Analysis. Circ Cardiovasc Interv 9(9): e003508
- Sinnaeve PR, Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, et al. (2014) ST-segment-elevation myocardial infarction patients randomized to a pharmacoinvasive strategy or primary percutaneous coronary intervention: Strategic Reperfusion Early After Myocardial Infarction (STREAM) 1-year mortality follow-up. Circulation 130(14): 1139-1145.
- Bainey KR, Armstrong PW, Zheng Y, Brass N, Tyrrell BD, et al. (2019) Pharmacoinvasive Strategy Versus Primary Percutaneous Coronary Intervention in STElevation Myocardial Infarction in Clinical Practice: Insights From the Vital Heart Response Registry. Circ Cardiovasc Interv 12(10):
- Westerhout CM, Bonnefoy E, Welsh RC, Steg PG, Boutitie F, et al. (2011) The influence of time from symptom onset and reperfusion strategy on 1-year survival in ST-elevation myocardial infarction: A pooled analysis of an early fibrinolytic strategy versus primary percutaneous coronary intervention from CAPTIM and WEST. Am Heart J 161(2): 283-290.
- Siddiqi TJ, Usman MS, Khan MS, Sreenivasan JK, Kassas I, et al. (2018) Meta- Analysis Comparing Primary Percutaneous Coronary Intervention Versus Pharmacoinvasive Therapy in Transfer Patients with ST-Elevation Myocardial Infarction. Am J Cardiol 122(4): 542-547.
- Solhpour A, Chang KW, Arain SA, Balan P, Zhao Y, et al. ( 2016) Comparison of 30-day mortality and myocardial scar indices for patients treated with prehospital reduced dose fibrinolytic followed by percutaneous coronary intervention versus percutaneous coronary intervention alone for treatment of ST-elevation myocardial infarction. Catheter Cardiovasc Interv 88(5): 709-715.
-
Hichem Denguir*, Mohamed Derwiche, Slim Abidi, Saher Gmiha, Marouene Haloui, Ahmed Elbatrawi and Marouene Gorii. Feasibility of Pharmacoinvasive Strategy in ST Segment Elevation Myocardial Infarction STEMI in the Tunisian Context: Monocentric Experience. On J Cardio Res & Rep. 7(3): 2023. OJCRR.MS.ID.000665.
-
Myocardial infarction, Pathology, Coronary angiogram, Angiographic characteristics, Heart failure, Thrombolysis, Angioplasty, Outcomes, Mortality, Chronic kidney disease, Percutaneous coronary intervention, Cardio Report
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






