 Case Report
Case Report
An Elderly Lady with Unexpected Oligosymptomatic Aortopulmonary Window Associated with Atrial Septal Defect: Rare Case from Bangladesh
Richmond R Gomes1* and Salim Mahmod2
1Department of Medicine, Ad-din Women’s Medical College Hospital, Bangladesh
2Department of Cardiology, Ad-din Women’s Medical College Hospital, Bangladesh
Richmond R Gomes, Department of Medicine, Ad-din Women’s Medical College Hospital, Bangladesh.
Received Date: November 02, 2022; Published Date: November 15, 2022
In aortopulmonary window (APW) (also known as aortopulmonary septal defect, aortopulmonary fenestration), a large defect is present between intrapericardial portion of the ascending aorta and the main pulmonary artery. This condition results from failure of the spiral septum to completely divide the embryonic truncus arteriosus. AP window is a rare lesion that can mimic patent ductus arteriosus (PDA) clinically and comprises only 0.1% to 0.6% of congenital heart defects. The defect is usually large; therefore, the likelihood of established pulmonary hypertension in the adult patient is high unless closure took place early in childhood. About 10% of aortopulmonary windows are relatively small and restrictive, in terms of pressure, and, therefore, not susceptible to early pulmonary hypertension. Aortopulmonary windows are commonly associated with other cardiac lesions such as ventricular septal defect (VSD), tetralogy of Fallot, subaortic stenosis, atrial septal defect (ASD), or PDA and thus can be easily overlooked. Occasionally, the right and rarely the left coronary arteries are transposed to the pulmonary trunk, and this must be taken into consideration in the surgical planning. Fifty percent of patients usually have no other heart defects. Here we describe an elderly Bangladeshi lady with chronic exertional dyspnoea for years. She was found to have aorto pulmonary window with atrial septal defect on echocardiography with mild pulmonary hypertension. She was referred to a higher center for surgical management.
Keywords:Aortopulmonary window; Congenital heart defects; Atrial septal defect; Pulmonary hypertension
Introduction
An aortopulmonary window (APW) is a rare congenital heart disease consisting of a communication between the PA and the intrapericardial portion of the ascending aorta in the presence of two separate semilunar valves, sometimes associated with 22q deletion syndrome. Approximately 50% of patients with APW have associated anomalies, such as a right aortic arch, type
A interruption of the aortic arch, anomalous origin of a coronary artery from the PA, TOF, TGA, VSD, or origin of the right PA from the aorta. It accounts for 0.2% to 0.6% of all congenital heart diseases [1]. Most patients with APW develop congestive heart failure in infancy owing to left-to-right shunt [2]. The survival rate of patients with large untreated APW is very low, with a mortality rate of 40% in the first year [3]; few patients with APW survive to adulthood.
Case Eeport
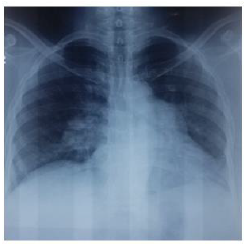
A 55-year-old pleasant lady from rural Bangladesh patient presented to us with chest tightness and shortness of breath (NYHA grade II/III) especially on exertion for more than 10 years and intermittent haemoptysis since then. The patient underwent medical evaluation when he was approximately 25 years old. Congenital heart disease was considered, but the exact cause of his chest symptoms was unknown because of limited medical resources at that time. Therefore, during the course of the disease, he had no systematic diagnosis and received no treatment. He had no history of hypertension, diabetes, coronary heart disease, smoking or related family diseases. But the patient suffered from recurrent respiratory infections since childhood which required repeated hospital admissions. Physical examination revealed the following: blood pressure: 110/70 mmHg, heart rate: 72 bpm, respiratory rate: 14 bpm and oxygen saturation: 94%. There was no cyanosis or clubbing. No dry or moist rales were heard on auscultation. The P2 heart sound was loud, and a grade 3/6 systolic murmur was ausculted over the upper left parasternal area in second intercostals space. Routine blood test results were as follows: Complete blood count was within normal limit with normal differentials and B-type natriuretic peptide concentration: 93.90 ng/L (reference range, 0–100 ng/L). Liver and renal function, urinalysis and other laboratory test results were normal. The cardiac borders were normal except fullness of pulmonary conus on chest radiograph (Figure 1).
Figure 1:Chest x ray PA view showing enlargement of pulmonary conus and enlarged pulmonary artery.
Electrocardiography suggested sinus rhythm. Transthoracic echocardiography revealed ostium secundum ASD (16 mm) (Figure 2) with aorto pulmonary window just beyond pulmonary valve at the level of bifurcation of pulmonary artery (Figure 3). The right ventricle and pulmonary artery were mildly dilated. There was mild pulmonary hypertension with PASP 42 mm. The size of the left ventricular end-diameter was normal, and the left ventricular ejection fraction was 63%. The final diagnosis was ostium secundum ASD combined with APW was confirmed. The patient started sildenafil and referred to thoracic surgeon for further surgical management.
Figure 2:Transthoracic echocardiography revealed ostium secundum ASD (16 mm) (Figure A) with aorto pulmonary window just beyond pulmonary valve at the level of bifurcation of pulmonary artery (Figure B).

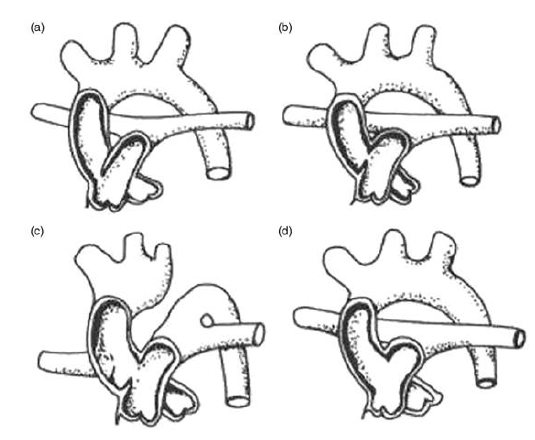
Figure 3:APW classification diagram. (A) Type I, proximal defect. (B) Type IIA, distal defect with the right pulmonary originating from the main pulmonary artery. (C) Type IIB, distal defect, anomalous origin of the right pulmonary from the aorta. (D) Type III, total defect.
Discussion
APW, also known as Aortopulmonary septal defect, is a rare congenital heart disease. APW is defined as direct communication between the ascending aorta and the main pulmonary artery owing to incomplete separation of the arterial trunk into the aorta and pulmonary artery during embryogenesis [4]. AP window was first described by J. Elliotson in 1830. Some studies have shown a male preponderance (2: 1). The first successful surgical closure of AP window was reported by Robert Gross in 1952. APW can appear as an isolated lesion, or may be combined with other cardiac abnormalities, such as ventricular septal defect, atrial septal defect, patent ductus arteriosus and tetralogy of Fallot [5]. Our patient was diagnosed with APW combined with ostium secundum ASD. According to the classification proposed by Mori, et al. [5], APW is divided into three types.
Type I indicates an APW located in the pulmonary artery bifurcation before the proximal defect, and the left pulmonary artery and main pulmonary artery maintain a normal relationship. Type II indicates an APW located at the bifurcation of the left and right pulmonary arteries, with a distal defect in an oblique direction. Type II APW accounts for only 10% of all APW cases. Berry, et al. [6]. modified the Mori classification according to the origin of the right pulmonary artery. In the modified classification, Type II is further divided into Type IIA and Type IIB. Type IIA indicates that the right pulmonary artery originates from the main pulmonary artery. Type IIB represents anomalous origin of the right pulmonary artery from the aorta (AORPA), often combined with aortic arch hypoplasia and patent ductus arteriosus; our patient had type IIB. Type III is a compound type with proximal and distal defects and complete absence of the aortopulmonary septum (Figure 1).
The pathophysiological changes in APW are complicated. Through the defect, a large amount of high-pressure aortic blood ejects directly into the proximal end of the pulmonary artery, which first leads to pulmonary hypertension and pulmonary congestion. Second, the continuous impact of high-pressure blood flow can induce pulmonary arteriolar spasm, intimal thickening and luminal thinning, which increases resistance. These pathophysiological changes can lead to pulmonary hypertension. Excessive pulmonary artery pressure can increase right heart load, which can induce right ventricular enlargement and dilatation and lead to right heart failure. Large APW defects and left ventricular volume overload cause left ventricular enlargement and dilatation, which can induce left heart failure. Severe cases can quickly develop complete heart failure after birth.
Infants with an aortopulmonary window present either with congestive heart failure or, if pulmonary hypertension has developed, with cyanosis. Occasionally, when the aortopulmonary window is relatively small, the patient may present with a continuous murmur and signs of left-sided heart dilation owing to volume overload. The rare adult with an unoperated aortopulmonary window can present with pulmonary hypertension, cyanosis, and Eisenmenger syndrome when the aortopulmonary window is large. They differ from patients with a large PDA and Eisenmenger syndrome in that they have both upper and lower body cyanosis. A continuous murmur and variable degrees of left ventricular dilation or heart failure when the aortopulmonary window is relatively small (about 10% of cases), without fixed pulmonary hypertension. These patients should be considered for surgical or device closure.
Echocardiography and cross-sectional imaging are important in diagnosing this condition by depicting the defect clearly. The importance of color Doppler study cannot be undermined as it quantifies the flow mechanics across the defect and is thus helpful in assessing its size. Cardiac catheterization remains the gold standard for diagnosing the defect with evaluation of the shunt [7,8]. However, cross-sectional imaging including CT and MRI may suffice in many patients by depicting the defect clearly as well as evaluation of lung parenchyma and other related anomalies. This can obviate the need for an invasive procedure, where the patient was not a surgical candidate [9]. Our patient was under-diagnosis for a long time because of limited medical resources. Her right ventricle was hypertrophic, and the left ventricle was normal; ejection fraction was in the normal range with bidirectional shunting. The reason for our patient’s survival may be related to the normal left ventricular structure and function.
APW can induce early severe pulmonary hypertension, congestive heart failure, respiratory tract infections and mortality. Thus, once the diagnosis is confirmed, surgery should be performed immediately, regardless of the patient’s age. In cases with early diagnosis and Unless pulmonary hypertension is deemed irreversible [10], patients should undergo timely surgical repair. Repair of an aortopulmonary window can be performed through the aorta or the pulmonary artery, with direct suture or the use of a Dacron or pericardial patch. A modification of this technique, particularly when the right coronary artery arises from the pulmonary trunk, is to create a flap of the anterior pulmonary artery, including the origin of the right coronary artery, rechanneled into the aorta. The flap should be large enough to cover the whole aortopulmonary window. Patients undergoing this so-called tunneltype of repair are at risk of supravalvar pulmonary stenosis. Adults with aortopulmonary windows repaired early should have a normal life expectancy. As with patients with repaired PDA, however, late pulmonary hypertension may develop depending on the timing of closure and the presence/absence of pulmonary vascular disease at the time of closure. Rarely, the origin of stenosis of the coronary arteries, which themselves may have been transplanted from the pulmonary trunk, can be a feature that merits attention.
In cases with early diagnosis and no other abnormalities, the intra operative mortality is low, and the long-term prognosis is satisfactory; however, surgery is not an option for patients with Eisenmenger syndrome [10,11]. For patients who have lost the opportunity for surgery, medical treatment is the only option to relieve symptoms, such as pulmonary hypertension, heart failure and respiratory tract infections. The treatment strategies for patients with Eisenmenger syndrome are stated in major clinical guidelines. Studies have shown that vasodilators may improve symptoms, and the main medications are endothelin receptor antagonists (e.g., bosentan), phosphodiesterase inhibitors (e.g., sildenafil) and prostacyclins (e.g., iloprost). Bosentan can improve patients’ exercise endurance and haemodynamics. Studies have shown that sildenafil is also beneficial regarding mortality [12]. If irreversible pulmonary hypertension has developed, patient is usually managed with anticoagulants and phlebotomy if haematocrit is more than 55% [7]. Heart– lung transplantation may be another treatment, according to a case reported by Bobylev, et al. [13-15]. which was a patient who underwent heart–lung transplantation for APW combined with Eisenmenger syndrome as the final treatment. The hope is that the ideal treatment plan can be determined with future research. Until more is known, early detection and diagnosis of APW is critical. The literature suggests that the median survival for uncorrected APW is 33 years [16]. The longest reported survival for untreated APW with Eisenmenger syndrome is 60 years [17]. which our patient has exceeded and continues to be followed-up.
Conclusion
Aortopulmonary window is a very rare congenital cardiac anomaly and adult survival without treatment, although known, is quite uncommon. The surgery for correction of APW has evolved over years, currently an open repair on cardiopulmonary bypass (CPB) with a single patch technique yields good results. Mortality is affected by the association of pulmonary hypertension and other cardiac malformations. This anomaly should be kept in mind and sought for in an adult patient with unexplained pulmonary hypertension.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Kutsche LM, Van Miersop LH (1987) Anatomy and pathogenesis of aorticopulmonary septal defect. Am J Cardiol 59: 443-447.
- Suneil Kumar Aggarwal, Jitendra Mishra, Vijay Sai, V Ramnath Iyer, BKP Panicker (2008) Aortopulmonary window in adults: diagnosis and treatment of late-presenting patients. Congenit Heart Dis 3: 341-346.
- Joud El Dick, Issam El-Rassi, Christelle Tayeh, Fadi Bitar, Mariam Arabi (2019) Aortopulmonary window in adults: a rare entity leading to Eisenmenger syndrome. Echocardiography 36: 1173-1178.
- Barnes ME, Mitchell ME, Tweddell JS (2011) Aortopulmonary window. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 14: 67-74.
- K Mori, M Ando, A Takao, S Ishikawa, Y Imai (1978) Distal type of aortopulmonary window. Report of 4 cases. Br Heart J 40: 681-689.
- T E Berry, S Bharati, A J Muster, F S Idriss, B Santucci, et al. (1982) Distal aortopulmonary septal defect, aortic origin of the right pulmonary artery, intact ventricular septum, patent ductus arteriosus and hypoplasia of the aortic isthmus: a newly recognized syndrome. Am J Cardiol 49: 108-116.
- Kose M, Ucar S, Emet S, Akpinar TS, Yalin K (2015) A case of aortopulmonary window: asymptomatic until the first pregnancy. Case Rep Cardiol 2015: 935253.
- Demir IH, Erdem A, Sarıtas. T, Demir F, Erol N, et al. (2013) Diagnosis, treatment and outcomes of patients with aortopulmonary window. Balkan Med J 30(2): 191-196.
- Sridhar PG, Kalyanpur A, Suresh PV, Sharma R, Maheshwari S, et al. (2006) Helical CT evaluation of aortopulmonary septal defect. Ind J RadiolImag 16(4): 847-849.
- Deepak Gowda, Trushar Gajjar, Jinaga Nageswar Rao, Praveen Chavali, Aaditya Sirohi, et al. (2017) Surgical management of aortopulmonary window: 24 years of experience and lessons learned. Interact Cardiovasc Thorac Surg 25: 302-309.
- Sachin Talwar, Palkesh Agarwal, Shiv Kumar Choudhary, Shyam Sunder Kothari, Rajnish Juneja, et al. (2017) Aortopulmonary window: morphology, diagnosis, and long-term results. J Card Surg 32: 138-144.
- Nazzareno Galiè, Marc Humbert, Jean-Luc Vachiery, Simon Gibbs, Irene Lang, et al. (2016) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37: 67-119.
- Basit H, Wallen TJ, Sergent BN (2020) Eisenmenger Syndrome. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Hartwig BJ, Schultze B (2019) Review of evidence for bosentan therapy for treatment of Eisenmenger syndrome. J Am Assoc Nurse Pract 31: 72-77.
- Dmitry Bobylev, Wiebke Sommer, Murat Avsar, Alexander Horke, Axel Haverich, et al. (2014) Aortopulmonary window: a rare untreated adult case. Heart Lung Circ 23: e235-e236.
- Murat Kose, Serra Ucar, Samim Emet, Timur Selcuk Akpinar, Kıvanc Yalin (2015) A case of aortopulmonary window: asymptomatic until the first pregnancy. Case Rep Cardiol 2015: 935253.
- Su-Mei AK, Ju-Le T (2007) Large unrepaired aortopulmonary window–survival into the seventh decade. Echocardiography 24: 71-73.
-
Richmond R Gomes* and Salim Mahmod. An Elderly Lady with Unexpected Oligosymptomatic Aortopulmonary Window Associated with Atrial Septal Defect: Rare Case from Bangladesh. On J Cardio Res & Rep. 6(5): 2022. OJCRR.MS.ID.000649
-
Aortopulmonary window, Congenital heart defects, Atrial septal defect, Pulmonary hypertension, Echocardiography, Cardiac abnormalities, Ventricular septal defect, Pericardial patch, Cardiopulmonary bypass
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






