 Research Article
Research Article
The Prevalence and Patterns of Use of Herbal Medicine in Wad Madani, Sudan, 2016: A Community Based Cross-Sectional Study
Khawla Ismat, Faculty of medicine, University of Khartoum, Sudan.
Received Date:November 29, 2022; Published Date:February 14, 2023
Abstract
Aim: Herbal medicine as part of conventional medicine is becoming a trend and (kambooj 2000) stated that they are being used by about 80% of the world population mainly in the developing countries, so we conducted a study aiming to determine the prevalence of use of herbal products and the causes of their use.
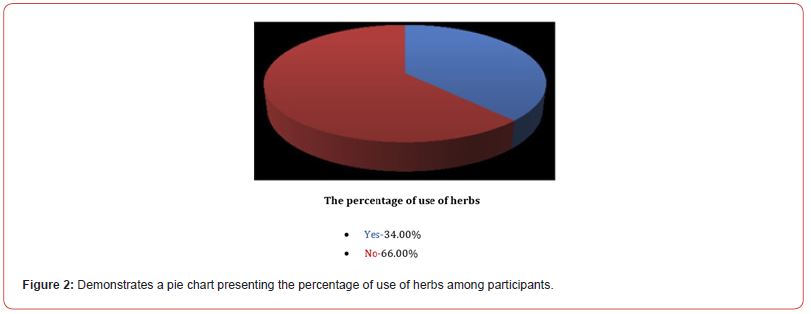
Methods: a descriptive cross-sectional community-based study was conducted on residents of Wad Madani locality, Sudan by distributing 150 structured questionnaires, investigating for the most common herbs used and their pattern of use. The prevalence of use was found to be 66.0% and the most common cause for use was the assumption by the participants that herbal products are more effective than conventional medicines, also the participants were found unaware of the possible interactions of herbs with conventional drugs and unaware of the lack of evidence-based information regarding herbal products.
Conclusion: this study confirms trends seen in other studies that there is a dramatic increase in herbal medicine use and health education to the public should be encouraged regarding the possible interactions of herbs with conventional drugs and the lack of evidence-based information in this area.
Keywords:Herbal medicine; Alternative medicine; Prevalence of use
Abbreviations:WHO: World Health Organization
Introduction
Background
Herbal medicine is being used as complementary or even alternative of conventional medicine. Complementary or traditional medicine is defined as: “The sum of knowledge or practices, used in prevention or elimination of diseases and relaying exclusively on experience and observation handed from generation to generation, whether verbal or written [1].” WHO stated that herbal medicine includes herbs, herbal materials, herbal preparations and finished herbal products that contain as active ingredients parts of plants, or other plant materials, or combinations [2]. Through its long history, Sudan has witnessed the fusion of many cultures, Pharaonic, Islamic, and Christian along with the local indigenous cultures. In addition, Sudan encompasses different terrains and climatic zones. This variation contributes to the immense diversity of vegetation in the region. The flora of Sudan consists of 3137 species of flowering plants belonging to 170 families and 1280 genera. It is estimated that 15% of these plants are endemic to Sudan [3]. The intersection of diverse cultures and the unique geography holds great potential for Sudanese herbal medicine.
Statement of the problem
Using of herbal medicines solely as an alternative to conventional medicine compromises the delivery of the appropriate evidence- based conventional health care services, delaying the appropriate treatment and increasing the burden of diseases. When an unconventional treatment is tried in a patient with a serious medical disorder, this can entail the risk that a well proven conventional care being delayed [4].
Justification of the problem
According to the world health organization (WHO), the use of herbal remedies exceeds that of conventional drugs by two to three times [5]. Nowadays the use of herbal product is becoming a trend, with the emerging companies which sales herbal recipes as treatment for all types of diseases, gaining the attention of the population through media which participate in the trends of those companies. This research would enlight the decision makers about the magnitude of the prevalence of use of herbs, and about the causes of using them, also it would provide information about the types of herbs commonly used, providing a basic knowledge for further studies and for researchers to study the efficacy and side effects of the commonly used herbs.
Literature review
In Saudi Arabia, a cross sectional hospital-based study on diabetics reported [6] that 17.4% used herbal products and 42% took herbs according to their friend’s advice, this may draw the attention to the health education in the community. A survey conducted on surgical patients [7], recorded that 57% of their respondents used herbal medicine, while in another study conducted on parturients [8],in the united states in tertiary hospitals, found that the use was infrequent and reported that 7% of nulliparas and 7.7% of multiparas used herbal remedies, all of those studies were conducted on specific groups of the patients, while the current study would be community based, being more representative of the population under study. A study done in Sudan added the easy availability of local medicinal plants as a factor contributing to the choice of herbal therapies [9]. Another study from India [5] reviewed the difference between herbal and conventional drugs, regulations, safety issues and the need for clinical trials, they stated that” the manufacturers and the regulatory agencies must apply rigorous scientific methodologies and clinical trials to ensure the quality and lot-to-lot consistency of the traditional herbal products”.
There is a wide variety of medicinal plants used, El-Kamali conducted a study on the ethno pharmacology of medicinal plants in North Kurdufan region, Sudan in which they performed personal interviews in the form of group discussions for the urban and rural inhabitants, during fieldwork plant materials were collected for preparation of herbarium specimens and for biological and chemical testing, they recorded the types of plants, the part of a plant used, their preparation and the conditions managed by those plants. The data recorded during the study were compared with the related literature and published reports on the traditional medicinal uses of the plants. Some species, namely, Abutilon panosum, Blepharislinariifolia, Cassiaabsus, Doberaglabra, Justiciaflava, Ethuliaconyzoides, Xeromphisnilotica, Tinosporabakisand Strigahermonthicahave never been described in the ethnobotanical literature of Sudan. For other species, namely, Acacia niloticassp. nilotica, Cissusquadrangularis, Geigeriaalata, Hibiscus sabdariffa and Ziziphusspins-christi, new therapeutic uses have been reported [9]. In a qualitative study from United Kingdom [10] the interviewees were asked about co-herbal conventional interactions also about their beliefs about herbal testing, while Lee, Shin, and Ernst [11] have done a systematic review about the interactions between herbal medicines and prescribes drugs and concluded that interactions do exist.
Specific objectives
To determine the prevalence of people using herbs, to determine the factors that influence the choice of these types of medications (i.e. sociodemographic factors, economic factors or fear of side effects of conventional drugs...etc.), to determine the sources of herbs (i.e. bought over the counter or from specialized herbal remedies companies), patterns of their use, identify the types of herbs used and types of illnesses managed by them. In addition, the study is aiming to detect the awareness of people about that herbal medicine is not evidence-based and their awareness about the possible interactions between herbs and convention.
Materials and Methods
This descriptive community based, cross-sectional study was conducted in Wadmadani locality, Al-Gazeira state, Sudan. The participants were adults (18 years or above), living in Wadmadani locality for more than 6 months. Mentally retarded people or those who refused to participate were excluded from being enrolled in the study. The sample size required for adequate power was 383, based on a 5% margin of error, but due to some limitations which are mentioned in the discussion section, I had to reduce the sample size to be 150. A multistage sampling and probability proportional to size technique was used. Information about the units of the locality, the number of the population in each unit and each neighborhood were obtained from the local authorities, according to probability proportionate to size technique, 3 out of 6 units of the locality was chosen, and 5 neighborhoods from each of the three units were chosen, then 10 questionnaires were distributed for each of the 15 neighborhoods, making a sample of total 150 questionnaires. Data has been collected by standardized structured self-administered questionnaire containing closed ended questions about the demographic data, the use of herbs, pattern of use, causes of use and awareness related questions. It also contains open ended questions about the types of herbs and the type of diseases dealt with by using herbs.
Statistical analysis
Statistical analysis using descriptive and inferential methods were conducted using IBM SPSS version 23 software. Graphs and tables were produced using Microsoft office Word and Excel software after obtaining information from SPSS output. Descriptive methods were used to obtain frequency tables. Inferential methods included chi square tests of association between sociodemographic variables and herbal medicine use.
Results
Demographics

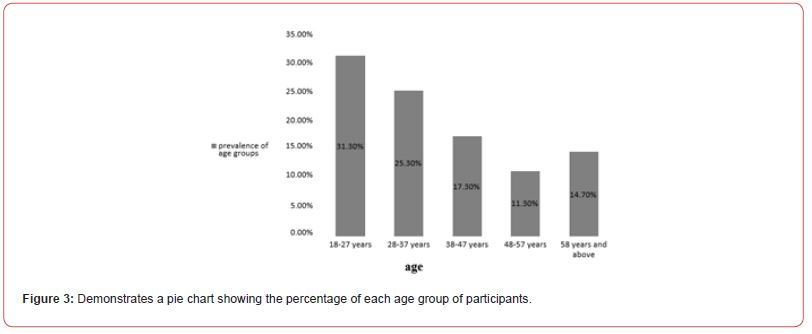
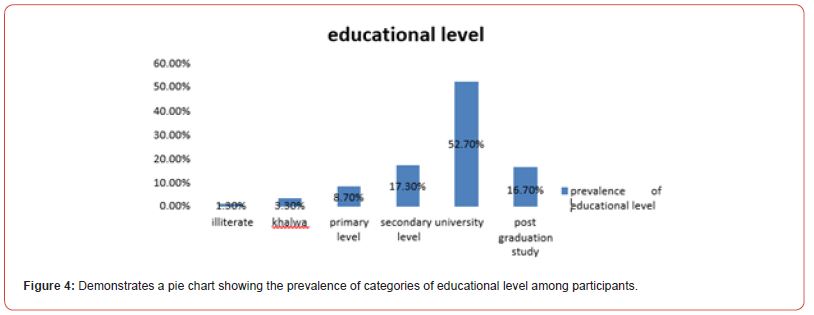
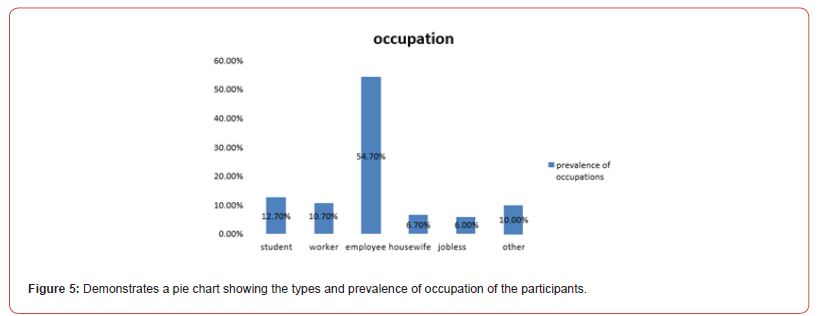
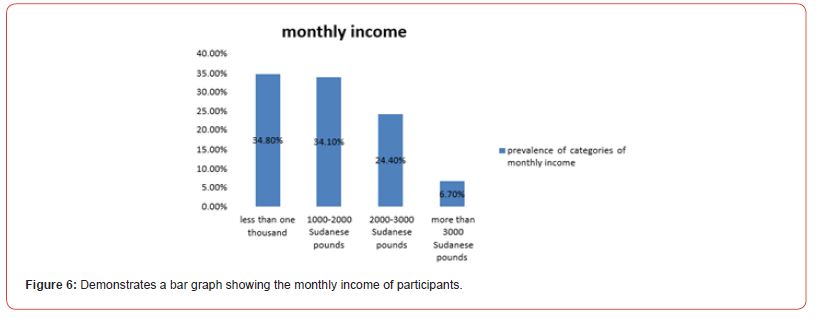
150 participants were enrolled in the study; the majority of them were females (n=93, 62.0%) (figure 1), in the (18-27 years) age group (n=47, 31.3%)(figure 3), educated till university level (n=79, 52.7%) (figure 4), employees (n= 81, 54%) (figure 5), and most of them earn less than one thousands Sudanese pounds monthly (n=47, 34.8%) (figure 6). Table (1) demonstrates that the study didn’t show any significant association between herbal medicine use and age, gender, level of education, occupation and monthly income.
Table 1: Demonstrates the association between socio demographic variables and the use of herbs.
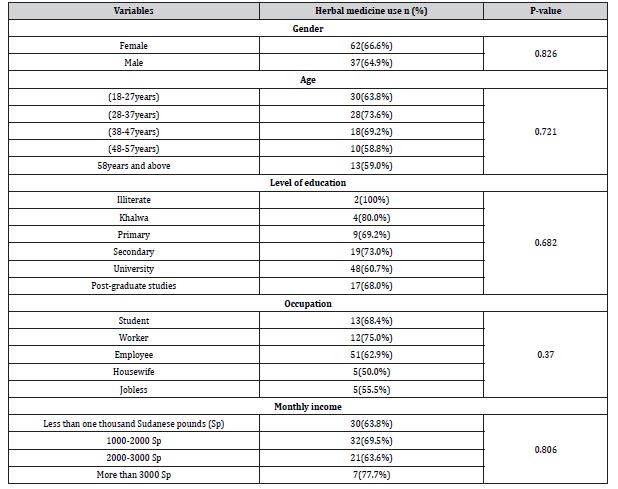
Table 2: Demonstrates the attitudes and patterns of use of herbs.
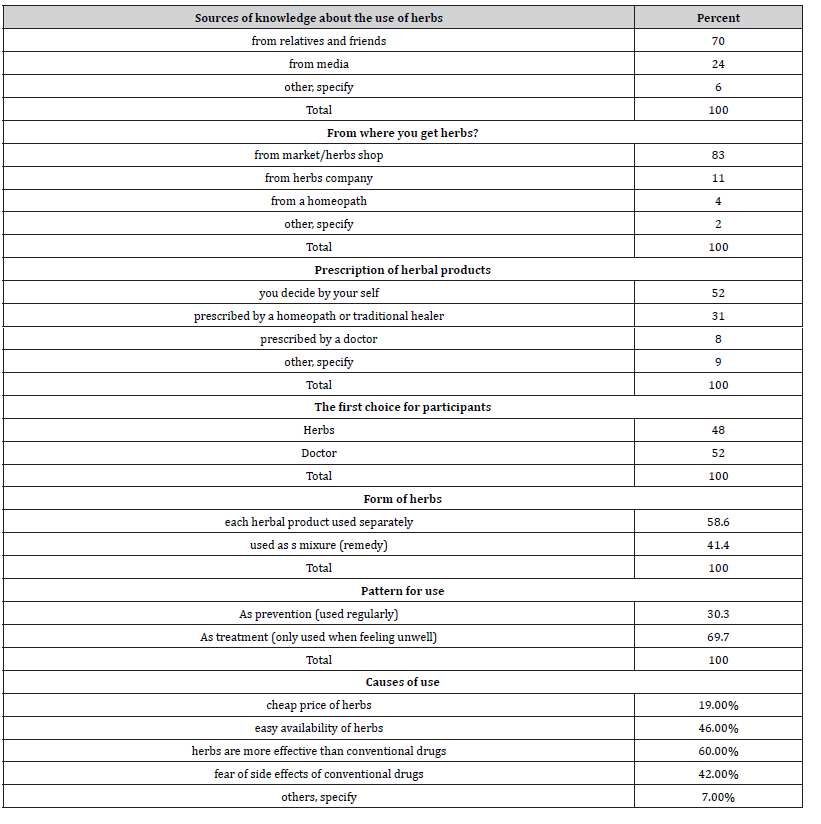
Table 3: Demonstrates frequencies of diseases dealt with by herbs.
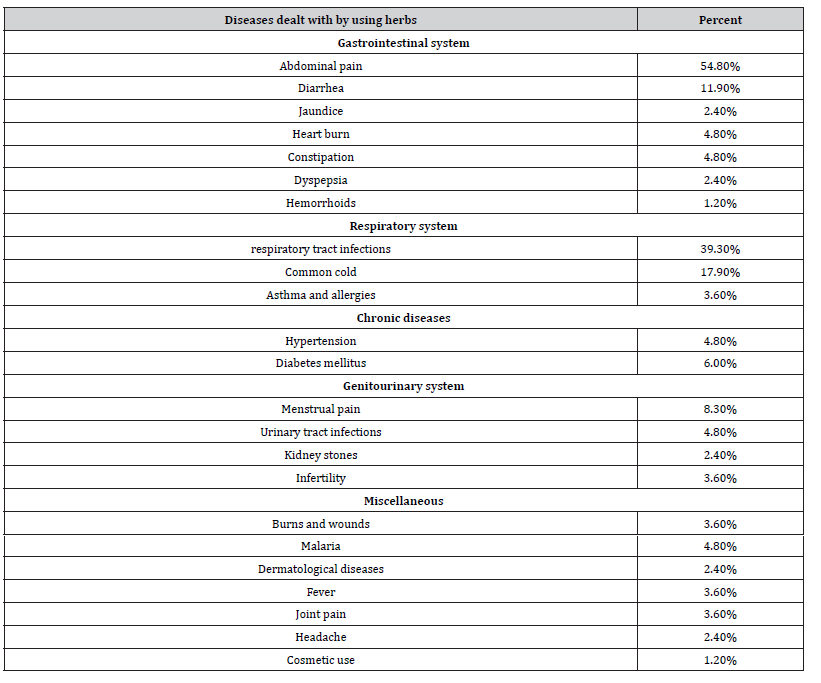
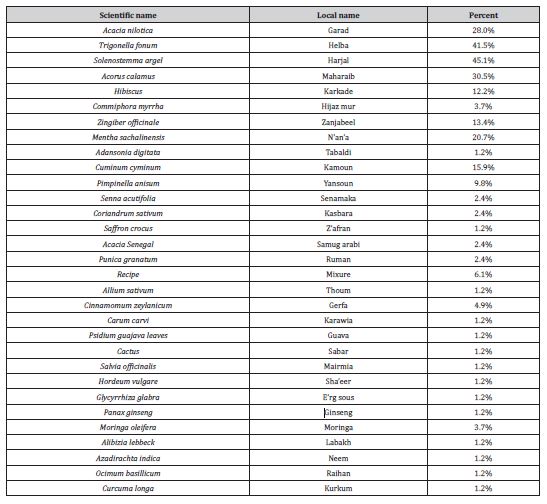
Table 4: Demonstrates the frequencies of types of herbs used.
Prevalence and patterns of use
The prevalence of herbal medicine use among participants was 66.0% (figure 2). In this group of herbal medicine users, 48% (n=48) reported that when they feel unwell they would use herbal products first, in contrast to the 52% (n=52) who would seek for a physician help first, while 50 participants didn’t respond for this question (Table 2). Among users of herbal medicine, the most troublesome diseases were abdominal pain (54.8%), respiratory tract infections (39.3%), common cold (17.9%), diarrhea (11.9%), menstrual pain (8.3%) and diabetes mellitus (6.0%) (Table 3). Only 39.0% of herbal products users reported that they determine the types of herbs they use according to a homeopath/traditional healer (31.0%) or a physician prescription (8.0%), the majority (52.0%) reported that they decide by themselves (Table 2). The most common herbs used were Solenostemma argel (45.1%), Trigonella fonum (41.5%), Acorus calamus (30.5%), Acacia nilotica (28.0%), Mentha sachalinensis (20.7%), Cuminum cyminum (15.9%), Zingiber officinale (13.4%) and Hibiscus (12.2%) (Table 4). In addition, 69.7% of the users reported that they use herbal products as a treatment method i.e. (they use them only when they feel unwell), while 30.3% use them as a prevention method i.e. (they use them regularly). 41.4% of the users took herbal products in the form of a mixture (remedy), while the majority (58.6%) took each herbal product separately (Table 2).
Attitudes
The majority of the herbal medicine users were either advised by a friend/relative (70.0%) or influenced by advertisements in the various types of media (24.0%). 83.0% bought herbal products from market/herbs shop, while others (11.0%) brought them from herbs companies and (4.0%) from a traditional healer. 34.5% of the participants who use herbs were motivated by their belief that herbs are more effective than conventional drugs, easy availability of herbs in Sudan was the motivation for (26.4%) of the users, while (24.1%) prefer herbs because they are afraid of the side effects of the conventional drugs and only (10.9%) were motivated by the low cost of herbal products (Table 2).
Awareness
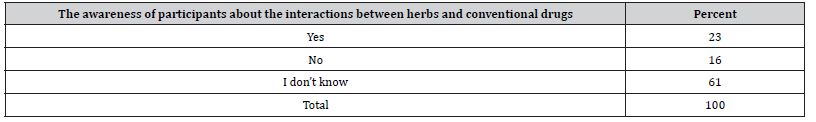
Participants who used herbs were asked if they knew that herbs efficacy is not scientifically proven, the majority (69.4%) reported that herbs are effective and it has been scientifically proven, 28.6% reported that effectiveness has not been proven scientifically but otherwise is effective by experience, only 2.0% reported that herbs are not useful at all (Table 5). 61.0% of users said that they don’t know if there is a possibility of interactions between herbal products and conventional drugs, while 23.0% responded with a (yes) answer and 16.0% said No (Table 6).
Table 5: Demonstrates the awareness of participants that herbs efficacy is not scientifically proven.

Table 6: Demonstrates the awareness of participants about the interactions between herbs and conventional drugs.
Discussion
The study sample consisted of 150 individuals, the females constituted 62.0% of the sample and the males were 38.0%, the females represented the majority in this study in contrast to Al- Rowais [6] who conducted a hospital-based study on diabetic patients, in which the males represented 56.7% of the sample, this difference between the two studies is mainly because my study is community based and mainly has targeted households during the day time, so this has increased the probability of enrolling women rather than men in the study, while Al-Rowais conducted the study in hospital where equal number of women and men are found. The prevalence of herbal medicine use was 66.0%, in agreement with a Nigerian study wih the same prevalence (66.8%) [12], compared to 17.4% in Al-Rowais study [6], this difference is attributed to the difference in objectives, as Al-rowais has asked about the use of herbs only in the period of 1 year prior to the interview, but I asked about the participant’s use in general without determining any specific period. Another study was conducted in united states on parturients [8], they found that the use was infrequent, only about 7.0%, this because their study was on specific group of the community which are women who gave or about to give birth of a child. My finding of 66.0% is considered a high prevalence, but it was expected to be higher if I had a larger sample size.
The use of herbs was more frequent among participants in the 28-37 years age group (73.6%), compared to (69.2%) in the 38-47 years age group, but this difference in use didn’t reach statistical significance (p=0.7) (Table 1), in the other study [8], the use was more frequent in 41-50 years age group (17.1%) compared with 7.3% for 31-40 years age group, and the difference also didn’t reach statistical significance. Participants who took the herbs according to a friend or a relative advice in this study were 70.0% and this may draw attention to the importance of health education to the community (table 2). If they were well informed this might be reflected in the kind of advice, they had given. And another 24.0% were encouraged by the media to use herbs, so the education should be included in the media and there should be a strict monitoring of all types of advertisements in the media, as for Al-Rowais [6], those who used herbs following an advice from a friend were 41.7% and 45.2% for the Nigerian study [12], while Hepner, Harnett anad Segal reported 52.0% for both who followed friend advice and those who were influenced by the media [8]. Earlier on I have put a hypothesis that specialized herbal companies play a major role in the trend of herbal medicine nowadays, but my results and findings is inconsistent with that hypothesis, because only 11.0% of the participants got herbs from specialized herbal companies, while the majority of them (83.0%) bought herbs over the counter from market or herbs shops and others (4.0%) got it from traditional healers (table 2). 52.0% of the participants stated that they decide by themselves when choosing herbs (table2), clearly there is a desire among the people to make their own decisions about their health and the therapies they use, so there should be improved information for the public about the product’s constituents, dosages, level of evidence for efficacy for specific uses, extent of safety testing, drug interactions, known side effects, precautions and contraindications. All of this to avoid misuse, much research and clinical trials are needed in this field to reach such a level of knowledge. Almost half of the participants mentioned that they would seek herbal management first if they feel unwell (table 2), and by doing that they would reduce their chances of getting healed as they would delay themselves from receiving an appropriate evidence-based care and by doing so they increase the burden of the diseases upon themselves, their caregivers and upon the health system because they would be diagnosed late when their conditions become serious, difficult to treat and to deal with, once again a higher percent is expected if I had a larger sample size.
58.6% mentioned that they take each herbal product separately rather than taking a mixture (remedy), taking each herb separately is considered better and safer than mixtures, as mixture increase the chances of co-herbal interactions and in most of the cases, their contents remain unknown for the consumers. 69.7% reported that they use herbs for treatment purposes rather than for prevention (Table 2), meaning that they use it infrequently which is good to avoid any possible interactions or side effects. In this study the most common cause for use of herbs was found to be the assumption of participants that herbal products are more effective than conventional drug (60.0%) (Table 2), compared to other studies [6/27/2018], [13] and [10] who mentioned that the common cause of use of herbal therapies is the fear of the side effects of conventional drugs. There is also the economic factor mentioned by [5] and [9], they stated that conventional care is more costly and time consuming, both of them also mentioned the cultural factors and traditional beliefs as a motivation for the use of herbs but other study [13] reported that cultural and philosophical factors are not as much important. EL-Kamali [9] added the easy availability of local medicinal plants as a factor contributing to the choice of herbal therapies. My finding is totally different from the findings of the previous studies; this may be attributed to the Sudanese people’s strong belief of herbal medicine and traditional practitioners and the consideration of it as a holistic method of treatment, this issue needs to be further evaluated by additional studies.
Participants were asked about the types of herbs they use, 39 types of herbs were mentioned and the most common are (in order): Solenostemma argel-Harjal, Trigonella fonum-Helba, Acorus calamus-Maharaib, Acacia nilotica-Garad, mint, Cuminum cyminum- Kamoon, Zingiber officinale-ginger then hebiscus (table 4). In another study [9] conducted on the ethno pharmacology of medicinal plants in North Kurdufan region, Sudan and reported some of the types used by the local population, he mentioned Acacia nilotica- Garad, Adansonia digitata-Tabaldi, Azadirachta indica-Neem and others. A similar study conducted in Jordan [14], it was a twoyear survey, interviewing more than 100 herbalists throughout the country and also mentioned the common herbs and their uses. The most common types of illnesses or symptoms dealt with by using herbs found to be:
abdominal pain, upper respiratory tract infections, common cold, diarrhea, and others (table3). Vickers, Jolly, Greenfield on their qualitative study on females they stated that “The conditions women used herbal remedies for were varied, most commonly depression, anxiety and stress, colds and flu, premenstrual tension and menopausal symptoms, infections and skin complaints” [10]. While Eisenberg [15] found that the most common conditions were back problems (36%), anxiety (28%), headache (27%) and cancer or tumors (24%). But this study was for unconventional medications in general, and our study was specifically about herbs. Another 2 studies [14] and [9] also reported the types of illnesses managed by herbal products.
There are wider harms to herbal products such as poorly identified side effects or drug interactions, delay in effective treatment with increasing morbidity and disillusionment, and disappointment and depression after a lack of effect is apparent, in this area there are short-term uncontrolled and un-blinded studies. This does not equate with the efficacy usually established for prescription medicines through double-blind randomized placebo-controlled trials. The public appears unaware of these vastly different levels of evidence, as found in this study that 69.4% consider herbs are effective and scientifically proven to be effective, while 77.0% didn’t know about the possible interactions with conventional drugs, public education in this area is crucially needed.
I strongly recommend researchers to investigate about the commonly used herbs I found and to carry out clinical trials on them to find degrees of therapeutic efficacy and their side effects. The main limitation was the small sample size, because of the lack of financial and human resources and lack of time. The results and findings of the study are unique to Sudan, therefore generalization would be difficult.
Conclusion
In conclusion, this study confirms trends seen in other studies that there is a dramatic increase in herbal medicine use and governments may be reluctant to legislate for tighter control of alternative medicine given the popularity of its use the most common cause for use of herbs was the assumption of participants that the herbs are more effective than conventional drugs, also they were found unaware of their possible interactions with conventional drugs and unaware of the lack of evidence-based information regarding herbal products, so health education to the public should be encouraged regarding the above mentioned issues, by organizing health education campaigns guided by the federal ministry of health to decrease this trend of use in the future.
Ethics Approval and Consent to Participate
> Department of community medicine at faculty of medicine, university of Khartoum had approved the research’s protocol, permission number is not applicable.
> Verbal consent was obtained from the participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgement
For supervision I acknowledge Dr. Nadia Yousif Mohamed Elemam MBBs, DPH, MD community medicine, Msc. clinical psychology, Directorate of curricula and professional development and research center/Academy of health sciences.
Conflict of Interest
No conflict of interest.
- Saeed B (1984) Traditional medicine in Sudan. Biochem Educ 622(1978): 1978-1980.
- (2016) Traditional medicine: Defintions.
- Halid HK, Bdalla EA, Bdelgadir HA, Patz TO, Fferth TE (2012) Gems from traditional north-African medicine: medicinal and aromatic plants from Sudan. Nat Products Bioprospect 2(3): 92-103.
- Pa De Smet (2004) Health risks of herbal remedies: an update. Clin Pharmacol Ther 76(1): 1-17.
- Pal S, Shukla Y (2003) Herbal medicine: Current status and the future. Asian Pac J Cancer Prev 4(4): 281-288.
- Al-Rowais NA (2002) Herbal medicine in the treatment of diabetes mellitus. Saudi Med J 23(11): 1327-1331.
- Adusumilli PS, Ben porat L, Pereira M, Roesler D, Leitman IM (2004) The Prevalence and Predictors of Herbal Medicine Use in Surgical Patients. J Am Coll Surg 198(4): 583-590.
- Hepner DL, Harnett M, Segal S, Camann W, Bader AM, et al. (2002) Herbal medicine use in parturients. Anesth Analg 94(3):690-693.
- EL Kamali HH (2009) Ethnopharmacology of Medicinal Plants used in North Kordofan (Western Sudan). Ethnobot Leafl 13: 89-97.
- Vickers KA, Jolly KB, Greenfield SM (2006) BMC Complementary and Herbal medicine: women’s views, knowledge and interaction with doctors: a qualitative study. BMC Complement Altern Med 6: 40.
- Lee MS, Shin B, Ernst E (2009) Interactions Between Herbal Medicines and Prescribed Drugs a Systematic Review. BJU Int 61(15): 366-370.
- Oreagba IA, Oshikoya KA, Amachree M (2011) Herbal medicine use among urban residents in Lagos, Nigeria. BMC Complement Altern Med 11: 117.
- Menniti Ippolito F, Gargiulo L, Bologna E, Forcella E, Raschetti R (2002) Use of unconventional medicine in Italy: A nation-wide survey. Eur J Clin Pharmacol 58(1): 61-64.
- Abu Irmaileh BE, Afifi FU (2003) Herbal medicine in Jordan with special emphasis on commonly used herbs. J Ethnopharmacol 89(2-3): 193-197.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, et al. (1993) Unconventional medicine in the united states. N Engl J Med 328(4): 246-252.
- Curtis P (2004) Evidence-Based Medicine Health Care.
- Angell M, Kassirer JP (1998) Risks of untested & unregulated remedies. New Engl J Med 339(12):839-41.
- Kamboj V (2000) Herbal medicine. Curr Sci 78(1): 35-39.
- Saad B, Azaizeh H, Said O (2005) Tradition and perspectives of Arab herbal medicine: A review. Evidence-based Complement Altern Med 2(4): 475-479.
- MacLennan A (2002) The Escalating Cost and Prevalence of Alternative Medicine. Prev Med (Baltim) 35(2): 166-173.
- Barnes PM, Bloom B, Interview H (2008) Complementary and Alternative Medicine Use Among Adults and Children: United States, 2007. Natl Health Stat Report 12: 1-23.
- Ernst E, Pittler MH, Stevinson C, White A (2001) The Desktop Guide to Complementary and Alternative Medicine: An Evidence-Based Approach. Am Coll chest physicians: 670-671.
-
Khawla Ismat*. The Prevalence and Patterns of Use of Herbal Medicine in Wad Madani, Sudan, 2016: A Community Based Cross-Sectional Study. On J Complement & Alt Med. 8(2): 2023. OJCAM.MS.ID.000684.
-
Herbal medicine; Alternative medicine; Prevalence of use; Complementary; Conventional medicine; Traditional medicine; Herbal materials; Herbal preparations; Herbal products; Plant materials; Indigenous cultures; Plant combinations
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






