 Research article
Research article
Maxillary Sinusitis of Odontogenic Origin
Dumitru Hîțu1, Nicolae Chele1, Vasile Cabac2*, Alexandru Mighic1 and Bădărău Lilia1
1Department of Oro-maxillo-facial surgery and Oral implantology, Catedra de chirurgie Oro-maxilo-facial implantology oral, Arsenie Guțan
1Department of Otorhinolaryngology, N Testimony, IP USMF, Europe
Vasile Cabac, Department of Otorhinolaryngology, N Testimony, IP USMF, Europe
Received Date: November 15, 2020; Published Date:March 11, 2021
Summary
We present a retrospective study, which was performed on a batch of 177 patients diagnosed with maxillary sinusitis, selected from the total number of patients with OMF disorders during 2017-2018. The patients were examined and treated at the Department of Emergency Medicine of the Institute of Emergency Medicine, Chisinau. The article contains statistical data on odontogenic maxillary sinusitis and the breakdown by age, sex, profession, etiology, addressability, place of life, hospitalization, causal tooth and treatment methods. Results: Out of the total number of 3227 patients with OMF, maxillary sinusitis (5.48%) was established for 177 patients. The majority of the patients 52.54% are from Chisinau. The most affected are the patients aged 31-40 years, constituting 26.56%, the majority being male persons 63.27%. Admission to the medical institution prevailed for 74.01% of the cases by itself, and the medical insurance was presented for 77.97%. Hospitalization of patients ranged from 1-5 days to 55.35%. The frequency of teeth involved in the inflammatory processes of the sinus was 41.78% cases, of which 1st molar prevails with 23.16%, thus being an etiological factor. As a surgical treatment of maxillary sinusitis in the section of oro-maxillofacial surgery, radical cure is used for 58.75% cases.
Keywords:Maxillary sinus; Odontogenic sinusitis; Frequency of odontogenic infection; Surgical treatment
Introduction
Maxillary sinusitis of dental origin is quite common for adults and elderly, being less commonly seen at children and young people. This is explained by the close anatomical relationships that exist between the sinus and the dental system. An important part of the pathology of the maxillary sinus is related to the periapical diseases of the teeth, to the maneuvers of the endodontic treatment, as well as to the traumatization of the floor during and after various surgical manipulations on the teeth of the upper arch [1,2]. According to the data presented by Hîțu D, since 2008, odontogenic sinusitis constitutes 2% of the total number of patients with inflammatory disorders treated in the oro-maxillofacial surgery department [3]. Banuh I. (2010) report from a study conducted in 2008, that out of the total number of patients treated in the oro-maxillo-facial surgery section of CNȘPMU, patients with inflammatory and traumatic processes of the maxillary sinus had constituted 1.83% [4]. In 2018 Ryan E. Little states that 10% of the total number of patients with oro-maxillofacial inflammatory disorders in the United States is odontogenic sinusitis, and a study of 674 patients diagnosed with maxillary sinusitis showed that for 65.7% of cases, the etiological factor was odontogenic [5]. Odontogenic maxillary sinusitis does not have a stable frequency confirming this fact through the mentioned publications. The cause of the variation is based on the multifactorial etiology, the demographic variation as well as the predisposing factors to this pathology: overgrowth, hypoavitaminosis, immunodeficiency etc. [6]. Thus, the multifactorial etiology requires us to establish a method of diagnosis and correct complex treatment and to prevent the possible complications with the unconditional involvement of the specialists in the oro-maxillo-facial area.
The Purpose of the Study
Statistical analysis of patients with odontogenic maxillary sinusitis during the years 2017-2018.
Materials and methods
The study method used was the clinical-statistical, retrospective, based on a mixed analytical and descriptive research, using articles on the topic available in medical information search databases: PubMed, PMC, Hinari, Cyberleninka as well as specialty books, in a total of 135 articles were analyzed, of which 36 were selected. Also, in order to reach the basic goal, a batch of 177 patients diagnosed with maxillary sinusitis were examined. The standard protocol for inclusion in the batch was followed, having as reference the medical records, which included: the etiology of maxillary sinusitis, age, sex, place of life, profession, type of medical insurance, entitlement to the medical institution, how many days the patient was hospitalized, the diagnosis, type of anesthesia and treatment. The statistics: t-Student. The patients were selected from the total number of patients with OMF disorders during the years 2017-2018, which were examined and treated at the Department of Maxillofacial Surgery of the Institute of Emergency Medicine, Chisinau.
Results and Discussions
During 2 years in the Department of Surgery Oro-Maxilo-Facial, 3227 patients were treated, of which 177 patients were maxillary sinusitis, accounting for 5.48% of the total number of patients Table 1. As the number of beds in the ward remained the same, the number of the population and the birth rate decreased, as well as the number of patients decreased from 1748 patients in 2017 to 1479 patients in 2018 with 269 patients constituting 8.33%. According to the represented data, the number of patients with maxillary sinusitis is decreasing from 95 patients in 2017 to 82 patients in 2018, so with 13 patients their number has decreased (Table 1).
Table 1: Number of patients with sinusitis hospitalized during the study period.

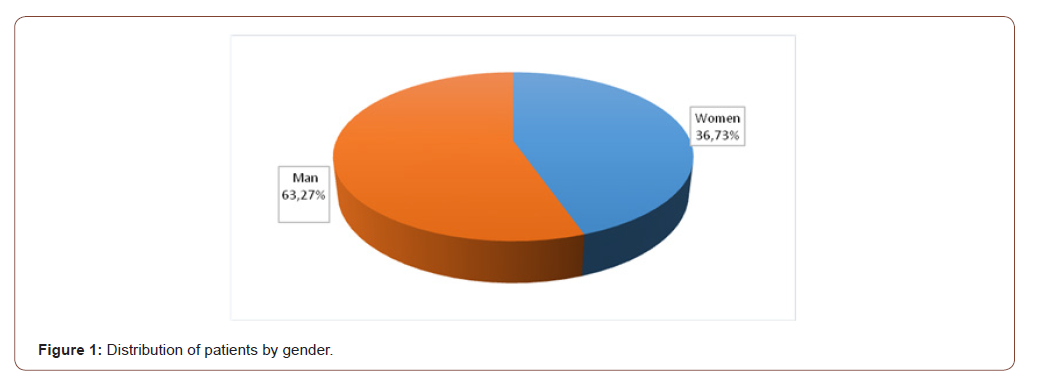
to the study conducted by Banuh I, out of the total number of patients treated in the oro-maxillo-facial surgery section within the CNȘPMU, in 2008 patients with inflammatory and traumatic processes of the maxillary sinus constituted 1.83% [3]. Mortuaire G. following a study conducted in 2017 for a period of 6 years states that the number of patients with odontogenic maxillary sinusitis increased by 1.7% from 32% in 2007 to 43% in 2013 [7]. From the analyzed statistical data and the data processed in the study we observe a variability of the percentage of maxillary sinusitis, the exact frequency remains uncertain. As a result of the processing of the data from the group of patients, they were distributed according to the gender, with 112 men representing 63.27% and 65 women, which constituted 36.73%. From the statistical data, men with a higher evident predisposition to sinus pathology are highlighted, the ratio being 26.5% Figure 1. We note the prevalence of men in the research conducted by Hâţu I. for the year 2015, which carried out a study on 93 patients with maxillary sinusitis, it reports that male persons have 55.9% and women 44.1% [8] (Figure 1).
According to Ryan E. Little data for 2018, most female patients suffer from sinusitis with a slight prevalence of 50.3% [5]. Probably the predisposition is due to the different anatomical particularities depending on the gender, namely the size of the maxillary sinuses was smaller in men than in women, and the left sinus is larger than the right one, also another causal factor could be the working conditions, smoking [9,10]. Following the retrospective study for the years 2017-2018, it was found that the largest number of patients belong to the age group 31-40 years, which constitutes 47 patients (26.56%), followed by patients aged 51-60 years in number of 37 people (19.21%). We note that the number of patients with other ages does not vary considerably, with the exception of patients up to 20 years registered with 4 cases of maxillary sinusitis (Table 2).
Table 2: Age analysis.
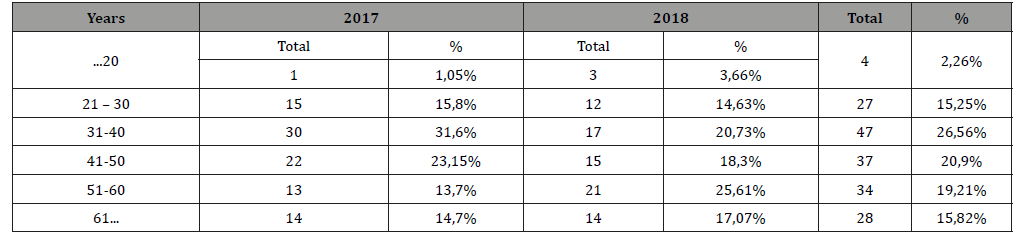
Burlibașa C. in the specialty literature argues that according to the age distribution of patients with odontogenic sinusitis, an increased frequency was found for the age between 26 and 40 years (53.4%) [6,11]. In the same study, Șcerbatiuc D. argues that the average age of patients with maxillary sinusitis is between 30- 50 years [4,12]. According to the 2017-2018 study, the patients most frequently affected by odontogenic maxillary sinusitis were the patients with the age range 31-40 years, the number being 47 patients Table 2 (Figure 2).
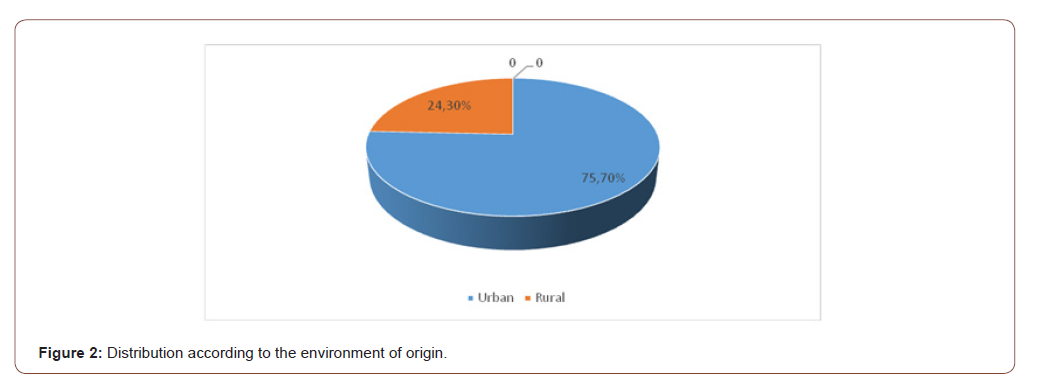
According to the environment of origin Figure 2, in the study group the urban environment prevails with 134 patients (75.70%), followed by the rural environment 43 patients (24.30%). Amărăscu M. also reveals similar data in the study carried out in 2014, namely that the majority of patients with sinus disorders are from urban areas 54.33% and from rural areas 45.67% patients [10] (Table 3).
Table 3: Distribution according to medical insurance.
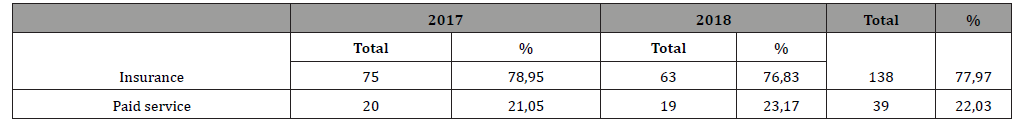
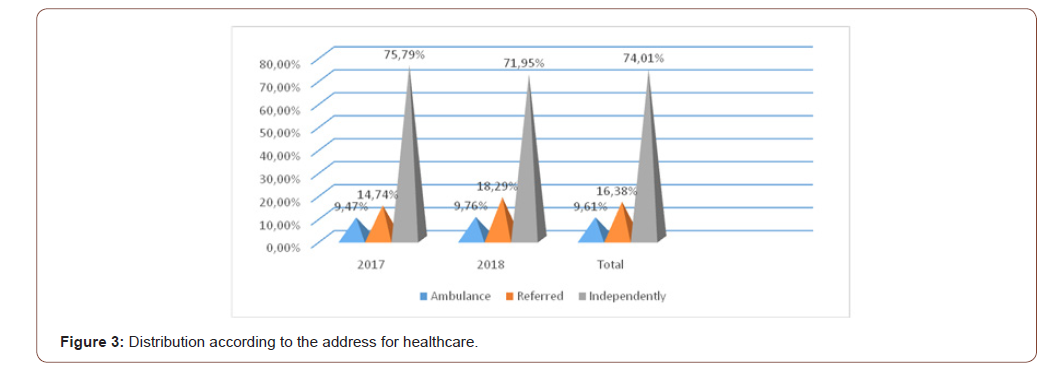
Analyzing the data from Table 3, according to the medical insurance, we observe that the insured patients make up the majority 77.97%, and those against 22.03%. The study conducted by Cazacu C. and the collaborators for 2015 offers data such that persons with compulsory health insurance are 68.8%, against payment 27.95%, and socially vulnerable persons 3.2% [13]. According to the address for the medical assistance during the years 2017-2018 in the study group we observe patients who addressed themselves to the medical institution 131 (74.01%), followed by those with rectification 29 (16.38%), and transported with the ambulance there were 17 (9.61%) patients (Figure 3).
According to data reported by ЕВ Kucherova, the number of patients who addressed the nurse at the medical institution for 2006-2007 was 70.3%, with rectification 23.5%, and those transported by ambulance 6.2% patients [14]. Similar data were obtained in another study where the address of the patients of the self-employed was 57%, with rectification 35.5%, and the ambulance transport 6.5% patients [15] (Table 4).
Table 4: Distribution according to the days of hospitalization.
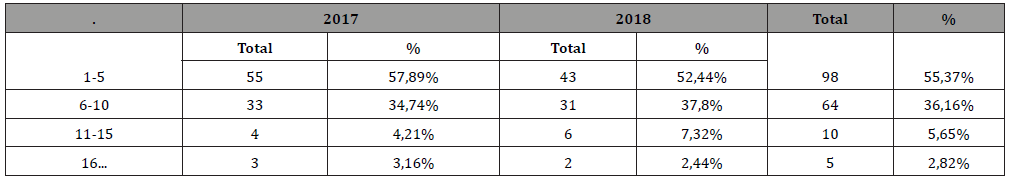
Also the data of the study show that the optimal number of patients who addressed and were hospitalized for 1-5 days was 98 (55.37%) cases, for the forms of sinusitis less complicated, and the patients who were treated from 6 to 10 days constituted 64 (36.16%), followed by those who were hospitalized for 11-15 days was 10 (5.65%) The data provided by Epure V. and al., for 2014 report that the major number of distributions according to the days of hospitalization is 5 days (57.3%) [10] (Figure 4).
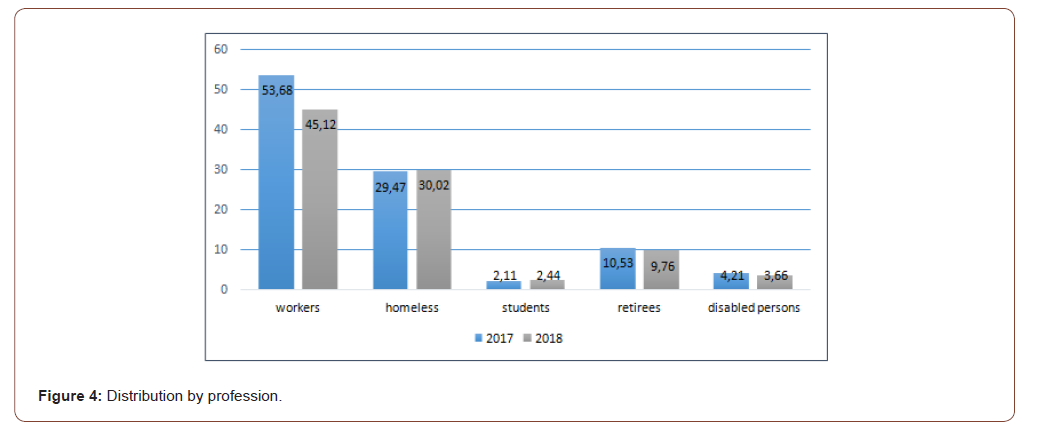
During the years 2017-2018 we observe the prevalence of workers, which constitutes on average 49.72%, followed by the homeless 33.9%, students 2.26%, retirees 10.17% and invalids 3.95%. Similar data were obtained in the research for 2009. The distribution by social categories was as follows: the workers 47.3%, followed by the homeless 31.2%, the students 2.2%, the retirees 8.6% and the disabled persons with 10, 8% of cases [16]. According to the study we deduce that a major cause of maxillary sinusitis is represented by the tumor affections 8.47% followed by the fungal sinusitis with 5.64% and the post-implant sinusitis with 4.51% of the cases (Table 5).
Table 5: Sinusitis distribution according to the etiological factor.
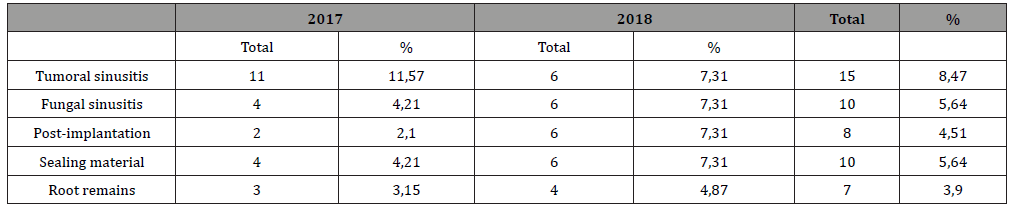
We also find in the work of Hîțu D, where the tumor factor is the cause of sinusitis for 18.5% cases, having the first place [17]. Puglisi S, following the study carried out for 3 years, found: out of 59 patients with chronic maxillary sinusitis 47 were with sinusitis of nonodontogenic origin, and 12 with sinusitis of odontogenic origin, mentioning that in most cases nonodontogenic sinusitis had polymicrobial origin (75%) [18]. Following an analysis by Oscar A. in 2010, regarding 41 articles including 770 cases from 1986- 2007, the etiology of sinusitis was found to be the iatrogenic cause with a frequency of 55.79% of the cases including: complications of periodontitis 40.38%, odontogenic cyst 6.66%, complications following dental extraction 47.56%, oro-sinus communications 19.72%, extrusion of sinus filling materials 22.27%, apicoectomies for 5.33% in some cases, post-implant sinusitis 4.17%, and sinusitis following the implantation of sinuses for 0.92% of cases [19]. According to the retrospective study over two years, we deduce that the most involved causal tooth is the first upper molar for 23.16% of cases, the second upper molar for 7.90% cases, the first premolar for 3.95% cases, the second premolar for 4.01% cases and the third molar 0.56% cases (Figure 5).
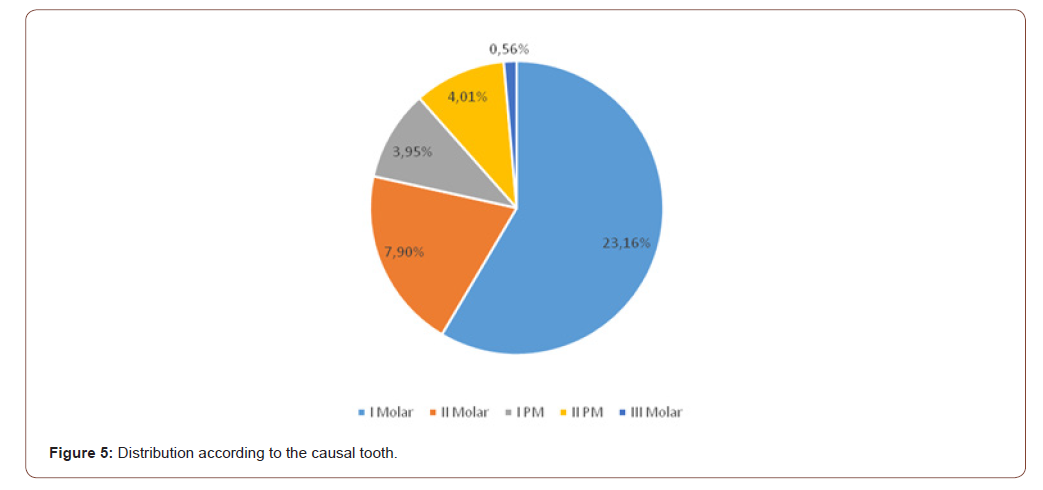
The study carried out by Mighic A on a group of 27 patients diagnosed with odontogenic maxillary sinusitis reports that the most commonly involved causal tooth was the first upper molar in 17 cases (47%), the second molar in 8 cases (22%), the first premolar. in 5 cases (14%), and the third molar in one case (3%) [20]. A study conducted for 2013 on a batch of patients diagnosed with odontogenic maxillary sinusitis reports that from the point of view of the teeth involved in the sinus pathological process, it was noticed that the first molar 1 with an incidence of 55.12%, in the second place there is molar 2 with an incidence of 32.28%, followed by premolars with 25.98 [13] (Figure 6).
According to the study, the most commonly applied method of surgical treatment in odontogenic maxillary sinusitis is the Caldwell- Luc procedure, for 58.75% of cases, followed by COS plastic for 40.67% cases and endoscopic treatment for 15.81%. According to data reported by Ryan E. Little and co-workers in 2018, the treatment method used to treat maxillary sinusitis was endoscopic by 14% of cases [5]. While Guțan A. in the study performed on 70 patients out of which 39 patients with the presence of the oro-antral fistula after dental extractions states that external access is not necessary once the causal factor is removed [21,22]. Hernando J. considers that the sinus mucosa after a chronic inflammatory process of dental cause is no longer treatable and therefore proposes for treatment radical treatment as more effective [23]. Mighic A, after analyzing a batch of 27 patients, established a success rate of 80% starting treatment with the elimination of the causal factor of odontogenic sinusitis, as afterwards the need to apply surgical treatment [20]. Even though the technique of the endoscopic approach compared to the classical one has much more impressive results, especially in order to express the degree of pain and the postoperative edema is approached differently by the specialists [24-36], so based on the information studied and the retrospective study, we affirm that odontogenic maxillary sinusitis has a multifactorial etiology and must be approached according to each case for successful results.
Conclusion
• During 2 years with odontogenic maxillary sinusitis, accounting for 5.48% of the total number.
• The causal tooth was the first upper molar for 23.16% of cases.
• The method of surgical treatment in odontogenic maxillary sinusitis was the Caldwell-Luc procedure for 58.75% of cases.
Acknowledgement
None.
Conflict of Interest
Author declare no conflict of interst.
References
- Ababii I, Popa V, Maniuc M, Antohii I, Sandu A, et al. (2000) Otorhinolaryngology. USMF Polygraphic Medical Publishing Center Chisinau p.340.
- Albu S (2001) Functional surgery of the nostrils. Albu S - Cluj-Napoca pp.45-58.
- Hîţu I, Gasițina A, Hîțu D (2014) Associated facial trauma and sinus lesions, clinical case.13th (Edn.), Bucharest pp.29-30.
- Banuh I, Hîțu D, Șcerbatiuc D, Vlas V, Chihai D, et al. (2010) News in traumatic and infectious lesions of the maxillary sinus. 11th (Edn.), in Scientific Annals of the State University of Medicine and Pharmacy Nicolae Testemitanu, Moldova, 4: 475-479.
- Ryan E Little, Christopher M Long, Todd A Loehrl, Dvid M Poetker (2018) Odontogenic sinusitis: A review of the current literature. Laryngoscope Investig Otolaryngol 3(2): 110-114.
- Timoşca G, Burlibaşa C (1992) Chirurgie oro-maxilo-facială. Chişinău Universitas p.265-298.
- Mortuaire TO, Theis D, Chevalier R, Gengler I (2018) Cost-effectiveness assessment in outpatient sinonasal surgery. Lille France 135(1):11-15.
- Hîțu I, Hîțu D, Pancenco A, Vlas V, Bicer C, et al. (2015) The evolution of perforating sinus lesions. Dental Medicine Chisinau 4(37): 42-45.
- Cabac V, Сastraveț P, Gurbulea G, Găchiuță D, Musteață D (2011) Incidence of chronic sinusitis. 12th (Edn.), Scientific Annals of the State University of Medicine and Pharmacy Nicolae Testemitanu, Moldova, 4: 285-289.
- Epure V, Dan Cristian Gheorghe (2013) Maxilloethmoidal rhinosinusitis. Cronica Editura Pro Universitaria p.183.
- Burlibaşa C (2007) Oral and maxillofacial surgery. Medical Publishing House Bucharest.
- Shcherbatyuk DI (1987) Prevention and treatment of inflammatory diseases of the maxillofacial area. Chisinau Shtiintsa pp.3-34.
- Cazacu C, Cebotari M, Vlas V, Pancenco A, Bicer C, et al. (2013) Early diagnosis and treatment of oro-sinus communication. 13th (Edn.), Scientific Annals 4: 466-469.
- Kucherova EV (2008) Sinusitis Incidence Among the Population of Magadan. GUZ Magadan Regional Hospital p.7.
- Shevrygina BV (1981) Intranasal surgery. Manyuk MK Chisinau: Shtiintsa pp.43-49.
- Hîţu D, Gabriela Cocier, Vlas V (2009) Methods of treatment of sinusitis. Scientific Annals of the State University of Medicine and Pharmacy. 10th (Edn.), Nicolae Testemitanu pp. 512-517.
- Hîţu D (2008) Treatment of odontogenic sinusitis (Theoretical course). Dental medicine 2(16): 243-247.
- Puglisi S, Privitera S, Maiolino L, Agostino Serra, Matteo Garotta, et al. (2011) Bacteriological findings and antimicrobial resistance in odontogenic and non-odontogenic chronic maxillary sinusitis. Journal of Medical Microbiology 60(9): 1353-1359.
- Nimish A Patel, Ferguson Berrylin J (2012) Odontogenic Sinusitis: an ancient but-appreciated cause of maxillary sinusitis. Current Opinion in Otolaryngology and Head Nesk Sugery 20(1):24-28.
- Mighic A (2019) Tratamentul sinuzitei maxilare de origine odontogenă. Medicina stomatologică 4(53): 36-46.
- Guţan A (1989) Lecture on Odontogenic Sinusitis. Chisinau p.18.
- Guţan A (1999) And the collaborators of the department, Stamatological Surgery. Chisinau pp.51-57.
- Hernando J, Gallego L, Junquera L, Villarreal P (2010) Oroantral communications. A retrospective analysis. Mad. Oral. Patol. Oral Cir Oral 5 (3): 499-503
- Feh AR, Robustova TG (2001) Endosurgical approaches to the maxillary sinuses in the experiment. Dentistry 3 Moscow pp.4-6.
- Bădărău Lilia, Daniela Chilari, Munteanu Elena (2019) Maxillary Sinus Injuries of Dental Origin. Statistical Aspects For 2018 Collection of scientific summaries of student’s residents and young researchers. Chisinau p.275.
- Ghicavîi, V, Ghicavîi V, Sârbu S, Şcerbatiuc D, Bacinschii N (2002) Pharmacotherapy of dental diseases. Guide 2nd (Edn.) revised and completed Chisinau, pp. 342-344.
- Hîţu D (2014) Oro-antral communication (Theoretical course). Dental Medicine 3(32): 103-107.
- Hîţu D (2007) Diagnosis of odontogenic sinusitis (Theoretical course). Dental medicine 2: 3-35.
- Hîţu D (2014) Perforated odontogenic maxillary sinusitis (Theoretical course). Dental Medicine 4(33): 20-26.
- Kim SJ, Park JS, Kim HT, Lee CH, Park YH, et al. (2016) Clinical features and treatment outcomes of dental implant-related paranasal sinusitis: A 2-year prospective observational study. Clinical Oral Implants research 27(11): e100-e104.
- Mukovozov NI (1982) Differential diagnosis of HZCHLO. Leningrad Medicine pp.105-112.
- Arias-Irimia O, Barona-Dorado C, Santos-Marino JA, Martinez-Rodriguez N, Mertinez-Gonzalez JM (2010) Meta-analysis of the etiology of odontogenic maxillary sinusitis. Med Oral Patol Oral Cir Bucal 15(1): e70-e73.
- Gutsan AE, Bernadsky I, Godorozha P, Shcherbatyuk D (2001) Handbook of Maxillofacial Operations. Chisinau pp.46-49.
- Rabukhina NA, Arzhantsev AP (2003) Odontogenic diseases of the maxillary sinuses. X-ray diagnostics in dentistry pp.371 -380.
- Robustova TG (2003) Surgical dentistry. Moscow: Medicine pp.359-479.
- Shargorodsky AG (1985) Inflammatory diseases of the cervix and neck. Moscow pp.268-283.
-
Dumitru Hîțu, Nicolae Chele, Vasile Cabac, Alexandru Mighic, Bădărău Lilia. Maxillary Sinusitis of Odontogenic Origin. On J Complement & Alt Med. 6(1): 2021. OJCAM.MS.ID.000626.
-
Maxillary sinus; Odontogenic sinusitis; Frequency of odontogenic infection; Surgical treatment; Pathology
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






