 Review Article
Review Article
Hypnosis as A Complementary Therapy for Promoting Well-Being in Neurodegenerative Disorders: A Review of The Literature
Francesca Vescovelli*
1Department of Psychology, University of Bologna, Bologna, Italy
2Department of Psychology, University of Pretoria, Pretoria, South Africa
Francesca Vescovelli, Department of Psychology University of Bologna, Viale Berti Pichat, 5, 40127 Bologna, Italy.
Received Date: February 03, 2020; Published Date: March 05, 2020
Keywords:
Abstract
Objectives: Hypnosis showed beneficial effects in terms of symptom relief in patients suffering from neurodegenerative conditions. Little is known about the effects of hypnosis on well-being, quality of life and personal resources of these patient populations. This narrative review aimed to summarize and discuss existing studies, which investigated improvements in well-being in patients with neurodegenerative disorders following hypnosis treatment.
Methods: A narrative review was performed in English databases with specific keywords “neurological disease or illness and hypnosis”, “hypnosis and positive psychology” and “hypnosis and well-being”. Eleven studies (with a total of 178 patients) were found which applied hypnosis for neurodegenerative disorders (Parkinson’s disease, Amyotrophic Lateral Sclerosis, Multiple Sclerosis, etc.).
Results: Hypnosis demonstrated beneficial effects, improving patients’ physical well-being and quality of life. Hypnosis was also found to promote existential well-being and resilience.
Conclusions: The majority of studies produced improvement in patients’ well-being. This points to the possibility of applying hypnosis aimed at increasing well-being as a complementary therapy for patients with neurodegenerative disorders. More controlled investigations are needed.
Keywords:Neurodegenerative disorders; Hypnosis; well-being; Embodiment; Relaxation; Complementary therapy
Introduction
Neurological and neurodegenerative disorders are medical conditions that primarily affect the neurons in the human brain, producing a variety of physical and psychological symptoms and complications. They often tend to be progressive, chronic and incurable, seriously hampering patients’ physical and psychological health [1]. Some of the most frequent types of neurodegenerative diseases include Alzheimer’s disease (AD), Parkinson’s disease (PD), Multiple Sclerosis (MS), Amyotrophic lateral sclerosis (ALS), and Huntington’s disease (HD). These disorders comprise of a progressive deterioration of motor neurons and functions and are associated with a variety of unpredictable symptoms, which affect sensory-tactile, motor, visual, bladder, sexual and bowel functioning. These disorders could be disabling and impair patients’ daily functioning. It is therefore important to consider psychological interventions, such as hypnosis, that could represent a complementary promising therapy to address these symptoms and which could also add to patients’ quality of life and well-being [2].
Historically, studies on individuals suffering from neurodegenerative diseases and other chronic conditions were based on a psychiatric and neurological perspective and mainly focused on their possible negative psychological consequences [3-5]. However, the World Health Organization defined health not merely as the absence of disease or symptoms, but as “a state of
complete physical, mental and social well-being” [6]. Consequently, the focus of research on chronic medical conditions started shifting towards also investigating well-being and other related concepts of positive psychological functioning. These themes are the focus of investigation of positive psychology. This relatively new field focuses on the scientific study of those factors that enable individuals to flourish and function optimally [7]. Accordingly, it explores conditions, processes and mechanisms that contribute to well-being and positive psychological functioning. It is important to state that positive psychology does not intend to ignore negative aspects of being human, such as emotional or physical suffering and psychological disorders. Rather, it aims to provide a complementary focus on the positive to allow for a broader understanding of the human experience [8].
Positive psychology theories have been applied both with normal and clinical populations, including individuals with psychological and medical illness in order to gain a more extensive understanding of their psychological experiences [9,10].
FFrom this perspective, it became evident that positive characteristics and resources such as the experience of well-being, positive emotions, gratitude, posttraumatic growth, and meaning may be linked to each other and associated with better psychological adaptation to illness, including neurodegenerative conditions [9-12]. Furthermore, the experience of well-being and positive emotions seemed to positively influence biological parameters involved in the aging process, thereby protecting psychological and physical health both in healthy and clinical populations [9-18].
These dimensions also seem to play a crucial role in the psychological adaptation of patients suffering from neurodegenerative disorders [9,10]. Such disorders may have many disabling consequences, but at the same time, given their lifethreatening nature they may implicate a process of personal growth and the achievement of new existential changes. They could lead patients to experience a personal journey of psychological growth, search for meaning and process of embodiment that may promote their adaptation to the illness [19,20].
Physical illness may be experienced as traumatic events that could produce not only psychological disabilities and symptoms, but often physical and body changes and transformation. The modification of the relationship with one’s body, the physiological processes of the body and the perception of the representation of the body are thus central to adjusting to living with these critical events, and in particular, neurocognitive disease.
Embodiment can be defined as an “awareness of and responsiveness to bodily sensations”, and also as “thoughts, feelings and behaviours that are grounded in sensory experiences and bodily states” [21,22]. The experience of psychological embodiment may allow individuals who suffer from medical illness and neurological disorders to develop greater body awareness. It reflects a process in which individuals could both correctly identify and recognize body sensations and link these body sensations to emotions [23,24]. Body awareness has been linked to subjective well-being within healthy individuals, any may therefore be equally, if not more important, to individuals suffering from neurological conditions [24]. Therefore, interventions, which could support body awareness using the mind-body connection, such as hypnosis, may be useful to these patients.
Research on interventions, conceptualized and implemented from a positive psychology stance, has burgeoned in the past decade. Positive interventions are strategies aimed at promoting positive emotions, thoughts and behaviors, which, in turn, are associated with increased well-being [25]. These empirically validated activities are based on theories of positive psychology. There is increasing evidence that positive interventions could increase wellbeing but also contribute to recovery and relief from pain, distress and psychological symptoms [25,26]. Further, there has been an increased focus on implementing positive interventions in clinical settings and in combination with existing psychotherapeutic strategies, such as cognitive behavioural therapy [27,28]. Hypnosis as therapeutic strategy could also be implemented in the context of positive interventions, through its focus on building positive psychological resources [29,30]. Specifically, hypnosis could potentially be applied to increase positive psychological functioning in the context of medical illnesses, as evident from the large body of research on its application as psychotherapeutic intervention for improving mental and physical health of patients with medical problems [31,32].
In this context, hypnosis could be useful to address patients’ physical symptoms and build personal resources for example through promoting both pain relief [33,34], and well-being [35,36]. Additionally, implementing hypnosis aligned with the goals of positive psychology, that is, to identify and promote individuals’ well-being and psychological resources, may be particularly important in the aftermath of medical illness in general and presence of neurocognitive disorders in particular. However, to our knowledge, there are only a few examples of research that applied hypnosis explicitly to promote well-being from the perspective of positive psychology. These include hypnosis for the treatment of childhood sexual trauma [37], for improving well-being during pregnancy and the post-partum period [35,36], promoting wellbeing of coronary artery bypass patients [38], and patients with pain disorders [34,39].
At the same time, there are some studies which allude to the implementation of hypnosis to improve well-being in medical conditions in general [40,41], and neurodegenerative disorders specifically [2], without explicitly implementing a positive psychology framework. Moreover, Jensen and colleagues state that hypnosis may lead to additional beneficial outcomes [34,42], such as increased well-being, for patients with chronic health conditions. Yet, well-being was not conceptualized as a comprehensive construct, unlike other studies using positive psychology theory [25,35-37].
The aim of this narrative review is to summarize and discuss existing studies, which implemented hypnosis and investigated possible positive experiences, changes and psychological resources reported by patients who suffer from neurodegenerative disorders. This can inform further development of hypnotherapeutic interventions to promote well-being in these patients and to complement their usual medical treatment.
Methods
We performed a narrative review to extract published scientific papers on the use of hypnosis for patients suffering from neurological illness with the aim of improving well-being. Terms such as “neurological disease or illness and hypnosis”, “hypnosis and positive psychology” and “hypnosis and well-being” were introduced in the databases. An electronic literature search on the following databases was undertaken: PubMed, Scopus, Ebsco, and Web of Science. We identified and reviewed the entire crossreferences of articles and book chapters, which described the use of hypnosis for neurological illnesses. Each of these selected articles of interest was entered one by one in the databases. If the database contained the article, a list of all cross-citing articles was created. The list of cross-citing articles was thereafter limited to the English language. No other search method was applied and the full search was conducted including articles from inception to December 2019. The Risk of Bias was calculated for each included study, and the results are presented in Table 1 [43].
Table 1: Table template.
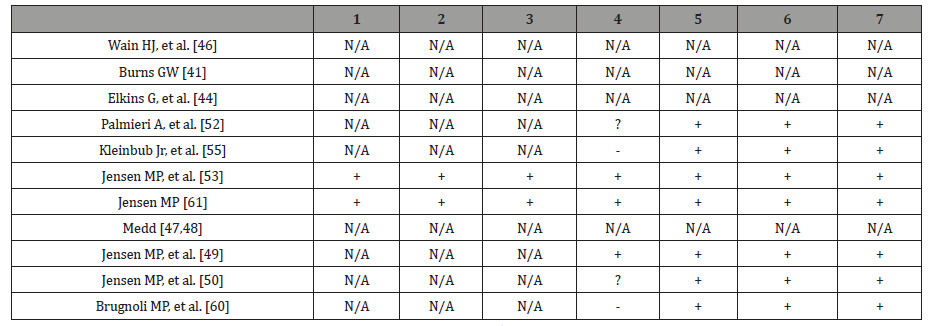
+ = “Low risk” of bias; - = “High risk” of bias; ? = “Unclear risk” of bias; N/A = Not Applicable
1=Random sequence generation (selection bias)
2=Allocation concealment (selection bias)
3=Blinding of participants and personnel (performance bias)
4=Blinding of outcome assessment (detection bias)
5=Incomplete outcome data (attrition bias)
6=Selective reporting (reporting bias)
7=Other bias
To be included in this review, studies were required to a) be full text articles or book chapters published in English; b) be research articles or a clinical case/case report/case series with hypnosis as main intervention; and c) investigate a clinical population with a neurodegenerative condition. Articles were excluded if they were d) reviews; f) meta-analysis; and g) applications of hypnosis for analgesia during surgery.
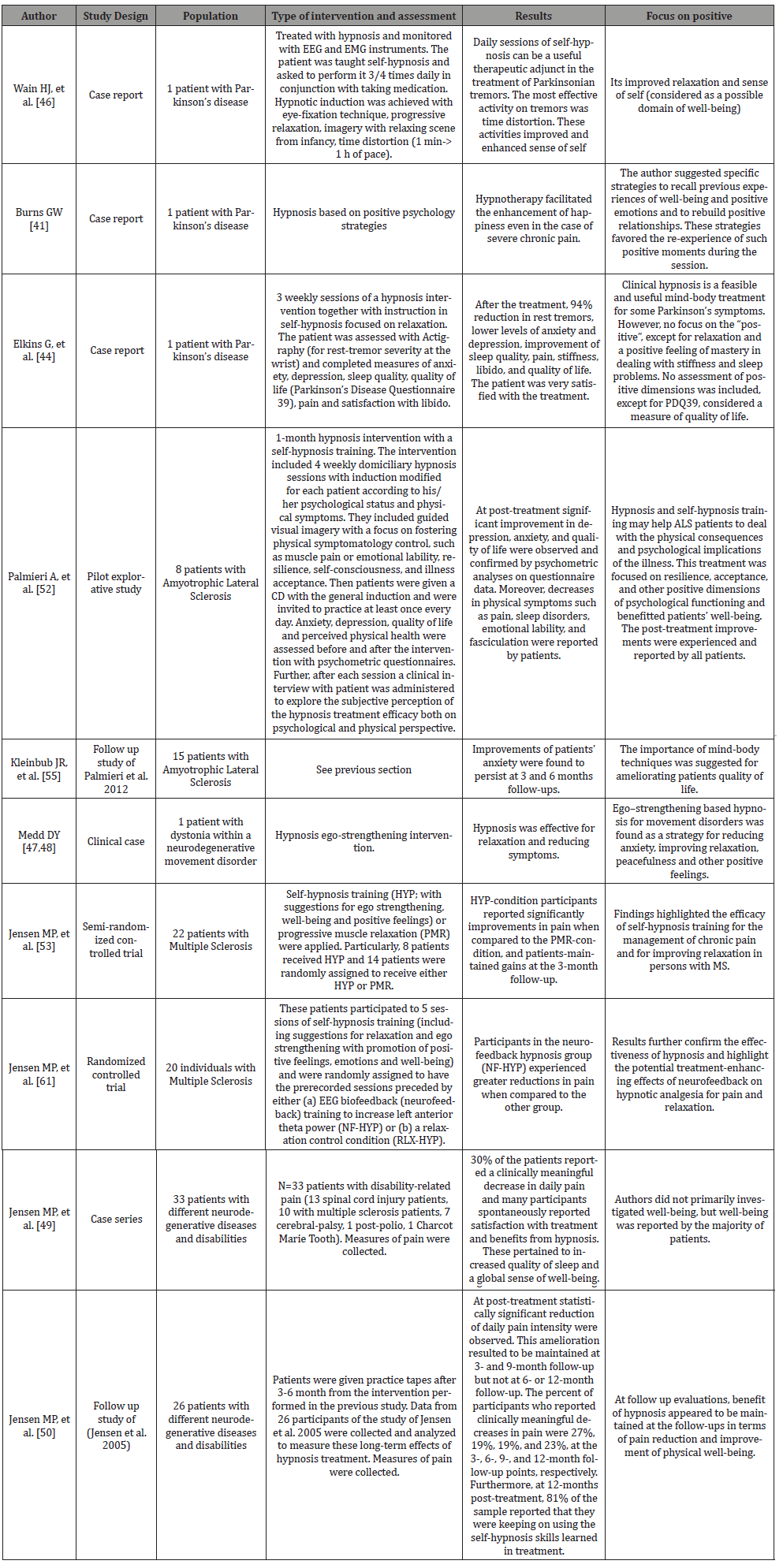
11 articles met all the inclusion criteria, and thus were included in the review. Data were extracted and analyzed using a pre-designed template with the following specified headings: authors, study design, population, type of intervention, results, focus on positive functioning/well-being. These aspects were thus elaborated in the result section and in the table template (Table 2).
Results
Considering previous criteria, 11 articles were included, involving a population of 178 patients with neurodegenerative disorders. Three articles were controlled trials or randomized controlled trials [44,45] whereas the remaining articles were clinical cases (4 articles) [2,39,46,47] or clinical case series (2 articles) [48,49] or explorative studies with no controls [50,51].
In the majority of the studies hypnosis was applied to relieve symptoms and enhance relaxation. Therefore, although hypnosis was not specifically applied from the theoretical framework of positive psychology, the interventions indirectly focused on generating positive emotions and strengthening personal resources. We present results grouped around patient’s diagnosis.
Hypnosis in parkinson’s disease
In the first study [46], applied hypnosis with a patient suffering from Parkinson’s disease. The authors taught the patient how to use self-hypnosis three to four times a day, in conjunction with taking medication. The self-hypnosis intervention included self-hypnotic suggestions, progressive relaxation, imagery using relaxing scenes from childhood, as well as time distortion for experiencing moments of peace. The intervention was useful for reducing tremors, to improve the feeling of relaxation and to enhance a sense of self-identity.
Burns [39] reported on the first application of hypnosis for neurological disorders using the framework of positive psychology. In a case study of a patient with Parkinson’s disease, he described how hypnotherapy could facilitate the enhancement of happiness even in case of severe chronic pain. The author implemented strategies to recall previous experiences of well-being and positive emotions as well as to rebuild positive relationships. Burns also described how the patient could re-experience such positive experiences in the present, leading to increased well-being.
In another recent study treated a 51-year-old male with Parkinson’s disease with 3 weekly sessions of hypnosis and instructions in self-hypnosis [2]. The hypnotic induction and hypnotic suggestions mainly focused on relaxation and reduced about 94% of rest tremors as well as anxiety and depression. It also improved sleep quality, pain, stiffness, libido, and quality of life. Furthermore, the patient was very satisfied with the treatment. The findings from this case study suggest that hypnosis as mindbody intervention, focused on physical relaxation and well-being, could be useful to address physical symptoms of patients with Parkinson’s disease who often do not completely benefit from medication or may even develop disabling side effects.
Hypnosis in amyotrophic lateral sclerosis
Palmieri et al. [50]. implemented a one-month hypnosis intervention, which included self-hypnosis training, with eight patients suffering from amyotrophic lateral sclerosis (ALS). They assessed the patients’ levels of anxiety, depression, quality of life and perceived physical health. Caregivers’ levels of anxiety and depression were also assessed. The hypnotic intervention consisted of 4 weekly hypnotic sessions that were performed at the patients’ home with individualized suggestions and modified according to each patient’s psychological and physical condition. Hypnotic suggestions consisted of guided visual imagery, focused on fostering control over physical symptoms, such as muscle pain or emotional lability, resilience, self-consciousness, and acceptance of illness. These suggestions were recorded and given to the patients who were invited to practice at least once a day (see Jensen et al. for the protocol [44,52]). The authors assessed changes in these aspects of functioning with both self-report and clinicians’ reports. After treatment, depression and anxiety decreased and quality of life improved. Moreover, patients experienced less physical symptoms such as pain, sleep disorders, emotional lability, and fasciculation. Improvements in caregivers’ levels of anxiety also emerged, which they attributed this to the patients’ greater physical and psychological well-being. These positive changes persisted at 3- and 6-months follow-ups, reported in a follow-up study [51]. This pilot study showed how using hypnosis and self-hypnosis, which can be viewed as mind-body strategies, could help ALS patients to deal with the physical consequences and psychological implications of the illness and enhance their quality of life. This was also one of the few studies, which focused on resilience, acceptance, and other positive dimensions of psychological functioning and were beneficial for both the patients’ well-being and, indirectly, for their caregivers. Moreover, the authors reported that there were “positive psychological changes in patients’ quality of life after the training” (p. 4). However, in this study, well-being and positive psychological functioning was also conceptualized as symptom relief (both for patients and caregivers) or as quality of life (for patients). Thus, dimensions such as positive emotions, psychological growth and meaning were neglected in the assessment and in the theoretical background. Finally, the post-treatment positive improvements mainly emerged from qualitative clinical interviews.
Kleinbub et al. [51], in line with the previous research, examined the long-term effect of a brief psychodynamic hypnosis-based intervention on patients with ALS, assessing their psychological, physical symptoms and quality of life and their caregivers were also included. In the study, 15 patients were treated with a hypnosis treatment and self-hypnosis training protocol after a psychological and neurological assessment. Patients’ primary caregivers and 15 matched control patients were also involved in the study. Patients and caregivers completed measures of anxiety and depression while only patients completed measures of quality of life and of functional impairment. This assessment was repeated at the baseline, at post-treatment, and at 3 and 6 months after the end of the intervention. The intervention was partially based on the protocol by Jensen et al. [44,52] and consisted of 4 weekly sessions of hypnosis treatment, articulated in three phases. The first phase focused on hypnotic induction and on mind-body relaxation. In the second phase, therapeutic metaphors were used with guided visual imagery, and personalized suggestions were given. The final phase consisted of anchoring suggestions aimed at teaching self-hypnosis, followed by a guided return to a completely awake state of full consciousness. The four sessions were based on fixed themes. Specifically, in the first session, suggestions were oriented to a safe and quiet place where the patient could allow his own body and mind to rest and recover in deep relaxation. In the second session, the suggestions were focused on developing awareness of thoughts, emotions and calming the sensations of the body. In the third session, the suggestions were directed to the focus on positive memories and their older family members.
The fourth and final sessions, was aimed at eliciting perceptions associated to positive emotions and metaphors. Other suggestions and metaphors were chosen considering each patient’s need, clinical condition, personality and history. Patients were encouraged to practice self-hypnosis at home. Depression and anxiety significantly improved after the treatment. A decrease in patients’ and caregivers’ anxiety as well as caregivers’ depression, were found to persist at 3- and 6-months follow-ups. Functional impairment was lower than that in a control group of patients. In this study, the protocol included relaxation, positive emotions and feelings of mastery in dealing with stiffness and sleep problems. The assessment focused on quality of life. The findings point to the potential of implementing hypnosis to enhance the well-being of patients with ALS.
Hypnosis in multiple sclerosis
JJensen et al. [44] compared the effects of self-hypnosis training (HYP; with suggestions for ego strengthening, well-being and positive feelings) with progressive muscle relaxation (PMR) on pain in 22 patients with multiple sclerosis (MS). Eight patients received HYP and the remaining 14 participants were randomly assigned to receive either HYP or PMR. In HYP-condition, participants significantly reported improvements in pain, when compared to the PMR-condition, and patients-maintained gains at the 3-month follow-up. Although findings highlight the efficacy of self-hypnosis training for the management of chronic pain in persons with MS, no specific focus on well-being and positive feelings was mentioned.
Similarly, Jensen et al. [53] measured the benefits of EEG neurofeedback for increasing responsiveness to self-hypnosis training for chronic pain management in 20 individuals with MS.
These patients participated to 5 sessions of self-hypnosis training (including suggestions for relaxation and ego strengthening with promotion of positive feelings, emotions and well-being) and were randomly assigned to have the pre-recorded sessions preceded by either (a) EEG biofeedback (neurofeedback) training to increase left anterior theta power (NF-HYP) or (b) a relaxation control condition (RLX-HYP). Participants in the neurofeedback hypnosis group (NF-HYP) experienced greater reductions in pain when compared to the other group. Results further confirmed the effectiveness of hypnosis and highlighted the potential treatmentenhancing effects of neurofeedback on hypnotic analgesia. However, no specific description of the achievement of a deeper sense of wellbeing and of more positive emotions was reported.
Hypnosis in groups of patients with heterogeneous neurodegenerative conditions
MMedd [47] applied hypnosis with a patient with long-term generalized dystonia. In this case study, hypnosis was effective for reducing anxiety and pain and for improving the experience of relaxation. However, there was no specific focus on well-being during assessment or treatment. In a subsequent review, Medd applied hypnosis [54], including ego-strengthening techniques, for different movement disorders (Parkinson’s disease, Tourette’s syndrome, and other types of dystonia). The rationale was that these disorders share a common aetiology characterized by dysfunction in the basal ganglia of the brain and decreased or imbalanced levels of specific neurotransmitters. The authors claimed that hypnosis may amplify the effect of symptom relief produced by relaxation. Ego-strengthening hypnotic techniques could improve positive emotions and foster personal resources (and thus wellbeing) of medical patients more effectively than simple relaxation [35-39]. However, the preliminary studies mentioned above did not specifically investigate these variables with appropriate psychometric instruments.
Jensen et al. [34,48] examined the efficacy of hypnosis for pain relief in 33 individuals with disability-related pain through a case series study (i.e., 13 patients with spinal cord injury, 10 patients with multiple sclerosis, eight with cerebral-palsy, one with postpolio syndrome, and one with Charcot-Marie-Tooth disease). Jensen and colleagues found that 30% of the patients reported a clinically meaningful amelioration of daily pain and the majority of them spontaneously experienced satisfaction with and benefits from hypnosis that were not necessarily related to the specific suggestions made in-sessions. These benefits included increased quality of sleep, sense of relaxation, positive mood and sense of well-being, as well as decreased perceived stress. Another major finding was that none of the participants reported adverse events or negative effects from treatment and that therapeutic gains were maintained at 3- and 9-month follow-up. At 12-month follow-up 81% of the sample reported that they continued using the selfhypnosis skills learned in treatment [49]. Even if these benefits were not the focus of the hypnosis interventions they appeared to be related to the intervention. Jensen et al. highlighted that, in spite of an absence of a specific focus on well-being promotion, hypnosis may have the potential for broadening positive effects other than symptom relief. Furthermore, Jensen & Patterson [34] suggested that it is important to include not only measures of pain and symptoms relief in future studies, but also to consider protective positive resources that patients could use for coping with physical pain, such as sense of well-being, positive affect, sense of efficacy and control. This study has important clinical implications, since it indicates to add suggestions specifically aimed at promoting psychological strengths and positive affect when implementing hypnosis in the context of neurodegenerative conditions.
In a follow-up study, Jensen et al. [49] evaluated the long-term outcome of hypnotic analgesia treatment for 26 patients with disabilities (some of those included in Jensen et al. [48]). The aim of the study was to better understand the long-term effects of hypnotic-analgesia treatment and the effects of continued use on those outcomes. Participants of the study of Jensen et al. [48] were approached at 3-6-9-12 month follow-up and were asked about the self-hypnosis practice frequency and about its effects at each of these follow-ups. Some participants (n=11 patients) were provided with tapes of hypnosis inductions and invited to listen to them at least once a day. Data from all of the 26 participants were analyzed to measure these long-term effects of hypnosis treatment. Measures of pain were collected. At post-treatment statistically significant reduction of daily pain intensity were observed. This amelioration resulted to be maintained at 3- and 9-month follow-up but not at 6- or 12-month follow-up. At the 3-, 6-, 9-, and 12-month follow-up points, participants who reported clinically meaningful decreases in pain were 27%, 19%, 19%, and 23%, respectively. Furthermore, at 12-month post-treatment, 81% of the sample reported that they were keeping on using the self-hypnosis skills learned in treatment. Those patients who were given tapes reported greater decrease in pain than those who did not receive tapes. Differently from Jensen et al. [48], no specific mention to physical well-being and positive feelings was reported by authors. However, they conclude that interventions and scripts should be tailored according to each patient needs in order to improve symptom relief and increase the benefits of hypnosis.
Brugnoli et al. [45] performed a nonrandomized clinical trial of integration of clinical hypnosis in palliative care versus standard pharmacological care in patients with severe chronic neurodegenerative diseases. The study wanted to measure whether a long-term intervention of 2 years with clinical hypnosis and self-hypnosis could represent a more effective adjuvant therapy for chronic pain and anxiety, when compared to pharmacological therapy alone. The sample was heterogeneous in terms of diagnosis and out of the 50 patients, only 16 suffered from a neurodegenerative or traumatic condition (e.g., Multiple Sclerosis, Parkinson’s Disease, spinal cord injuries, etc.). Patients were divided into two groups, each with 25 patients suffering from severe chronic illnesses. All of them were treated with standard pharmacological therapy (Opioids, NSAIDS and Corticosteroids) and attended a 2-hour workshop with an expert explaining them the meaning of clinical hypnosis in palliative care for pain and anxiety. Each patient voluntarily decided which group to be enrolled (hypnosis or nonhypnosis). One group received only pharmacological standard treatment, whereas the other group received also adjuvant hypnosis therapy. Hypnosis consisted of self-hypnosis, visualizations, metaphors and relaxing music. The experimental group of patients that participated to hypnosis as an adjuvant therapy reported a significant reduction of pain and anxiety and a significant lower risk of increasing pharmacological pain treatment in the long-term follow-up, when compared to the control group. Authors concluded that clinical hypnosis can be considered an effective adjuvant therapy for pain and anxiety control for patients receiving palliative care. Furthermore, self-hypnosis was so helpful for some patients who reported to have achieved a sense of psychological wellbeing, psychosocial and spiritual healing at the end of their life. Many patients in the hypnosis group referred increased energy, better sleep quality, greater resilience, well-being, self-growth, hope and spirituality. Reaching this sense of inner peace, acceptance and spiritual healing was very helpful for these patients and their families struggling with the proximity to the end of their life.
Discussion
The aim of this narrative review was to summarize and discuss primary studies, which investigated possible positive experiences, changes and resources reported by patients who suffer from neurological disorders after hypnosis treatment. Eleven studies were found on the application of hypnosis for neurodegenerative disorders. Only three of them were controlled studies or clinical trials with control groups. Furthermore, the studies referred to well-being and health, without conceptualizing well-being explicitly or measuring well-being with validated questionnaires. Rather, improvements of well-being after hypnosis were assessed with qualitative interviews or with quality of life indicators or with symptom reduction (e.g., improvements in PDQ39). Moreover, although none of the interventions were primarily focused on increasing well-being, they led to improvement in facets of patients’ well-being. As Guse reported, the potential of hypnosis to enhance well-being was put forward many years before the growth of positive psychology [29,30]. For example, Heap suggested that hypnosis should be included within “growth psychology” rather than “sickness psychology” due to its focus on the promotion of well-being [55]. Only recently did literature on specific hypnosis interventions, based on positive psychology assumptions, start to emerge [29,30,35,36,38,56,57].
The protocol used in most of the 11 studies included in the review applied a sequential ego-strengthening approach with suggestions on relaxation, well-being and positive emotions.
Findings of this narrative review suggest that hypnosis and these “positive” induction have the potential to improve wellbeing of patients suffering from neurodegenerative conditions, going beyond symptom relief. Given the possible impairments that patients with neurodegenerative disorders could experience in emotional well-being (as a primary effect of the illness or as a secondary effect of receiving the chronic diagnosis) [19,20], hypnosis could represent an important complementary therapy for these patients [46]. Many studies showed that hypnosis was helpful in dealing with pain and with other physical symptoms. The beneficial effects of hypnosis may counterbalance the possible lack of effect of the standardized medical treatment or its side effects [2,42].
Many studies considered hypnosis as a mind-body treatment, which could yield beneficial effects in patients suffering from complex form of psychological and psychosomatic symptoms [46]. The protocol of hypnosis described in the present review included a specific focus on relaxation and physical well-being. Therefore, they were able to foster the process of embodiment defined as “awareness of and responsiveness to bodily sensations”. This issue is particularly important in neurodegenerative disorders since these patients struggle with a progressive loss of physical independence and has to deal with significant changes in their physical identity. In fact, in the majority of studies, patients reported to better control and manage tremors, stiffness and other physical symptoms.
The review contributes to existing literature by highlighting the importance of implementing hypnosis not only to relieve distress, but also to enhance positive psychological functioning in patients with neurodegenerative disorders.
Although these promising results, the majority of the studies included in the review presented some methodological limitations. In line with the prevalence of neurodegenerative disorders, studies have very small sample sizes and the samples were very heterogeneous. Studies lack a proper conceptualization of wellbeing and thus did not include standardized and specific measures capable of investigating this construct and positive emotions. The measurement of these positive dimensions should be the target of future studies in order to reach a better standardization of methodological procedures. In addition, future studies should give importance to a more valid method of assessment including both qualitative and quantitative measures. This more comprehensive assessment may help clinicians to better represent patients’ functioning and to develop complementary interventions tailored to each patients ‘peculiar needs.
Conclusion
In conclusion, hypnosis could represent an optimal complementary therapy for neurodegenerative disorders. This review, in fact, highlighted that hypnosis may promote physical well-being and the process of embodiment in these patients. At the same time, as Jensen and Patterson suggested [34], it may exert positive side effects in terms of existential and spiritual benefits, fostering the process of growth, acceptance and resilience. These themes are of extremely importance in chronic and progressive disorders such as the neurodegenerative ones.
More controlled studies are needed to develop and implement specific hypnotherapeutic interventions and protocols, based on well-being promoting strategies.
Acknowledgement
None.
Conflict of interest
Author declare no conflict of interest.
References
- Gao HM, Hong JS (2008) Why neurodegenerative diseases are progressive: Uncontrolled inflammation drives disease progression. Trends Immunol 29(8): 357-365.
- Elkins G, Sliwinski J, Bowers J (2013) Encarnacion E. Feasibility of clinical hypnosis for the treatment of parkinson's disease: a case study. Int J Clin Exp Hypn 61(2): 172-182.
- Martinez Martin P, Leentjens AF, De Pedro Cuesta J, Chaudhuri KR, Schrag AE, et al. (2016) Accuracy of screening instruments for detection of neuropsychiatric syndromes in Parkinson's disease. Mov Disord 31(3): 270-279.
- Peters M, Fitzpatrick R, Doll H, Playford D, Jenkinson C (2011) Does self-reported well-being of patients with Parkinson's disease influence caregiver strain and quality of life. Parkinsonism Relat Disord 17: 348-352.
- Starkstein S, Dragovic M, Brockman S, Wilson M, Bruno V, et al. (2015) The impact of emotional distress on motor blocks and festination in Parkinson’s Disease. J Neuropsychiatry Clin Neurosci 27(2): 121-126.
- World Health Organization WHO Constitution (1948).
- Seligman MEP, Csikszentmihalyi M (2000) Positive Psychology: An introduction. Am Psychol 55: 5-14.
- Pawelski JO (2016) Defining the “positive” in positive psychology: Part I. A descriptive analysis. J Posit Psychol: 1-18.
- Barskova T, Oesterreich R (2009) Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: a systematic review. Disabil Rehab 31(21): 1709-1733.
- Hefferon K, Grealy M, Mutrie N (2009) Post‐traumatic growth and life-threatening physical illness: A systematic review of the qualitative literature. Br J Health Psychol 14(ppt 2): 343-378.
- Mc Cullough ME, Kilpatrick SD, Emmons RA, Larson DB (2001) Is gratitude a moral affect? Psychol Bull 127(2): 249-266.
- Wood AM, Froh JJ, Geraghty AW (2010) Gratitude and well-being: A review and theoretical integration. Clin Psychol Rev 30(7): 890-905.
- Diener E, Chan MY (2011) Happy people live longer: Subjective well‐being contributes to health and longevity. Appl Psychol Health Well Being 3: 1-43.
- Helgeson VS, Reynolds KA, Tomich PL (2006) A meta-analytic review of benefit finding and growth. J Consult Clin Psychol 74(5): 797-816.
- Ruini C, Vescovelli F, Albieri E (2013) Post-traumatic growth in breast cancer survivors: new insights into its relationships with well-being and distress. J Clin Psychol Med Settings 20(3): 383-391.
- Ryff CD, Singer BH, Love GD (2004) Positive health: Connecting well-being with biology. Philos Trans R Soc Lond B Biol Sci 359(1449): 1383-1394.
- Ryff CD (2014) Psychological well-being revisited: Advances in the science and practice of eudaimonia. Psychother Psychosom 83(1): 10-28.
- Steptoe A, Dockray S, Wardle J (2009) Positive affect and psychobiological processes relevant to health. J Pers 77(6): 1747-1776.
- Vescovelli F, Sarti D, Ruini C (2019) Well-being and distress of patients with Parkinson's disease: a comparative investigation. Int Psychogeriatr 31(1): 21-30.
- Vescovelli F, Sarti D, Ruini C (2018) Subjective and psychological well‐being in Parkinson's Disease: A systematic review. Acta Neurol Scand 138(1): 12-23.
- Impett EA, Daubenmier JJ, Hirschman AL (2006) Minding the body: Yoga, embodiment, and well-being. Sex Res Social Policy 3: 39-48.
- Meier BP, Schnall S, Schwarz N, Bargh JA (2012) Embodiment in social psychology. Top Cogn Sci 4(4): 705-716.
- Brani O, Hefferon K, Lomas T, Ivtzan I, Painter J (2014) The impact of body awareness on subjective wellbeing: The role of mindfulness. International Body Psychotherapy Journal 13: 95-107.
- Mehling WE, Gopisetty V, Daubenmier J, Price CJ, Hecht FM, et al. (2009) Body awareness: Construct and self-report measures. PloS One 4(5): e5614.
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, et al. (2013) Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health 13: 119.
- Sin NL, Lyubomirsky S (2009) Enhancing well‐being and alleviating depressive symptoms with positive psychology interventions: A practice‐friendly meta‐analysis. J Clin Psychol 65(5): 467-487.
- Johnson J, Wood AM (2017) Integrating positive and clinical psychology: Viewing human functioning as continua from positive to negative can benefit clinical assessment, interventions and understandings of resilience. Cognit Ther Res 41: 335-349.
- Bannink FP (2014) Positive CBT: From reducing distress to building success. J Contemp Psychother 44: 1-8.
- Guse T (2012) Enhancing lives: a positive psychology agenda for hypnotherapy. S Afr J Psychol 42: 214-223.
- Guse T (2016) Increasing psychological well-being through hypnosis. In Fava GA, Ruini C, eds., Increasing Psychological Well-being in Clinical and Educational Settings. The Netherlands pp. 91-102.
- Elkins G (2016) Clinician's guide to medical and psychological hypnosis: Foundations, applications, and professional issues. New York, USA.
- Yüksel R, Ozcan O, Dane S (2013) The effects of hypnosis on heart rate variability. Int J Clin Exp Hypn 61(2): 162-171.
- Büchi S, Sensky T, Sharpe L, Timberlake N (1998) Graphic representation of illness: a novel method of measuring patients’ perceptions of the impact of illness. Psychother Psychosom 67(4-5): 222-225.
- Jensen M, Patterson DR (2006) Hypnotic treatment of chronic pain. J Behav Med 29(1): 95-124.
- Guse T, Wissing MP, Hartman W (2006) The effect of a prenatal hypnotherapeutic programme on postnatal psychological well-being. J Reprod Infant Psychol 24: 1-15.
- Guse T, Wissing MP, Hartman W (2006) A hypnotherapeutic programme to facilitate postpartum psychological well-being. Australian Journal for Clinical and Experimental Hypnosis 34: 27-40.
- Fourie G, Guse T (2011) An integrated hypnotherapeutic model for the treatment of childhood sexual trauma: A case study. Am J Clin Hypn 53(3): 193-205.
- De Klerk JE, du Plessis WF, Steyn HS, Botha M (2004) Hypnotherapeutic ego strengthening with male South African coronary artery bypass patients. Am J Clin Hypn 47(2): 79-92.
- Burns GW (2009) Happiness, healing, enhancement: Your casebook collection for applying positive psychology in therapy. John Wiley & Sons.
- Pinnell CM, Covino NA (2000) Empirical findings on the use of hypnosis in medicine: A critical review. Int J Clin Exp Hypn 48(2): 170-194.
- Wahbeh H, Elsas SM, Oken BS (2008) Mind-body interventions applications in neurology. Neurology 70(24): 2321-2328.
- Jensen MP, Adachi T, Tomé Pires C, Lee J, Osman ZJ, et al. (2015) Mechanisms of hypnosis: toward the development of a biopsychosocial model. Int J Clin Exp Hypn 63(1): 34-75.
- Higgins JPT, Altman DG, Sterne JAC (2011) Chapter 8: Assessing risk of bias in included studies. In JPT Higgins and S Green (Eds.). In: Cochrane Handbook of Systematic Review of Interventions Version. The Cochrane Collaboration, London, UK.
- Jensen MP, Barber J, Romano JM, Molton IR, Raichle KA, et al. (2009) A comparison of self-hypnosis versus progressive muscle relaxation in patients with multiple sclerosis and chronic pain. Int J Clin Exp Hypn 57(2): 198-221.
- Brugnoli MP, Pesce G, Pasin E, Basile MF, Tamburin S, et al. (2018) The role of clinical hypnosis and self-hypnosis to relief pain and anxiety in severe chronic diseases in palliative care: a 2-year long-term follow-up of treatment in a nonrandomized clinical trial. Ann Palliat Med 7(1): 17-31.
- Wain HJ, Amen D, Jabbari B (1990) The effects of hypnosis on a parkinsonian tremor: Case report with polygraph/EEG recordings. Am J Clin Hypn 33(2): 94-98.
- Medd DY (1999a) A single-case study of generalized dystonia and hypnosis, with unexpected immobility and an untoward effect. Contemp Hypn Integr Ther 16: 45-48.
- Jensen MP, Hanley MA, Engel JM, Romano JM, Barber J, et al. (2005) Hypnotic analgesia for chronic pain in persons with disabilities: A case series abstract. Int J Clin Exp Hypn 53(2): 198-228.
- Jensen MP, Barber J, Hanley MA, Engel JM, Romano JM, et al. (2008) Long-term outcome of hypnotic-analgesia treatment for chronic pain in persons with disabilities. Int J Clin Exp Hypn 56(2): 156-169.
- Palmieri A, Kleinbub JR, Calvo V, Sorarù G, Grasso I, et al. (2012) Efficacy of hypnosis-based treatment in amyotrophic lateral sclerosis: A pilot study. Front Psychol 3: 465.
- Kleinbub JR, Palmieri A, Broggio A, Pagnini F, Benelli E, et al. (2015) Hypnosis-based psychodynamic treatment in ALS: a longitudinal study on patients and their caregivers. Front Psychol 6: 822.
- Jensen MP (2011) Psychosocial approaches to pain management: an organizational framework. Pain 152(4): 717-725.
- Jensen MP (2016) Use of neurofeedback to enhance response to hypnotic analgesia in individuals with multiple sclerosis. Int J Clin Exp Hypn 64(1): 1-23.
- Medd DY (1999b) Hypnosis with selected movement disorders. Contemp Hypn 16: 81-86.
- Heap M (1988) Hypnosis: current clinical, experimental and forensic practices. London: Croom Helm.
- Ruysschaert N (2009) (Self) hypnosis in the prevention of burnout and compassion fatigue for caregivers: Theory and induction. Contemp Hypn 26: 159-172.
- Yapko MD (2012) Trancework: An introduction to the practice of clinical hypnosis.
-
Francesca Vescovelli, Chiara Ruini, Tharina Guse. Hypnosis as A Complementary Therapy for Promoting Well-Being in Neurodegenerative Disorders: A Review of The Literature. On J Complement & Alt Med. 3(4): 2020. OJCAM.MS.ID.000569.
-
Complementary therapy, Neurodegenerative disorders, Positive psychology, Parkinson’s disease, Lateral Sclerosis, Multiple Sclerosis, Hypnosis; Well-being, Embodiment, Relaxation, Human brain
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






