 Review Article
Review Article
Fall Prevention Efforts in Hospitals
George G Couch, Assistant Professor, Department of Health Care Management, USA.
Received Date: August 03, 2019; Published Date: September 11, 2019
Introduction
Falls are deadly and costly events in health care facilities and have become a primary focus of most hospital quality improvement programs. Falls can occur to patients with simple medical problems as well as those with more complex diagnosis and treatment. From the emergency room, intensive care unit, general inpatient floor to outpatient settings falls can turn a routine patient care encounter into a complicated matter with potential for significant mortality, cost, morale, quality, and public image repercussions. Falls can result in no or minimal harm with injuries ranging from scrapes, bumps, and bruises up to lengthened, expensive, and stressful patient stays for significant injuries or may even result in traumatic death. Falls among hospitalized patients occur frequently and some repeatedly. Of those who fall, 28% have bruises and minor injuries, 11.4% have severe soft tissue wounds, and 5% have fractures. An additional 2% have head trauma, which can lead to a subdural hematoma, long-term disability, or death [1]. Evidence supports the need for interventions aimed at reducing the risk of falls and decreasing the number and severity of falls events. The Collaborative Alliance for Nursing Outcomes and the National Data Base of Nursing Quality Indicators have identified falls as a primary nursing quality indicator. In 2005 The Joint Commission added requirements that both acute and long-term care facilities assess and periodically reassess patients for risk of falls. In 2006 the Centers for Medicare and Medicaid Services [2] identified falls as “never events”, which are defined as serious, preventable and costly medical errors with the potential for death. CMS proposed and promoted strategies to prevent and reduce falls to lower the incidence of “never events” [2].
Aims
This review focuses on three objectives; 1) to review various interventions and evaluate their effectiveness in hospital settings with the primary outcomes of interest on the evaluation of reduction or no reduction in patient falls and fall-related injuries; 2) to determine what characteristics of applied interventions or underlying principles of the approaches to falls reduction are attributable to the observed outcomes in hospital settings; and 3) to determine if findings from this literature review can lead to a model and practical framework for hospital leaders to implement a fall prevention strategy based upon changes in care processes, physical environment, equipment, training, culture or technology.
Method
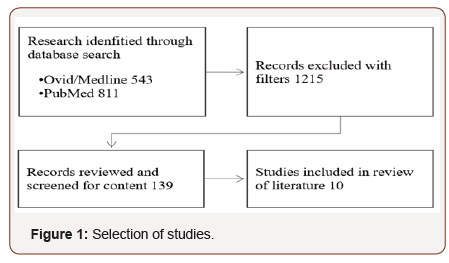
A peer-reviewed literature search was conducted within the electronic databases of Ovid/MEDLINE and PubMed. The search strategy used the following terms or combination of terms including: “patient falls,” “hospital patient falls,” “falls prevention” and “falls risk factors”. Searches were conducted with a primary focus on articles published from 2011 to current 2018. Focus was on articles with research conducted in general acute care hospitals; with qualitative or quantitative study design; on patients 18 and older. 1,354 articles contained some or all the critical components of this search, and after applying filters for age, setting, interventions, published and peer-reviewed studies the search was narrowed down to 139 articles. Abstracts or initial introductions of each of these articles were reviewed with a focus on selecting ten articles which had significant relevance and satisfactory content to be included in this review (Figure 1).
Intervention characteristics
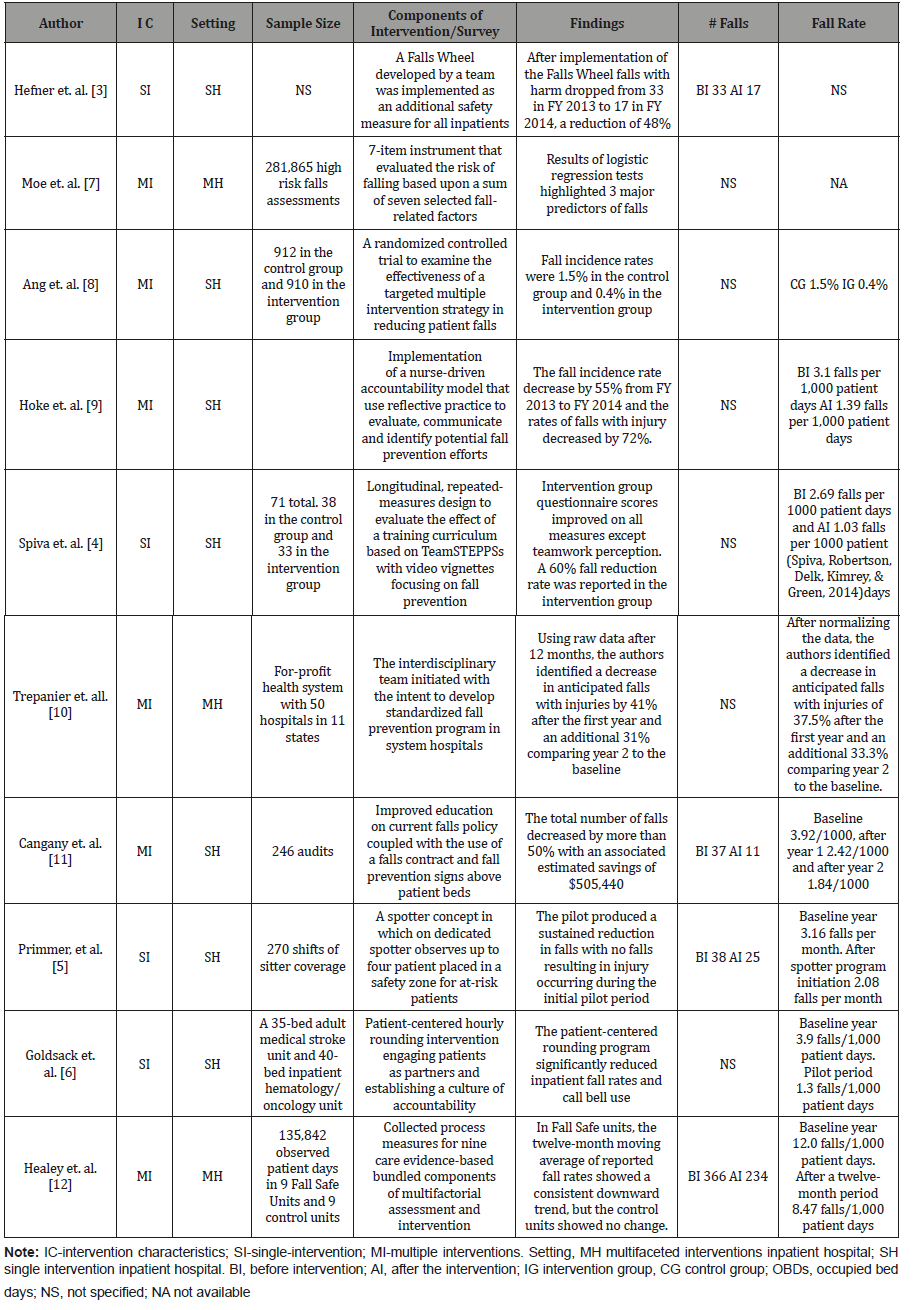
Fall prevention interventions take on many forms and designs. Conducting patient falls risk assessments to identify patients who are most likely to fall followed by the development and implementation of an individualized care plan to reduce the likelihood of a patent fall was common among all settings and studies. Formal risk assessment tools commonly cited in the reviewed literature included the Morse Fall Scale (MFS), St. Thomas Risk Assessment Tool in Falling (STRATIFY), the Conley Scale and the Hendrich Falls Risk Model II (HFRM II). Of the ten studies selected for the review, six utilized multiple interventional methods to address the general consensus that falls have been shown by research to be predominately multifactorial, complex and interrelated and typically due to a combination of individual and transient risk factors including physical environment, patient behavior, medications, physical and mental condition [1]. The other four studies selected focused on single intervention designs. It is important to note all these designs included the use of a patient assessment prior to the application of the intervention to assure the patient’s fall risk profile might benefit from the single intervention. These four single interventions included a unique approach with a “Falls Wheel” Hefner JL, et al [3]designed to provide viewers with information at the bedside via a multi-layer wheel which provided tailored interventions based upon four risk categories ranging from Low Fall/Low Injury Risk to High Fall/High Injury Risk. Other interventions reviewed included: targeted multiple intervention strategies; nurse-driven accountable models; the Team STEPPS video vignette-based staff training model focusing on fall prevention; an education program that included a falls contract and falls prevention sign; the use of human “spotters” to monitor groups of high risk patients; hourly rounding with high patient engagement and bundled components of multifactorial assessments and interventions.
Settings
The analysis included identification of the settings in which the interventions were implemented and studied. Predominately the research was conducted in single inpatient hospitals (SH) which likely produced generally accepted controls but in which certain biases or patient characteristics might have affected outcomes. In seven of the ten articles reviewed, the research was conducted within a single hospital setting, though most often on specific patient units rather than hospital wide. The second setting reviewed included multifaceted interventions within several related inpatient hospitals (MH) or in a select geographic area. The large size and populations in these studies were likely to produce a larger sample with potentially higher validity and less bias, but likely less control. Three of the ten studies selected (Table 1) were conducted in the MH setting, and these were predominately in hospitals owned by a single system or with an intervention deployed over multi-hospital locations.
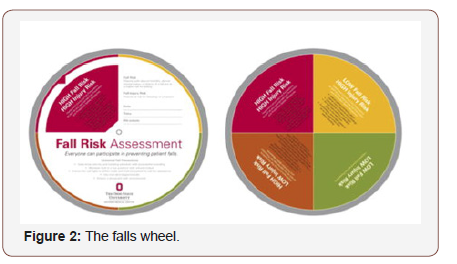
Table 1: Overview of studies included in the review.
Single intervention strategies
Generally, past studies on fall prevention have focused on assessments and multiple strategies in identifying patients at risk and preventing falls. However, some researchers have attempted to develop and implement falls prevention and reduction strategies using one primary intervention is associated with the determination of risk by initial assessment and then attempted to measure and evaluate the outcome of these single strategies. The following were the four unique single intervention strategies identified in the articles selected for this review. A Falls Wheel was developed Hefner JL, et al [3] by a team of patients, family members and health system leaders in a large system comprised of five hospitals affiliated with a large mid-western university. The Falls Wheel (Figure 2) consists of a top layer circle instructing viewers that Universal Fall Precautions should be implemented for all patients. The top wheel has a cut-out quadrant that, when turned, provides patient information about one of four specific falls risks categories (from lowest to highest risk) then guides which additional safety measure are in specified for the patient’s coded falls risk status. A novel element of this tool is that the four risk categories allow for the personalization of the risk of fall and risk of injury. Staff training was incorporated with the Falls Wheel along with daily reporting of falls activity.
The second method reviewed was TeamSTEPPS Spiva L, et al. [4] which is a training curriculum centered around video vignettes focusing on fall prevention. In this study, TeamSTEPPS included a master trainer, and two clinical nurse leaders knowledgeable in fall prevent strategies. TeamSTEPPS focused on building skills in four domains of communication, situational monitoring, mutual support, and leadership. Two training session of 30 minutes each were conducted with didactic training centered around customdesigned patient scenarios. The first training session demonstrated poor teamwork related to fall prevention, and the second session covered communications and situational monitoring with patient handoffs and safety huddles. A third video vignette session covered mutual support, leadership along with a review of Team STEPPS domains and selected tools related to fall prevention. The study was conducted at two acute care hospitals located in the southeast United States on four medical-surgical acute care units. Two of these units served as control groups, and the other two units functioned as intervention groups with similar bed sizes and patient groups.
The third innovative program involved educating unlicensed assistive personnel (UAP) to act as Safe Patient Observation Technicians, or “spotters” assigned to high falls risk patients that were grouped in safety zones [5]. The program was created by a nursing team and piloted on a 43-bed medical-surgical unit in a 649-bed general medical and surgical teaching hospital with a high percentage of older adult patients, then expanded to other units of the facility with large concentrations of patients classified as high risk. The final single strategy intervention was a more typical and common strategy centered around hourly rounding [6]. The intervention was designed collaboratively by clinical nurses, pharmacist, physician, physical therapist, process improvement expert, a researcher and nurse leaders around three core principals; 1) avoiding redundancy with existing strategies; 2) engaging patients as active partners; and 3) establishing a culture of accountability coupled to the strategy with staff buy-in. This study was conducted in two medical units in a 907-bed hospital in Newark, Delaware.
Multiple intervention strategies
In more contemporary and widespread approaches toward understanding the cause and evaluating methods to reduce the frequency and severity of falls are multiple intervention strategies. Six of these strategies were identified and selected for this literature review. In the first a large study of 218,865 high risk falls assessments was conducted using a 7-item instrument that evaluated the risk of falling based upon the sum of these seven fall-related factors that included: falls in the last 6-months, age, mental status (confused or not confused), elimination status (either frequent toileting or presence of urgency), mobility issues (mobility issues or requiring assistance), medications taken and a nurses clinical judgement score ranging from 0 to 10 [7]. High scores were considered to demonstrate an increased risk of falling with a score of 13 or more deemed as putting a patient at high risk of falls. The second selected multiple intervention strategy in reducing falls for patient identified as high-risk fallers was trialed at an acute care hospital in Singapore in which two interventions (targeted multiple interventions with usual care versus usual care only) were conducted with patients identified as high-risk for falls over eight months with 912 patients in the control group and 910 in the intervention group. This sample size was an effort to achieve a 95% CO of 1.4-2.8% [8]. In this case study, Registered Nurses performed routine assessments of participants within four hours of admission using the Henrich II Fall Risk Model.
The third multiple intervention study was of an intermediate cardiac unit (CICU) in a large university hospital in Pennsylvania, which had experienced a 41% one-year increase in falls. A cohort of four clinical nurses identified that the majority of the falls occurred when patients were unassisted by nurses most often during toileting [9]. The cohort developed an accountability care program requiring nurses to use reflective practice to evaluate each fall. This practice included sending an e-mail to all CICU staff members with both the nurse’s and the patient’s perspective on the fall accompanied by the nurse’s reflection on what could have been done to prevent the fall. Other program components were post-fall huddle and guidelines for assisting and remaining with fall risk patients during the duration of their toileting. A fourth large study was conducted across a 50 acute care for-profit hospital system in 11 states over a two-year period [10]. The performance improvement team focused on a single goal: to decrease the number of anticipated falls with injuries. Their standardized program was evidence based on literature and expert reviews. From this research a program was developed that included; a policy and procedure with a minimum set of standards; falls identification safety tools; a sample post-fall assessment; implementation of a “stop the line” concept when a fall occurs; hourly rounding education tool and log; room observation form; decision-making algorithm for sitter usage; educational material for the caregivers, patients and significant others; commitment standards for health care providers; bed safety instructions; physical therapy evaluation process; audit tools; and a sample handoff communication tool. Another evidence-based approach was the fifth selected and conducted at a 30-bed, medical progressive unit (PCU) in a 200-bed Midwest hospital [11]. The title of the project was “No Fall Zone” with the objective to determine if improved education on the current falls policy coupled with a fall contact and falls prevention signs placed on the ceiling above patient’s beds would decrease the overall number of falls. The education program centered around a 40-minute video developed to reenact a real-life fall of a patient resulting in harm. The video included details of the chain of events leading up to the fall and the harmful consequences of a fall from the patient and the patient’s family perspective. The video’s second half demonstrated steps and interventions which could have been taken through the various stages of the incident’s progression showing how each failed event could have been properly handled.
The final multiple intervention strategies reviewed was an 18-month study of the Fall Safe quality improvement project that studied the outcomes of nine Fall Safe nursing units to nine control nursing units [12]. Fall Safe is described as a lead collected process measure for nine care bundle components conducted on 20 patients, per unit, per month using formats that define collection methods and evidence of compliance. The nine care bundle components evaluated included: 1) call bell in sight and reach; 2) cognitive screen; 3) asked about fear of falling; 4) history of falls; 5) laying and standing blood pressure; 6) medication review requested; 7) dose of night sedation NOT given last night; 8) safe footwear on feet; and 9) evidence of urine dip-test taken and recorded.
Results
All ten of the fall intervention programs resulted in an important or sizeable reduction in falls or falls-related injuries (Figure 3). However, due to the multi-faceted nature of the interventions it is difficult to isolate the effect of an individual intervention to determine which component of the intervention contributed to associated outcomes (a measureable reduction or no reduction in falls) of each approach.
A review of the rates reported in each study is shown in (Figure 3). The most significant reduction was a 66.67% reduction in the fall rate per 1,000 patient days experienced in the study, which focused on hourly rounding [6]. The lowest reported decrease in standard patient care unit was 34.18% Primmer p, et al. [5] which relied on a minimum of one “Spotter” per four patients with identified falls risk in a common area. However, it was this “Spotter” study which reported a sustained reduction in falls with no falls resulting in injury occurring during the initial trial period when “Spotters” were in active use.
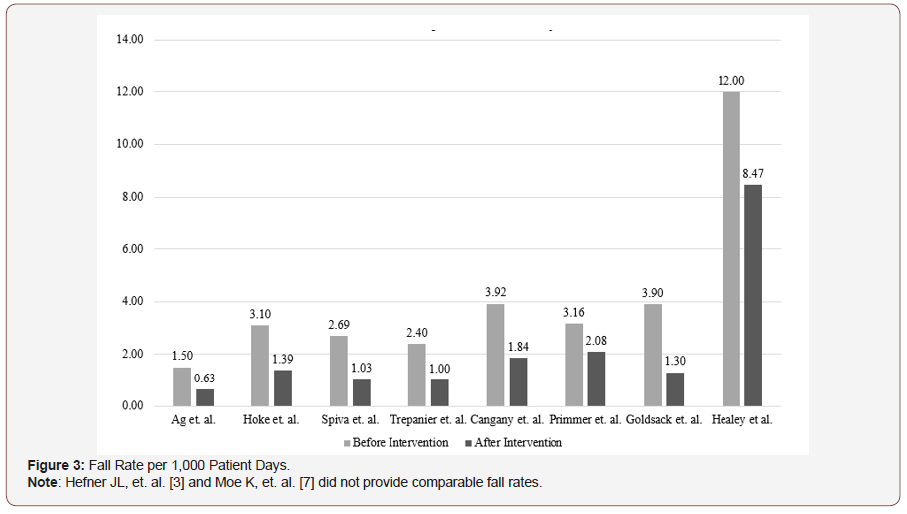
The Healey study Healey F, et al. [12] appears to be an outlier, but the larger before intervention rate of 12.0 falls per 1,000 patient days and the after intervention rate of 8.47 falls per 1,000 patient days is the result of a study conducted on patients who were previously identified and grouped as high fall risk patients on highrisk Fall Safe units. Therefore, one could objectively concur that the fall reduction of 29.42% experienced on this unit is meaningful in this high-risk population. Two studies, the Falls Wheel approach Hefner JL, et al. [3] and 7-instrument fall risk evaluation Moe K, et al. [7] did not provide falls rates per 1,000 patient days, but both reported promising results. The Falls Wheel approach reported a one-year reduction in falls with harm from 33 events to 17 events or a 48% reduction. Whereas the 7-instrument instrument study identified three major predictors for falls with the conclusion that patients who have fallen within the last six months are 2.98 times more likely to fall in the hospital in the future; if confused 2.05 times more likely to fall in the hospital in the future and if taking a laxative are 1.54 times more likely to fall in the hospital in the future.
Discussion
Based upon the literature search, review and selection hospitals focusing on reducing the frequency, severity, and risk of falls have many evidence-based interventions and a variety of approaches to explore when considering the implementation of new falls reduction protocols and practices. In the selection and analysis of these ten research studies hospitals employ two broad strategies at fall prevention and reduction with the implementation of care processes and technological methods. A third strategy commonly utilized is the modification of the patient environment. In all cases reviewed the caregiver and, to a more limited extent, the family became essential parts of the identification of patient fall risks, patient observation for falls prevention and intervention structure through education and training.
Strengths and limitations
Though an in-depth analysis is not possible in a literature review of this scope the analysis did identify a wide range of currently available interventions and approaches to falls reduction that might prove beneficial to hospitals and other health care organization looking to reduce falls and the related implications for patients, patient families, staff and the organizations. The search strategy did not use a more extensive and selective process by which to review and evaluate articles considered for inclusion and exclusion, which likely limited the depth and value of this literature review.
Implications for research
The need for more extensive investigation with varied approaches and techniques both known and those not yet explored in methods of falls reduction indicates the need for additional funded research. Even with these and hundreds of other major research efforts into reducing falls the Joint Commission [13] as recently as 2015 identified the continued significant ongoing threats of falls to patient safety:
i. Every year in the United States, hundreds of thousands of patients fall in hospitals with 30-50 percent resulting in injury.
ii. Injured patients require additional treatment and sometimes prolonged hospital stays. As an example, one study of fall with injury indicated such incidents added 6.3 days to the hospital stay.
iii. The average additional cost for a fall with injury is about $14,000.
Without question, research into falls reduction will remain a significant concern and area of investigation in the health care profession.
Conclusion
Based upon these studies and the reports of the Joint Commission and regulatory and research organizations, hospitals have historically tried to reduce falls and, to some extent have succeeded, but a significant and sustained reduction has proven elusive. The wide variety of potential intervention strategies does not appear to be leading researchers to a best practices model which could be universally deployed with consistent and cost-effective results across the varied hospital settings. Falls are best described as generally unpredictable with many variables known and unknown. An unfortunate conclusion is that falls are not universally preventable currently to any level of consistency, regardless of cost or effort. A less formal and basic statistical conclusion may be that hospital and hospital units that deploy formalized methods of patient fall assessment, staff training, family education, and management commitment are likely to see a meaningful decrease in the frequency of patient falls and injuries from these falls ranging from +/-29.4% to +/-66.67%. Hospitals with a lack of effort or commitment to formalized falls reduction programs are likely to experience a high frequency of patient falls and falls with injury. Falls resulting in minimal to significant harm, the related potential costs of increased penalties, the loss of performance incentives along with increased litigation and settlement costs are likely to result if it can be demonstrated that a hospital organization did not take reasonable steps to minimize or prevent the well-known, researched and documented safety threat of anticipated and unanticipated falls to patients.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Spoelstra SL, Given BA, Given CW (2012) Falls Prevention in Hospitals: An Integrative Review. Clin Nurs Res 21(1): 92-112.
- Centers for Medicare and Medicaid Services (2006) CMS.gov.
- Hefner JL, Mc Alearney AS, Mansfield J, Knupp AM, Moffatt Bruce SD (2015) A Falls Wheel in a Large Academic Medical Center: An Intervention to Reduce Patient Falls with Harm. J Healthc Qual 37(6): 374-380.
- Spiva L, Robertson B, Delk ML, Patrick S, Kimrey MM, et al. (2014) Effectiveness of Team Training on Fall Prevention. J Nurs Care Qual 29(2): 164-175.
- Primmer P, Borenstein KK, Downing MT, Fochesto D, Reilly L, et al. (2015) Reducing falls with a safety spotter program. Nursing 45(8): 16-19.
- Goldsack J, Bergy M, Mascioli S, Cunningham J (2015) Hourly rounding and patient falls: What factors boost success? Nursing 45(2): 25-30.
- Moe K, Brockopp D, Mc Cowan D, Merritt S, Hall B (2015) Major Predictors of Inpatient Falls. J Nurs Adm 45(10): 498-502.
- Ang E, Zubaidah Mordiffi S, Bee Wong H (2011) Evaluating the use of a targeted multiple intervention strategy in reducing patient falls in an acute care hospital: a randomized controlled trial. J Adv Nurs 67(9): 1984-1992.
- Hoke LM, Guarracino D (2016) Beyond Socks, Signs, and Alarms: A Reflective Accountable Model for Fall Prevention. Am J Nurs 116(1): 42-47.
- Trepanier S, Hilsenbeck J (2014) A Hospital System Approach at Decreasing Falls with Injuries and Cost. Nurs Econ 32(3): 135-141.
- Cangany M, Back D, Altman M, Hamilton Kelly T, Lacey S (2015) Bedside Nurses Leading the Way for Falls Prevention: An Evidence-Based Approach. Crit Care Nurse 35(2): 82-84.
- Healey F, Lowe D, Darowski A, Windsor J, Treml J, et al. (2014) Falls prevention in hospitals and mental health units: an extended evaluation of the Fall Safe quality improvement project. Age Ageing 43(4): 484-491.
- The Joint Commission (2015) Sentinal Event Alert - Preventing falls and fall related injuries in health care facilities. Sentinel Event Alert (55): 1-5.
-
George G Couch. Fall Prevention Efforts in Hospitals. On J Complement & Alt Med. 2(1): 2019. OJCAM.MS.ID.000530.
-
Health care, Diagnosis, Treatment, Patient, Stressful, Traumatic death, Fractures, Disability
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






