 Research Article
Research Article
Efficacy of Automated Text Messaging Services on Sleep Health, Stress, Pain, and Function in Physical Therapy Patients
Ashley Pfeiffer1*, Craig Triplett1, Alissa Anderson Call2, Daesha Erskin1 and Hannah Hirschi1
1Department of Exercise Science, Black Hills State University, Spearfish, USA
2Department of Psychology Black Hills State University, Spearfish, SD, USA
Ashley Pfeiffer DPT, 1200 University Street, Unit #9405, Black Hills State University, Spearfish, SD, 57799.
Received Date:October 21, 2022; Published Date:November 30, 2022
Abstract
Purpose: Physical therapy (PT) patients have been shown to have greater sleep disturbances and poor sleep hygiene compared to the general population. Automated text messaging has emerged as one possible strategy to assist with improving sleep hygiene. The purpose of this study was to trial sleep hygiene education for improving PT patients’ sleep through the use of daily automated text messaging.
Methods: Adult PT patients completed an electronic survey consisting of five questionnaires: Pittsburgh Sleep Quality Index (PSQI), Sleep Hygiene Index (SHI), Patient Specific Functional Scale (PSFS), Perceived Stress Scale (PSS), and the Numeric Pain Rating Scale (NPRS). Participants were randomly assigned into groups. The intervention group received PT services along with daily text messages on sleep hygiene tips. The control group only received PT services. At the end of four weeks, questionnaires were repeated.
Results: A marginally significant difference was seen between conditions on the PSQI, F(1, 20) = 4.11, p = .056, np2 = .17. A significant effect difference between time of testing was seen on the SHI scale. F(1, 20) = 8.15, p = .010, np2 = .29, and the PSFS scale, F(1, 20) = 20.97, p < .001, np2 = .58.
Conclusions: The intervention group was trending towards significance on the PSQI, suggesting improved sleep quality. Improvements were seen in sleep hygiene and overall function over the four weeks regardless of group assignment. It appears automated text messaging is a means to increase sleep function in PT patients, a larger sample size would confirm this finding.
Keywords:Sleep Hygiene; Physical Therapy; Automated Text Messaging
Abbreviations:RT: PT: Physical therapy; PSQI: Pittsburgh Sleep Quality Index; SHI: Sleep Hygiene Index; PSFS: Patient Specific Functional Scale; PSS: Perceived Stress Scale; NPRS: Numeric Pain Rating Scale
Introduction
Poor sleep is a major problem in the United States that may impact overall health and quality of life. Many adults do not get the recommended 7 to 9 hours of sleep, with 35.2% of adults reporting sleeping on average less than 7 hours a night [1]. Individuals who get less than 7 hours of sleep per night are classified as short sleepers and have been found to have chronic health conditions in addition to being more likely to be obese, smoke, and be physically inactive in comparison to those who get an adequate amount of sleep [2].
Past research has shown that many individuals experience some form of sleep related problem and overall poor sleep quality. Emerging research suggests a higher prevalence of these sleep disturbances in outpatient physical therapy (PT) patients compared to the general population [3]. The findings suggested that 80% of participants reported poor sleep quality and greater than 50% reported poor sleep hygiene and insomnia. Results also demonstrated that increased pain intensity was correlated with worsening sleep quality [3]. These outcomes highlight a need for sleep health education in this population.
There is a limited amount of literature on the topic of sleep interventions within the PT outpatient clinical setting. A recent systematic review and meta-analysis performed on the effects of exercise related PT interventions on sleep disorders in patients diagnosed with neurological diseases showed promising results [4]. Atlas and Demirdal examined the effect of PT modalities on pain, sleep, mental status, and quality of life compared to regular exercise in patients with osteoarthritis [5]. Results indicated the PT intervention made a significant difference on pain, sleep, mental status, and quality of life. These results suggest that there may be a possible use for PT services in the aid of improving sleep health, function, and overall quality of life [5].
Various interventions have been used to assess behavioral changes surrounding sleep [6-17]. Text messaging has the potential to be an effective tool when it comes to behavior change related to sleep in healthy college students [18]. Automated text messaging is an efficient and inexpensive method of delivering support in various health related topics to induce behavior change resulting in better function, reduced pain, and improved quality of health [18-20]. The researchers of the current study hypothesized that patients receiving daily text messages in addition to PT services would demonstrate improved quality of sleep, sleep hygiene, stress, pain, and function compared to the control condition including patients only receiving PT services.
Methods
Participants
Individuals currently seeking outpatient PT services were recruited to participate in the study from an outpatient PT clinic in the Midwest part of the United States. Flyers were placed at the front desk within the PT clinic and information about the study was provided to patients at their initial evaluation by their physical therapist. Twenty-two individuals who volunteered to participate in the study were randomly assigned to either a control group or intervention group. The study took place from September 1, 2021, to May 1, 2022, with each participant taking part in the study for a four-week period.
Participants were eligible for the study if they were an adult 18 years of age or older and currently receiving outpatient PT services for a minimum of four weeks. Participants were excluded from the study if they did not have access to a computer or smartphone that could receive automated text messaging services. The survey provided to participants was created using the PsychData platform. After consenting to participate in the present study, each individual was instructed by the Principal Investigator’s research assistant on how to access the survey using an electronic tablet provided to them at the clinic during their initial and follow-up appointments. This study was conducted in accordance with the university Institutional Review Board.
Materials and Dependent Measures
The survey was composed of a demographic information section followed by five subjective questionnaires: Pittsburgh Sleep Quality Index (PSQI) [21], Sleep Hygiene Index (SHI) [22,23], Perceived Stress Scale (PSS) [24], Numeric Pain Rating Scale (NPRS) [25,26], and the Patient-Specific Functional Scale (PSFS) [27-29]. Participants were asked to provide the following demographic information: age, sex, employment status, marital status, the highest level of completed education, race, reasons for seeking PT, length of time the participant had the current issue they were seeking PT for, average pain in the last week, conditions being treated for, and a list of current medications. The five questionnaires were used to evaluate the individual’s recent sleep behavior, sleep quality, stress level, and function with a self-chosen activity. Each questionnaire used in this study has proven to be a reliable form of acquiring data in past studies and a great means for comparison between initial and follow up visits [12,21,22,24,27].
The Pittsburgh Sleep Quality Index (PSQI) is a self-rated questionnaire containing twenty-four items that give seven component scores for subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction over a one-month time period. The sum of the nineteen self-reported scores is divided into the seven components and then added together to yield a single global score ranging from zero to twenty-one, with a higher score indicating poorer sleep quality. A global PSQI score greater than five yielded a diagnostic sensitivity of 89.6% and specificity of 86.5% in distinguishing individuals with “poor” sleep quality from individuals with “good” sleep quality [21].
The Sleep Hygiene Index (SHI) is a thirteen-item self-report survey, designed to assess sleep hygiene behaviors. Each question has a scale of zero (never) to four (always). Thus, each item was rated on a five-point scale. Participants could receive total scores ranging from thirteen to sixty-five. A higher score indicated poorer sleep hygiene. Reliability across populations for the SHI has been found on multiple occasions, with results showing a strong correlation to sleep quality and perception of daytime sleepiness [22,23].
The Perceived Stress Scale (PSS) is a brief stress assessment questionnaire that is highly regarded in its ability to outline how perception of a situation can influence how one scores themselves and whether they are placed in a low, moderate, or a high stress category. Participants were asked questions regarding their feelings and thoughts during the past month. Each question was scored on a five-point scale from zero (never) to four (very often). Participants received a total score rated on a scale of zero to forty. A score of zero to thirteen indicated low perceived stress, fourteen to twenty-six represents moderate perceived stress, and twenty-seven to forty suggests high perceived stress [24].
The Patient-Specific Functional Scale (PSFS) is a questionnaire used to assess functional disability and changes in performance activities of daily living. This questionnaire asked patients to list at least three activities they were unable to do or had difficulty doing as a result of the problem/injury they were being seen for. Patients then rated each of these activities on an eleven-point scale from zero to ten. A score of zero meant the patient was unable to perform the activity while a score of ten meant they were able to perform the activity at the same level as before injury or problem. In the follow-up assessment, patients rated the same activities they had listed previously in their initial visit. The PSFS provided a means to track patients’ functional ability with specific activities from beginning to the end of the sleep study, showing if any significant change had been made over the course of the study. The PSFS has shown to be a useful and reliable tool for clinical studies due to its consistency and responsiveness [27-29].
The Numeric Pain Rating Scale (NPRS) is a self-report pain assessment used on patients in primary care settings as well as in clinical studies. The NPRS has been confirmed to be a valid measurement of pain intensity in populations with known and chronic pain. It also has been shown to produce moderately accurate results. Participants within the current study used the NPRS to rate their pain on a scale from zero (no pain) to ten (intense pain). This pain scale was used in both the initial and follow-up assessments to examine if any improvements had been made in association with sleep hygiene tips [25,26].
Data Analysis
The researchers ran a series of mixed analysis of variance (ANOVA) models with our condition (intervention vs. control) as the between-subjects independent variable and time as our within- subjects variable. The pre- and post-scores for our five scales (PSQI, SHI, PSFS, PSS, and NPRS) served as our dependent variables. Significance was set at 0.05. IBM SPSS version 26 software was used for all data analyses.
Results
Participants
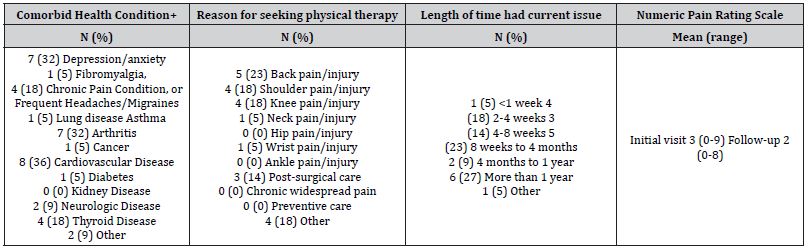
The researchers recruited 22 individuals (68% females) to participate in the present study. The average age of participants was 60 years (SD = 14.31, participant age ranged from 32 to 78 years). Participants were recruited from a Midwestern PT clinic. The 22 participants (11 in each group) were then randomly assigned to either the control or experimental group. Initial data collection was performed, and demographic data was collected (Tables 1&2).
Table 1: Demographics. N = Number. F = female, M = Male. + able to select more than 1; *full description is “unemployed but formerly employed, expect to be employed in the future, or currently looking for a job; %full description is “not looking for a job but working as a homemaker or doing work on a volunteer basis.
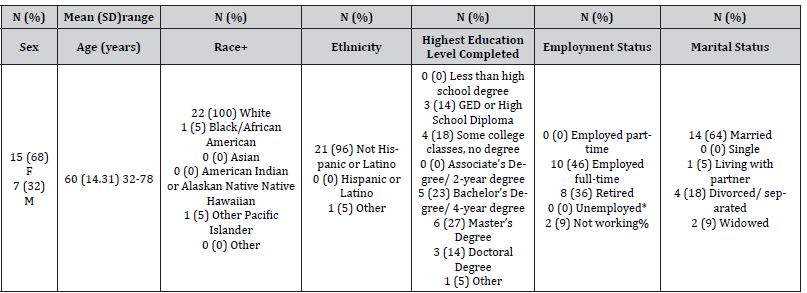
Table 2: Comorbid health conditions and reason for seeking PT services. +able to select more than 1.
Survey
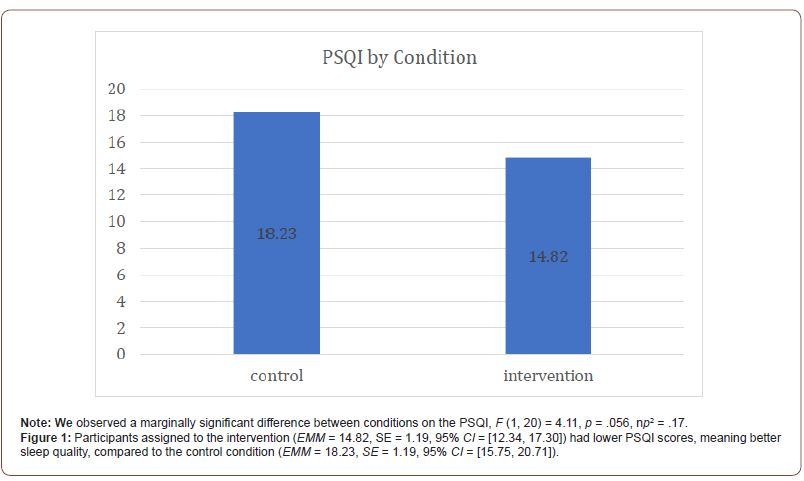
The data suggest there was no significant effect of time on the PSQI scale, F (1, 20) = 3.61, p = .072, np2 = .15. However, there was a marginally significant difference between conditions on the PSQI, F (1, 20) = 4.11, p = .056, np 2 = .17. Participants assigned to the text message intervention (M = 14.82, SE = 1.19, 95% CI = [12.34, 17.30]) had lower PSQI scores, meaning better sleep quality, compared to the control group who only received traditional PT services (M = 18.23, SE = 1.19, 95% CI = [15.75, 20.71]). No interaction between condition and time was observed for the PSQI, F (1, 20) = 1.24, p = .280, np2 = .06 (Figure 1).
We did not find a significant effect of time on the NPRS scale, F (1, 20) = 2.49, p = .130, np2 = .11. Further, there was no significant difference between the conditions on the NPRS scale, F (1, 20) = .58, p = .456, np2 = .03. No interaction between condition and time was observed for the NPRS scale, F (1, 20) = .46, p = .506, np2 = .02
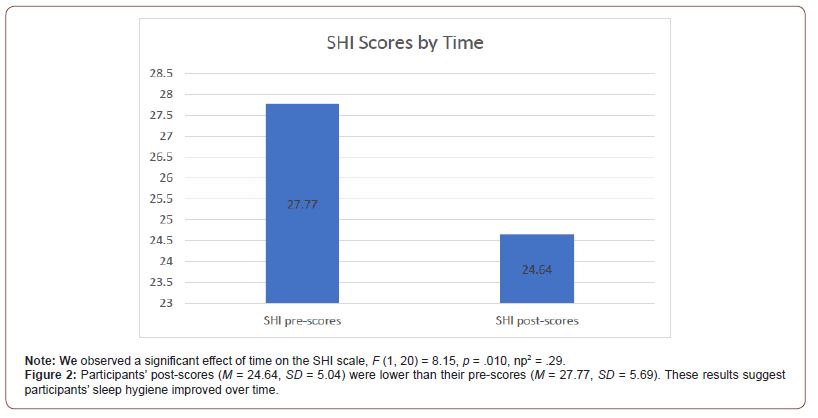
Data showed a significant effect of time on the SHI scale, F (1, 20) = 8.15, p = .010, np2 = .29. Participants’ post-scores (M = 24.64, SD = 5.04) were lower than their pre-scores (M = 27.77, SD = 5.69). These results suggest participants’ sleep hygiene improved over time (Figure 2). No significant difference between conditions was observed for the SHI scale, F (1, 20) = .27, p = .608, np2 = .01. No interaction between condition and time was observed for the SHI, F (1, 20) = .39, p = .539, np2 = .02.
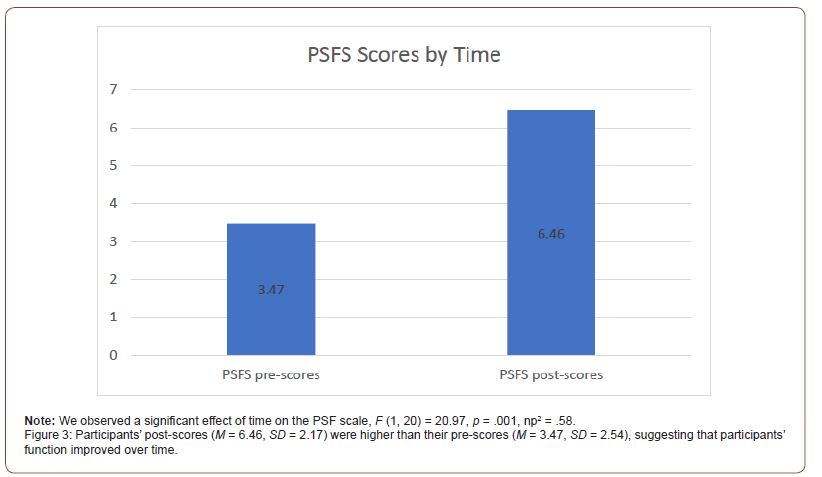
There was significant effect of time on the PSFS scale, F (1, 20) = 20.97, p < .001,np2 = .58. Participants’ post-scores (M = 6.46, SD = 2.17) were higher than their pre-scores (M = 3.47, SD = 2.54), suggesting that participants’ function improved over time (Figure 3). We did not observe a significant difference between conditions on the PSFS, F (1, 20) = .06, p = .805,np2 = .004, nor was there a significant interaction between condition and time on this measure, F (1, 20) = .03, p = .877,np2 = .002.
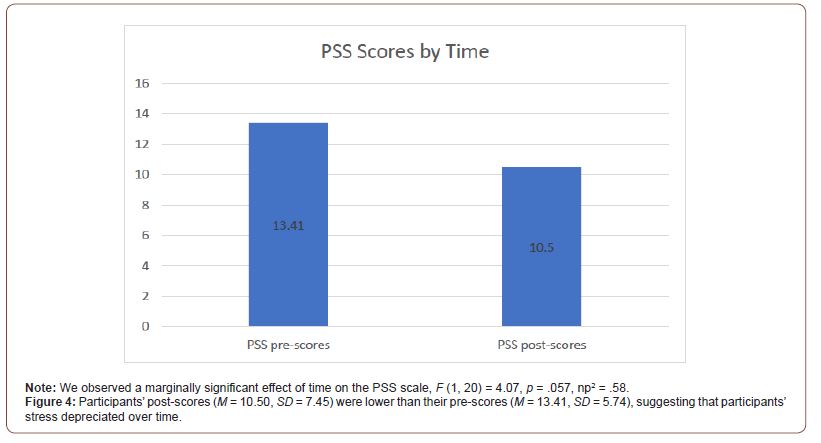
We observed a marginally significant effect of time on the PSS scale, F (1, 20) = 4.07, p = .057, np2 = .58. Participants’ post-scores (M = 10.50, SD = 7.45) were lower than their pre-scores (M = 13.41, SD = 5.74), suggesting that participants’ stress depreciated over time (Figure 4). There was not a significant difference between conditions on the PSS, F (1, 20) = 3.15, p = .091, np2 = .14. No interaction between condition and time was observed for the PSS, F (1, 20) = 1.92, p = .181, np2 = .09.
Discussion
The primary focus of the study was to examine the effectiveness of automated text messaging on sleep health in outpatient PT patients over the course of a four-week period. The researchers’ hypothesis was that patients receiving daily text messages would demonstrate improved quality of sleep, sleep hygiene, stress, pain, and function compared to patients receiving traditional PT services. The results of the study indicate that participants receiving automated text messages in addition to receiving traditional PT services showed improvements in sleep quality as indicated by the PSQI at near significant levels. Both the intervention and control groups showed improvements in sleep hygiene and overall function from pre- to post-scores. Collectively, the results demonstrate that PT interventions combined with automated text messaging may have an improvement in patient’s sleep quality, however PT alone may be enough to improve sleep hygiene and overall function. This improvement sleep hygiene and overall function echoes the results of previous research in this area by Atlas and Demirdal, demonstrating that PT interventions can make a significant difference on pain, sleep, mental status, and quality of life [5].
Although the results of the intervention group did not reach a statistical level of significance on the PSQI for overall sleep quality, it was trending that way. Our findings add to previous research which has indicated that PT exercises and modalities can have a positive impact on sleep. Moreover, PTs are positioned to make a positive impact on their patient’s sleep habits and quality of sleep [4,5].
Clinical Relevance
Based on the data from the current study, practicing clinicians may start to have a better understanding of what types of interventions best help their patients achieve good sleep quality and hygiene. The current study suggests that PT can be beneficial for improving patient’s function which is often the number one reason why patients present to PT clinics. This study also demonstrated that PT in general may be positively impacting patient’s sleep hygiene practices although further studies are needed to explore the best interventions to elicit substantial change in this area.
Limitations
There were a few limitations for this study. The sample size was small and potentially led to underpowered statistical analyses. Also, only those with the means to attend PT services at a private outpatient clinic were eligible to participate which might exclude people of lower socioeconomic status. In addition, no long-term follow- ups were performed so lasting sleep behavior changes are still unknown. Lastly, in previous research, text message interventions were successful in healthy young adults, however our population was much older with the average age being sixty years old, therefore we may not have seen as advantageous results as previous studies [18,20].
Future Research
Future research should continue to explore various sleep behavior change strategies to improve the quality of sleep of PT patients. This research could focus on additional randomized control trials aimed at finding the most effective and consistent interventions by including more long-term follow-ups as part of the study. Additionally, research could explore objectively tracking sleep changes through the use of sleep wearable trackers.
Conclusion
Physical therapy demonstrated positive changes in sleep hygiene, patient function, and overall sleep quality. The additional use of daily text messages caused a trend towards further improvements in sleep quality compared to traditional PT alone. Research demonstrates that sleep is an important aspect of overall health, and that sleep is often disturbed in PT patients; this study provides some initial insight into which interventions may be best for practicing clinicians to use for improving this disturbance in sleep. Further research is needed with larger sample sizes and more longterm follow-ups; however, this study is a great first step into understanding PT best practices for improving our patient’s sleep.
Acknowledgment
Research reported in this publication was supported by the South Dakota Biomedical Research Infrastructure Network (SD BRIN) through an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number P20GM103443. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would also like to thank Black Hills Physical Therapy for their willingness to assist us with recruitment of participants. This study would not have been possible without their support.
Conflict of Interest
Author declares no conflict interest.
- Suni E, Truong K (2022) Sleep statistics - facts and data about sleep.
- (2022) Sleep and Sleep Disorders Data and Statistics.
- Pfeiffer AM, Triplett C, Siengsukon C (2022) Examining the Prevalence of Sleep Disturbances in Patients Seeking Physical Therapy Services. Physiother Theory Pract 19: 1-9.
- Tramontano M, Angelis SD, Galeoto G, Cucinotta MC, Lisi D, et al. (2021) Physical Therapy Exercises for Sleep Disorders in a Rehabilitation Setting for Neurological Patients: A Systematic Review and Meta-Analysis. Brain Sci 11(9): 1176.
- Altaş EU, Demirdal U (2020) The effect of physical therapy and rehabilitation modalities on sleep quality in patients with primary knee osteoarthritis: A single-blind, prospective, randomized-controlled study. Turk J Phys Med Rehabil 66(1): 73-83.
- Murawski B, Wade L, Plotnikoff RC, Lubans DR, Duncan MJ (2018) A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med Rev 40: 160-169.
- Brown FC, Buboltz WC Jr, Soper B (2006) Development and evaluation of the Sleep Treatment and Education Program for Students (STEPS). J Am Coll Health 54(4): 231-237.
- Cai ZY, Wen-Chyuan Chen K, Wen HJ (2014) Effects of a group-based step aerobics training on sleep quality and melatonin levels in sleep-impaired postmenopausal women. J Strength Cond Res 28(9): 2597-2603.
- Gao R, Yi LV, Li X, Zhou K, Jin X, et al. (2014) Effects of comprehensive sleep management on sleep quality in university students in mainland China. Sleep and Biological Rhythms 12(3): 194-202.
- Greeson JM, Juberg MK, Maytan M, James K, Rogers H (2014) A randomized controlled trial of Koru: a mindfulness program for college students and other emerging adults. J Am Coll Health 62(4): 222-233.
- Hahn VC, Binnewies C, Sonnentag S, Mojza EJ (2011) Learning how to recover from job stress: effects of a recovery training program on recovery, recovery-related self-efficacy, and well-being. J Occup Health Psychol 16(2): 202-216.
- Jensen CG, Lansner J, Petersen A, Vangkilde SA, Ringkøbing SP, et al. (2015) Open and Calm--a randomized controlled trial evaluating a public stress reduction program in Denmark. BMC Public Health 15: 1245.
- Klatt MD, Buckworth J, Malarkey WB (2009) Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Educ Behav 36(3): 601-614.
- Kakinuma M, Takahashi M, Kato N, Aratake Y, Watanabe M, et al. (2010) Effect of brief sleep hygiene education for workers of an information technology company. Ind Health 48(6): 758-765.
- Murphy LR (1984) Stress management in highway maintenance workers. J Occup Med 26(6): 436-442.
- Querstret D, Cropley M, Fife-Schaw C (2017) Internet-based instructor-led mindfulness for work-related rumination, fatigue, and sleep: Assessing facets of mindfulness as mechanisms of change. A randomized waitlist control trial. J Occup Health Psychol 22(2): 153-169.
- Suzuki E, Tsuchiya M, Hirokawa K, Taniguchi T, Mitsuhashi T, et al. (2008) Evaluation of an internet-based self-help program for better quality of sleep among Japanese workers: a randomized controlled trial. J Occup Health 50(5): 387-399.
- Gipson CS, Chilton J, Dickerson SS, Alfred D, Haas BK (2019) Effects of a sleep hygiene text message intervention on sleep in college students. J Am Coll Health 67(1): 32-41.
- Nelligan RK, Hinman RS, Kasza J, Crofts SJC, Bennell KL (2021) Effects of a Self-directed Web-Based Strengthening Exercise and Physical Activity Program Supported by Automated Text Messages for People with Knee Osteoarthritis: A Randomized Clinical Trial. JAMA Intern Med 181(6): 776-785.
- Filion AJ, Darlington G, Chaput JP, Ybarra M, Haines J (2015) Examining the influence of a text message-based sleep and physical activity intervention among young adult smokers in the United States. BMC Public Health 15: 671.
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2): 193-213.
- Mastin DF, Bryson J, Corwyn R (2006) Assessment of sleep hygiene using the Sleep Hygiene Index. J Behav Med 29(3): 223-227.
- Cho S, Kim GS, Lee JH (2013) Psychometric evaluation of the sleep hygiene index: a sample of patients with chronic pain. Health Qual Life Outcomes 11: 213.
- Nielsen MG, Ørnbøl E, Vestergaard M, Bech P, Larsen FB, et al. (2016) The construct validity of the Perceived Stress Scale. J Psychosom Res 84: 22-30.
- Krebs EE, Carey TS, Weinberger M (2007) Accuracy of the pain numeric rating scale as a screening test in primary care. J Gen Intern Med 22(10): 1453-1458.
- van Dijk JF, Kappen TH, van Wijck AJM, Kalkman CJ, Schuurmans MJ (2012) The diagnostic value of the numeric pain rating scale in older postoperative patients. J Clin Nurs 21(21-22): 3018-3024.
- Abbott JH, Schmitt J (2014) Minimum Important Differences for the Patient-Specific Functional Scale, 4 Region-Specific Outcome Measures, and the Numeric Pain Rating Scale. J Orthop Sports Phys Ther 44(8): 560-564.
- Sterling M, Brentnall D (2007) Patient Specific Functional Scale. Aust J Physiother 53(1): 65.
- Mathis RA, Taylor JD, Odom BH, Lairamore C (2019) Reliability and Validity of the Patient-Specific Functional Scale in Community-Dwelling Older Adults. J Geriatr Phys Ther 42(3): E67-E72.
-
Ashley Pfeiffer*, Craig Triplett, Alissa Anderson Call, Daesha Erskin and Hannah Hirschi. Efficacy of Automated Text Messaging Services on Sleep Health, Stress, Pain, and Function in Physical Therapy Patients. On J Complement & Alt Med. 8(1): 2022. OJCAM.MS.ID.000678.
-
Sleep Health; Stress; Pain; Physical Therapy Patients; Sleep hygiene education; Text Messaging Services; Sleep Hygiene; Physical Therapy; Automated Text Messaging; Chronic health conditions; Adequate amount of sleep; Worsening sleep quality; Sleep interventions; Quality of life; Hypothesized; Physical therapist
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






