 Case Report
Case Report
Improved Quality of Life Following Myofascial Release Treatment Case Report of Police Officer
Andrew Gillihan1* and Shawn Drake2
1Doctor of Physical Therapy Student, Department of Physical Therapy, Arkansas State University, USA
2Professor Department of Physical Therapy, Arkansas State University, USA
Andrew Gillihan, Arkansas State University, PO Box 910, State University, USA.
Received Date:April 28, 2022; Published Date:June 03, 2022
Abstract
Due to the unpredictable, varied, and often physical nature of law enforcement duties, police officers are at increased risk of work-related bodily injury and psychologically traumatic events. Myofascial release (MFR) technique and myofascial unwinding (MFU) potentially addresses the ill effects, both physical and mental, of the occupation. Fascia is a connective tissue that permeates the human body. Myofascia is described as the connective tissue network that extends three-dimensionally throughout the body, surrounding, supporting, suspending, protecting, connecting, and dividing its muscular, skeletal, and visceral components. Therefore, the purpose of the present case report is to explore the effect of MFR and MFU on the quality of life, pain, and recovery outcomes of a law enforcement officer with a previous traumatic injury.
We reported a case of a 32-year-old male diagnosed with bilateral shoulder and low back pain. The subject was treated with MFR and MFU for 10 x 60-minute treatment sessions. The Pittsburgh Sleep Quality Index (PSIQ) evaluated sleep, the DASH (Disabilities of the Arm, Shoulder, and Hand) outcome measured physical function and symptoms of the shoulders, and the Short Form Survey (SF-36) indicated the quality of life. The subject filled out preintervention and postintervention outcome measures. The application of MFR and MFU resulted in improved scores on all outcome measures. The present case provides supporting evidence of the effectiveness of MFR and MFU as important treatment strategies in improving the quality of life of law enforcement officers.
Keywords:Myofascial release; Myofascial unwinding
Abbreviations:MFR: Myofascial release; MFU: Myofascial unwinding; NP: Non-specific; LBP: Low back pain
Introduction
Fascia is a connective tissue surrounding, supporting, suspending, protecting, and connecting all aspects of the body. At a microscopic and macroscopic level, the fascia serves as a tension component providing the body mobility, stability, and function [1]. Fascia acts as a communication system for emotions, pain, trauma, or unconscious thought [2]. Manual fascial techniques which include myofascial release (MFR) and myofascial unwinding (MFU), release fascial restrictions and restore optimal tissue mobility [3]. Tozzi et al. [4], reported improved pain perception in persons with non-specific (NP) and low back pain (LBP) following MFR.
Law enforcement is one of the most dangerous occupations and has a greater risk of musculoskeletal injury than many other occupations [5]. The most common body site of damage is the upper extremity, including soft-tissue sprains and strains at a rate of 2.5 times more likely than a lower body or torso injury. Most commonly, injuries occur due to a non-compliant offender or an assault [6]. Injuries cost law enforcement organizations financially and in staffing, calling for a more efficient post-injury rehabilitation and return to work protocol.
Massman [7], demonstrated that various psychophysiological effects are relevant to each patient and patient-specific trauma recovery. Therefore, the purpose of the present case report is to explore the impact of MFR and MFU on the quality of life, pain, and recovery outcomes for a law enforcement officer with a previous traumatic injury.
Case Presentation
Subject
The subject provided written informed consent to participate in this case report. He was a 32-year-old Caucasian male who worked as a police officer within a street crimes unit and a local gym owner. He was a United States Army Veteran and a previous professional road cyclist. He is married with children and enjoyed CrossFit-style exercise and Brazilian Jiu-Jitsu. The subject is a very high functioning and extremely busy individual in all aspects of his life.
The subject presented during the initial visit with complaints of bilateral shoulder pain. The subject described the initial right (R) shoulder injury in 2014 during a combative exercise while enlisted in the military. The damage came from a high-velocity anterior traction force at 90-degrees of flexion from another service member pulling on his distal arm. Upon further examination, the subjectreported symptoms of right (R) low back pain and episodic pelvic pain in conjunction with his shoulder pain. His left (L) shoulder has no specific mechanism of injury (MOI) but still has significant pain with flexion-type movements. The subject complained of the R arm “popping” and increased pain while driving with shoulder flexed and using a rotation-like motion while turning the steering wheel with one hand. The subject reported very little sleep due to pain and his lifestyle. His main goal for physical therapy is to reduce his pain levels and increase his shoulder range of motion to maintain a high fitness level during barbell lifts.
The systems review revealed impairments in the musculoskeletal and cardiopulmonary systems (Table 1). Neuromuscular, integumentary, and cognitive systems review were unremarkable. The specific musculoskeletal and cardiopulmonary impairments are in Table 2.
Table 1: Systems Review.
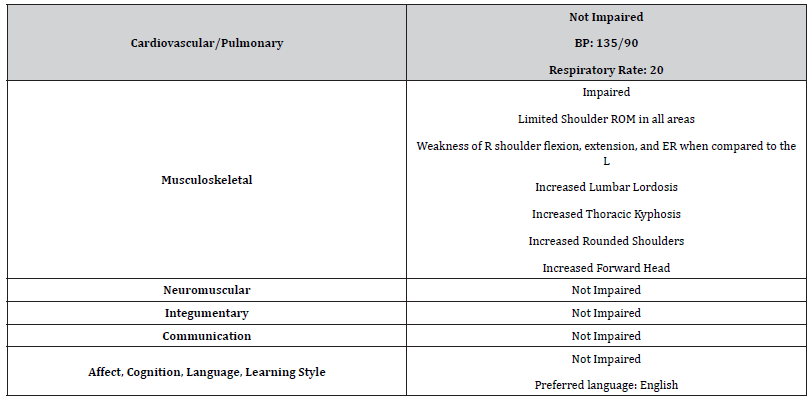
Table Abbreviations: (L)- left, (R)- right
Table 2: Tests and Measures.
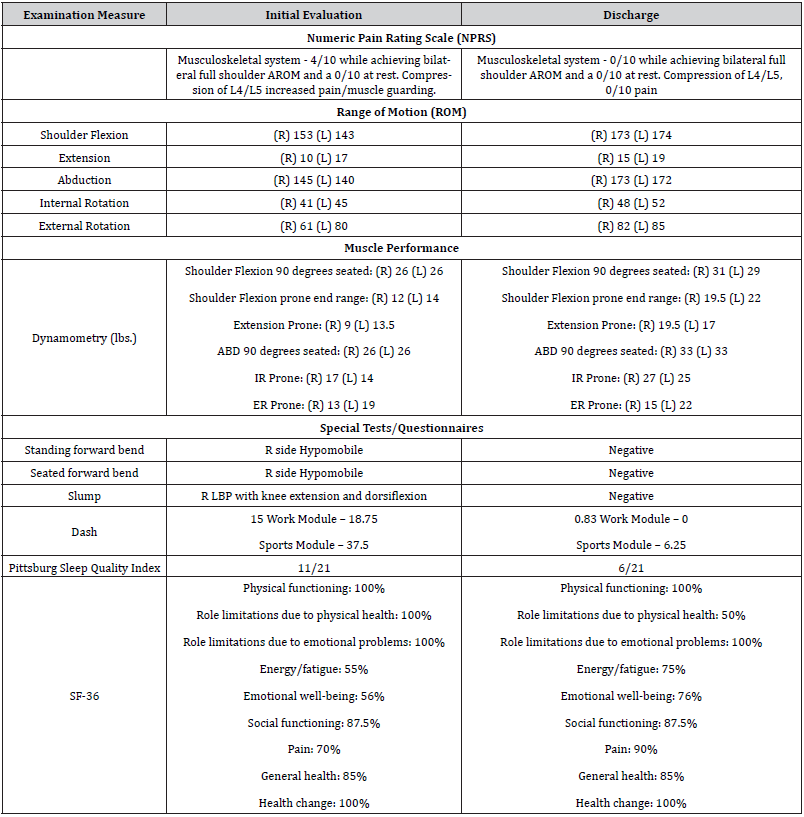
Table Abbreviations: (L)- left, (R)- right
Clinical Impression 1
The subject reported simultaneous multifactorial pain with high activity levels. Functional work activities, impaired functional mobility, myofascial restrictions, and pain were the subject’s primary difficulties. The differential diagnosis’ included ligament tear, labral tear, dislocated glenohumeral joint, subluxated glenohumeral joint. Special tests for the lumbar spine ruled out other differential diagnoses related to spine involvement. The patient presented with musculoskeletal imbalances and significantly decreased shoulder range of motion (ROM). The author’s examination results at the initial evaluation (IE) can be viewed in Table 1. Multiple physical therapy diagnoses established were bilateral shoulder pain and weakness and low back pain (LBP).
Dependent Measures
The examination utilized goniometric measurements to assess bilateral shoulder active range of motion (AROM). Goniometric measures contain excellent interrater reliability and good concurrent validity [8]. The Numeric Pain Rating Scale (NPRS) scored pain from 0-10 (0=no pain, 10=worst pain). The NPRS is both a reliable and valid scale to measure pain intensity in adults [9]. The minimal clinically important difference (MCID) of NPRS is a reduction in 2 or more points [10]. Handheld dynamometry measured strength throughout different planes and ranges of motion and has good reliability and moderate validity in measuring maximum isometric shoulder rotational strength [11]. Special tests, including the standing and seated flexion, are used in subjects with LBP to discern a sacroiliac joint dysfunction [12]. The slump test assessed altered neural tissue sensitivity and radicular symptoms using the slump test. The slump test assesses the mobility of the nerves of the lower extremities (LE) and has a sensitivity of 0.84, but a higher specificity of 0.83 [13]. The Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire examines musculoskeletal disorders of the upper limbs. The DASH holds validity and reliability for proximal and distal disorders. The MCID of the DASH is 10.83-15 [14]. The Pittsburgh sleep quality index (PSQI) screened for sleep dysfunction. The PSQI has shown strong reliability and validity in clinical and non-clinical samples. A global score of greater than five indicates a marker for significant sleep disturbances [15]. The SF-36 indicated a self-reported measure of overall health. Consisting of 8 domains, the SF-36 is used to measure an individual’s quality of life. The outcome measure has validity and reliability across a multitude of individuals [16].
Interventions
Coordination, communication, documentation, subjectrelated instruction:Communication with the subject included direct contact with the subject through in-person, text messages, and phone calls. The researcher educated the subject about the evaluation findings, plan of care (POC), and a home exercise program (HEP). The HEP included the following exercises:
Abdominal bracing: 3 x 10 repetitions, hold 5 seconds
Bridging: 3 x 10 repetitions, hold 3 seconds
Quadruped alternate arms / legs: 3 x 10 repetitions, hold 3
seconds
Plank: 3 x 30 second hold, twice daily
The researcher initially demonstrated exercises and gave the subject written/picture instructions on exercises. The subject performed the exercises during the first visit and at home once per day. The subject reported good compliance and understanding of the HEP. The researcher measured proper form and compliance at each visit by including the exercises within the treatment.
Procedural Interventions
The course of therapy consisted of a total of ten, 60-minute sessions. The in-person interventions consisted primarily of MFR, explicitly focusing on MFU techniques of the upper and lower body, cross arm pushes, cranial and fascial releases. The subject completed all treatment sessions and HEP.
Outcomes
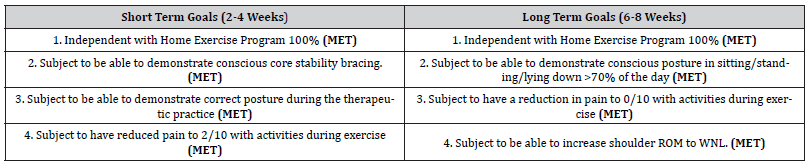
The subject reported continuous progress and reduced symptoms through the process of care. The objective measures showed improvement in shoulder ROM, strength, and pain levels (Table 2). All outcome measures, including the SF-36, DASH, and PSQI, met the criteria for MCID, indicating that the treatment sessions had an overall positive impact on the subject’s quality of life. The subject also met all of the short and long-term goals shown at the initial visit (Table 3). At discharge, the subject stated that he would continue with his HEP to maintain his relief of symptoms. There were no adverse or unanticipated events during his care episode.
Table 3:Short & Long-Term Goals.
Discussion
This case report described the physical therapy management of bilateral shoulder pain and low back pain. The management of the subject consisted of myofascial release techniques, myofascial unwinding, joint mobilizations, manual therapy, and therapeutic exercises. The initial findings of mobility and strength deficits throughout the body determined the subject’s POC. The POC demonstrated success as the subject had increased strength and ROM, decreased pain, and significant improvements in sleep quality and quality of life outcome measures. Considerations that may have positively influenced the POC included good overall health, prior high level of function, HEP compliance, and contextual factors such as time. Limitations of this study include selection bias and lack of a control group. The findings of this report are not generalizable to a larger population of subjects.
The findings of this case report supported previous research by Goyal et al. [3] & Tozzi et al. [4], including MFR to treat subjects with pain and myofascial restrictions. Additionally, therapeutic exercise is effective in the treatment of subjects with shoulder and low back pain [17]. The clinical implications of this case indicated MFR and the therapeutic exercise in the presence of shoulder and low back restrictions and pain appear to be effective for this subject. Future research should investigate the generalizability of MFR treatment to all law enforcement officers and another high rate of work injury population.
Acknowledgement
Shawn Drake, PT, PhD served as supervising physical therapist and research advisor during the project. She assisted in the final edits and submission of the article and No grant was provided for this research study.
Conflict of Interest
The authors declare no competing interests.
- Minasny B (2009) Understanding the process of fascial unwinding. Int J Ther Massage Bodywork 2(3): 10-17.
- Langevin HM (2006) Connective tissue: a body-wide signaling network? Med Hypotheses 66(6): 1074-1077.
- Goyal M, Goyal K, Bathla M, Kanimozhi D, Narkeesh D (2017) Efficacy of myofascial unwinding and myofascial release technique in a patient with somatic symptoms – a case report. Indian J Psychol Med 39(2): 199-201.
- Tozzi P, Bongiorno D, Vitturini C (2011) Fascial release effects on patients with non-specific cervical or lumbar pain. J Bodyw Mov Ther 15(4): 405-416.
- Lyons K, Radburn C, Orr R, Pope R (2017) A profile of injuries sustained by law enforcement officers: a critical review. Int J Environ Res Public Health 14(2): 142.
- Larsen B, Aisbett B, Silk A (2016) The injury profile of an Australian specialist policing unit. Int J Environ Res Public Health 13(4): 370.
- Massmann RS (2015) A descriptive study of the myofascial unwinding experience. Saybrook University.
- Kolber MJ, Hanney WJ (2012) The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: a technical report. Int J Sports Phys Ther 7(3): 306-313.
- Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken) 63(Suppl 11): S240-S252.
- Michener LA, Snyder AR, Leggin BG (2011) Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. J Sport Rehabil 20(1): 115-128.
- Chen B, Liu L, Bin Chen L, Cao X, Han P, et al. (2021) Concurrent validity and reliability of a handheld dynamometer in measuring isometric shoulder rotational strength. J Sport Rehabil 30(6): 965-968.
- Vincent-Smith B, Gibbons P (1999) Inter-examiner and intra-examiner reliability of the standing flexion test. Man Ther 4(2): 87-93.
- Majlesi J, Togay H, Unalan H, Toprak S (2008) The sensitivity and specificity of the slump and straight leg raising tests in patients with lumbar disc herniations. J Clin Rheumatol 14(2): 87-91.
- Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, et al. (2001) Measuring the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther 14(2): 128-146.
- Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, et al. (2016) The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev 25: 52-73.
- Jenkinson C, Wright L, Coulter A (1994) Criterion validity and reliability of the SF-36 in a population sample. Qual Life Res 3(1): 7-12.
- Shipton EA (2018) Physical therapy approaches in the treatment of low back pain. Pain Ther 7(2): 127-137.
-
Andrew Gillihan and Shawn Drake. Improved Quality of Life Following Myofascial Release Treatment Case Report of Police Officer. On J Complement & Alt Med. 7(4): 2022. OJCAM.MS.ID.000667.
-
Myofascial release; Myofascial unwinding; Myofascial Release Treatment; Physical; Mental; Occupation; Myofascia; Surrounding; Supporting; Suspending; Protecting; Connecting; Dividing; Muscular; Skeletal; Visceral components
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






