 Research Article
Research Article
Trends Among a Population of Neonatal Abstinence Syndrome Patients in Huntington, West Virginia
Taylor Boggess*
Joan C. Edwards School of Medicine at Marshall University, USA.
Taylor Boggess, PhD Student, Joan C. Edwards School of Medicine at Marshall University, 1600 Hal Greer Boulevard, Huntington, WV, USA.
Received Date: February 01, 2022; Published Date: June 13, 2022
Abstract
Neonatal abstinence syndrome (NAS) represents a serious emotional toll for the families of affected children and represents a significant financial burden for healthcare providers. Historically, patients living in rural regions, such as Appalachia, have limited access to healthcare facilities. The goal of this study was to increase understanding of the population served by a medical treatment center for NAS patients in Huntington, West Virginia in the hopes of better meeting the needs of these patients and their families. A clinical records review was conducted using the charts from 122 NAS patients that returned for follow-up clinic appointments at Lily’s Place, a non-profit NAS center in Huntington, between the years of 2015 and 2019. Factors examined in this study included number of visits to the clinic, drugs used by patient mothers, developmental milestones reached, medical issues observed during clinic visits, medical issues common among patient mothers, insurance status, and plans for care developed during each visit. The mean number of visits to the clinic per patient was 1.92. Opioids were found to be the most commonly misused class of drugs among the mothers of patients. Over one third of patient mothers were positive for hepatitis C. Medicaid was the most common insurance for patients and their parents/guardians. Many patients demonstrated a delay in reaching developmental milestones for their age group. Common patient symptoms included muscle and/or joint tightness, torticollis, and tremors. Many patient visits required a demonstration of stretches/exercises for the patient’s guardian to perform on the patient and most patient visits resulted in referrals to additional developmental support services. The results of this study indicate important trends among NAS patients and their families in West Virginia and, potentially, in the wider United States.
Keywords: Neonatal abstinence syndrome; Drug abuse; Infant development; Social determinants of health; Qualitative research
Abbreviations: NAS: neonatal abstinence syndrome; GERD: gastroesophageal reflux disease; CDC: Center for Disease Control and Prevention; BTT: Birth to Three; WVDHHR: West Virginia Department of Health and Human Resources; MRI: Magnetic Resonance Imaging
Introduction
Coinciding with the rise in rates of opioid abuse within the United States in the past several years, there has been a significant rise in incidence rates of neonatal abstinence syndrome (NAS) [1- 4]. In West Virginia alone, the incidence rate of NAS was 50.6 per 1000 live births in 2017 [5]. NAS represents a serious emotional toll for the families of affected children and represents a significant financial burden for healthcare providers [6]. Historically, patients living in rural regions such as Appalachia have limited access to healthcare facilities and are therefore less likely to receive treatment for substance abuse or NAS [7,8].
Lily’s Place, a non-profit neonatal abstinence syndrome center in Huntington, WV, founded in 2014, provides therapeutic and pharmacological care to newborns evaluated as demonstrating the signs and symptoms of NAS [9] born at nearby hospitals. Patient records from facilities such as Lily’s Place may offer insight into the patient populations that benefit most from the services provided by these facilities. In this study, the charts of patients treated at Lily’s Place that returned for follow-up appointments with Dr. Mitzi Payne, a pediatric neurologist at Cabell Huntington Hospital, between 2015 and 2019 were reviewed in order to examine any emerging trends among the children and their mothers. The types of drugs abused by the mothers of patients, the number of patients to reach developmental milestones, the types of medical issues observed among patients and their mothers, the insurance status of the patients, and the plan for care at each patient appointment were all recorded and compiled in order to report any emerging trends and increase understanding of the patient population served by Lily’s Place.
Discussion
Newborn patients from Huntington-area hospitals evaluated as showing symptoms of NAS were referred and transported to Lily’s Place. During their stay at the facility each patient is treated in individual nursery rooms where their health is monitored. Pharmaceutical treatment is administered, if necessary, to help wean patients from drugs of abuse. A monthly follow-up clinic was held for the parents of patients to bring their children for neurological and general health evaluations. The first follow-up appointments for all patients are scheduled 3 months following departure from the treatment center. Electronic charts (Allscripts Healthcare, LLC, Chicago, IL) from Lily’s Place patients who appeared for these follow-up visits between the years 2015 to 2019 were compiled and analyzed using statistical software (Microsoft Excel, Redmond, WA and GraphPad Prism, San Diego, CA). Confidentiality of patient names and identifying information was maintained in line with HIPAA regulations.
Results
Number of Appointments and Patients
122 patients that appeared for follow-up appointments with Dr. Payne at Lily’s Place between 2015 and 2019 were included in this study. These patients accounted for a total of 217 individual clinic visits. The majority of patients appeared at the clinic only once (67 patients or 54.9%), despite the encouragement for parents to schedule additional appointments (see Figure 1). The mean number of visits per patient was 1.92 with the highest number of visits for any one patient being 9.

Patient Sex Distribution and Birth Information
Of the 122 patients that appeared for follow-up appointments at Lily’s Place, 64 (52.5%) were male and 58 (47.5%) were female. 75 patients were in the custody of someone other than their biological mother at the time of their follow-up appointment (e.g. foster parent). 15 patients were born via cesarian section while 7 were born prematurely (before 37 weeks of pregnancy).
Drugs Used by Patient Mothers
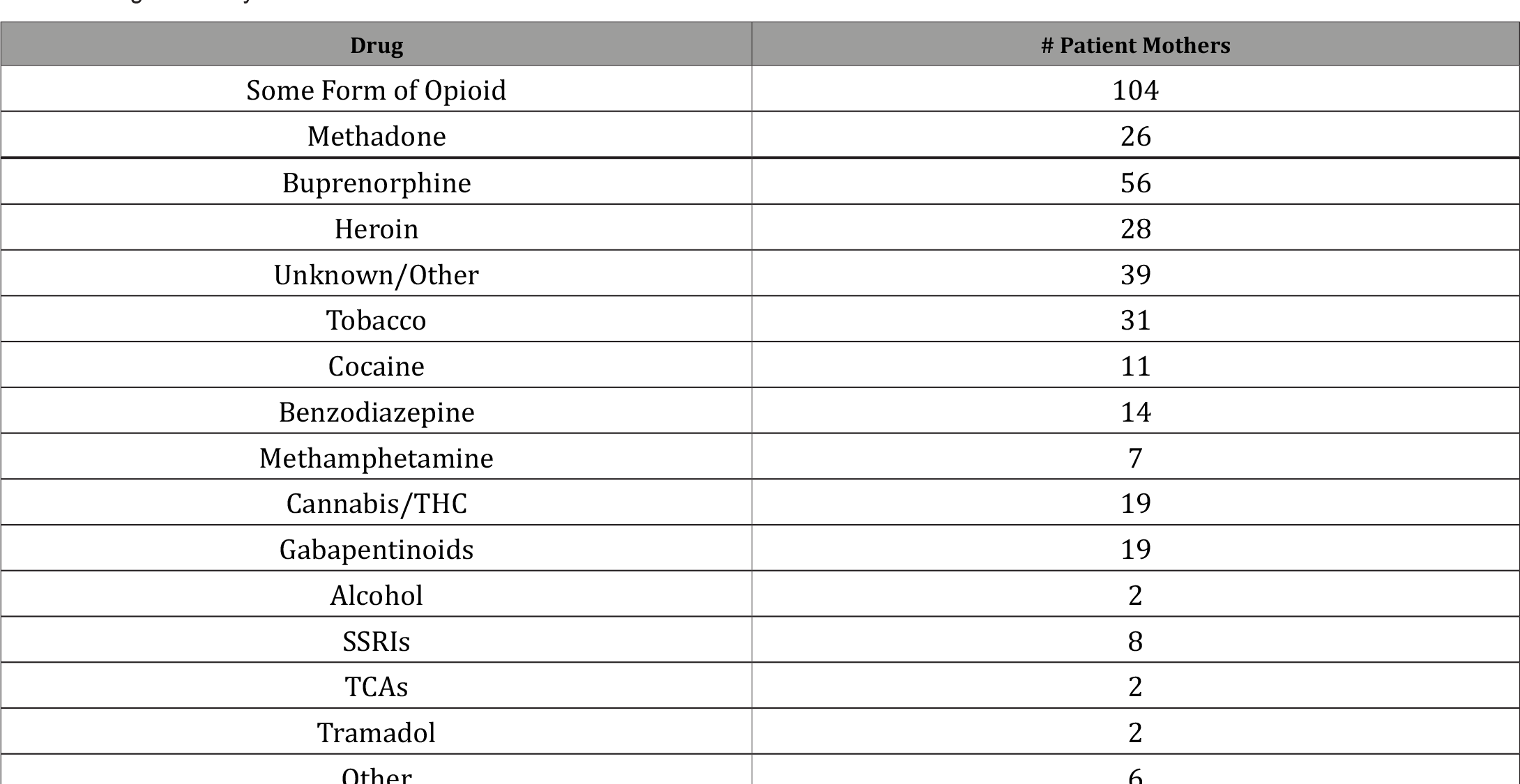
Drugs of abuse taken by the mothers of patients during their pregnancies were reported in the patient records through a combination of drug screenings at the time of birth or through selfreport by the mothers (see Table 1). Opioid drugs of some form were confirmed to be used by 104 mothers of patients (85.2%) during their pregnancy. The single most commonly used drug among mothers of patients was buprenorphine with 56 either currently taking the drug as a part of medication assisted treatment for opioid abuse or with a history of using the drug without a prescription. 28 mothers were recorded as having used heroin. Tobacco products were the most commonly used non-opioid drugs (31 mothers; 25.4%) followed by cannabis products and gabapentinoids (e.g. Neurontin®, Lyrica®) with 19 mothers (15.6%) each.
Table 1:Drugs Taken by the Mothers of Patients.
Reaching Developmental Milestones
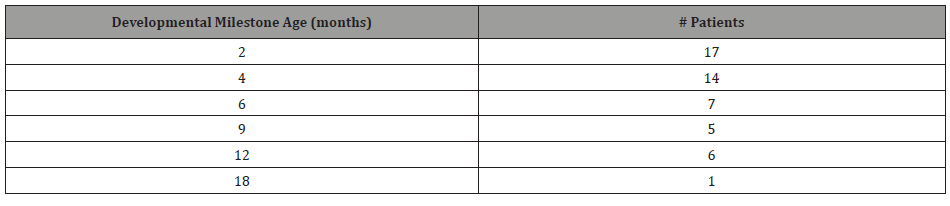
The development of each patient was assessed in each followup appointment based on the Centers for Disease Control and Prevention’s Developmental Milestones [10]. The number of patients to reach all milestones in their age group was recorded for this study. By 2 months of age, only 17 of the 122 patients included in this study successfully reached all developmental milestones for that age. At 4 months of age, 14 managed to reach all developmental milestones on time (see Table 2).
Table 2:Number of Patients That Reached Each CDC Developmental Milestone.
Medical Issues Observed Among the Patients
Medical issues common among Lily’s Place patients were recorded (see Table 3). During the follow-up appointments, the most common medical issues seen in patients were musculoskeletal, with 47 patients (38.5%) showing muscle and/or joint tightness, most commonly within the hips and legs. 20 patients were diagnosed with torticollis and 10 showed muscle weakness or low tone in at least one major muscle group.
Table 3:Medical Issues Among Patients at Follow-Up Appointments.
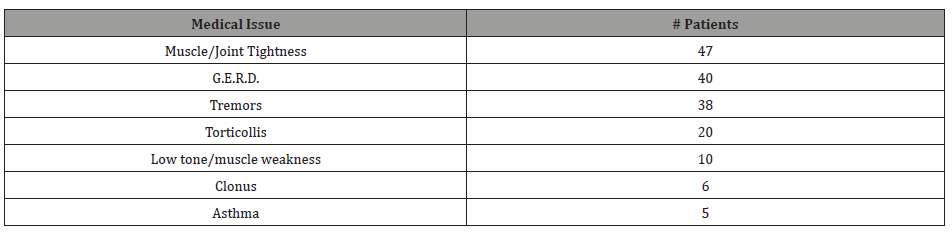
In terms of neurological symptoms, 38 patients (31.1%) exhibited tremors that could not be attributed to another neurological condition during their appointments. Among these patients, 25 patients exhibited tremors at their 3-month followup but not in subsequent clinic visits. The latest any patient demonstrated tremors during an examination was at 8 months of age. In addition, 6 patients exhibited clonus in at least one heel when tested during their neurological examinations.
The most common medical issue not involving the musculoskeletal or nervous systems was gastroesophageal reflux disease (GERD) with 40 patients diagnosed with the condition, the majority of which also had already been prescribed ranitidine (Zantac®) to reduce reflux by their primary care physicians. 5 patients were diagnosed with asthma and had all been prescribed medications for its treatment.
Medical Issues Among the Mothers of Patients
Significant health conditions of the mothers of patients were included in their children’s medical histories if such a condition could have impacted either their pregnancy or the delivery (see Table 4). The most common medical condition among mothers was Hepatitis C. 43 mothers either tested positive at the time of delivery or had a recent history of testing positive. Sexually transmitted diseases, hypertension, diabetes, and psychological conditions (including depression, anxiety, and bipolar disorder) were also observed in mothers.
Table 4:Medical Issues Common the Mothers of Patients.
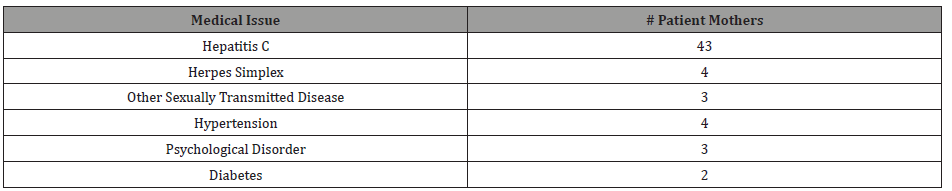
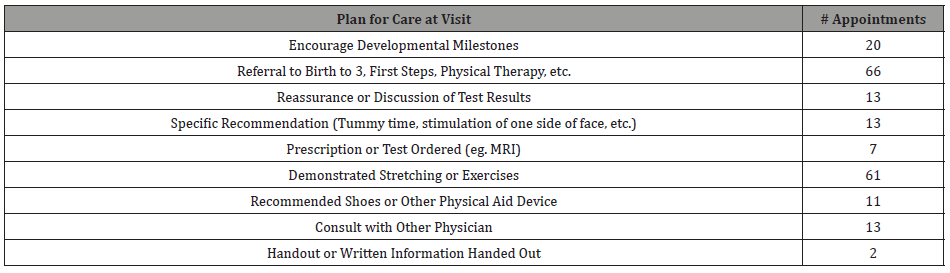
Table 5:Plans Developed for Patients at the End of Appointment.
Medical Insurance
The medical insurance status of each patient was recorded at each clinic visit. 65 patients’ (53.3%) primary medical insurance was listed as West Virginia Medicaid, making it the most common form of insurance among the patients included in this study. 10 patients had no medical insurance/self-pay at the time of their appointment. All other patients were insured by at least one other healthcare insurance company (e.g. Aetna®).
Plan for Care
At the end of every patient encounter, in addition to scheduling their next appointment at the clinic, a plan was developed to attempt to meet the medical needs of each patient. 66 of 217 visits to Lily’s Place resulted in a referral to developmental support services such as Birth to Three (BTT), a program developed by the West Virginia Department of Health and Human Resources (DHHR) through the Bureau for Public Health and the Office of Maternal, Child, and Family Health available for free to all children at risk for a developmental delay. Other services to which patients were referred included Head Start (a program overseen by the United States DHHR Office of the Administration for Children & Families), First Steps (overseen by the Kentucky Department for Public Health in the Cabinet for Health and Family Services), or one of Cabell Huntington Hospital’s Rehabilitation Services (including physical therapy, occupational therapy, and speech therapy). 61 clinic visits included a demonstration of stretches or exercises designed to improve muscle/joint tightness or low tone/muscle weakness. Specific recommendations other than stretching or exercise, such as increasing the amount of time the patient spent on its stomach to promote motor skills or deliberately stimulating one side of the patient’s face in order to encourage head turning in a specific direction to treat torticollis, were made in 13 visits. In 11 visits, specific physical aids, such as supportive shoes, were encouraged to improve mobility development in struggling patients. Tests such as MRI scans or prescription drugs were ordered in only 7 patient visits. Discussions of test results or general reassurance of patient parents/guardians occurred in 13 visits while in 20 visits parents/guardians of patients were given encouragement to continue current therapies with the goal of reaching developmental milestones. At the end of 13 separate visits, Dr. Payne made plans to consult with another physician (such as the patient’s primary care physician) to discuss a patient’s plan for treatment. Lastly, although written informational materials are always made available to patients and their families, during 2 separate interactions relevant informational handouts were shared and discussed with the patient’s parents/guardians.
Discussion
The results of this study of NAS patients treated at Lily’s Place reveal some important information about trends among NAS patients in West Virginia and, potentially, in the wider United States. The high appearance of opioid drug use among the mothers of patients is consistent with national trends of increased rates of opioid abuse [1-3]. The long-term health and psychological effects of prenatal exposure to drugs of abuse, such as opioids, continue to be an area of intense scientific investigation. Many such studies suggest a correlation between prenatal drug exposure and diagnosis of an intellectual disability or mental disorder [11-18]. Additional studies suggest a correlation between prenatal drug exposure and poor academic performance [16,19].
Among the opioid drugs used by patients, the single most common drug was buprenorphine. Buprenorphine is increasingly prescribed to pregnant mothers as part of medication assisted therapy to help them overcome opioid addiction and limit the exposure of the developing fetus to potentially more harmful opioids [20]. It has also been prescribed as a weaning therapeutic in place of methadone for infants with NAS prenatally exposed to opioids [21]. Therefore, it is not surprising that the most common drug taken by the mothers of the children in this study was some form of buprenorphine (as Subutex®, Suboxone®, Butrans®, etc.). However, this study agrees with previous research which shows that buprenorphine as a replacement therapy for other opioids does not eliminate the risk of NAS in exposed infants [21,22]. Of the 6 patients included in this study that exhibited clonus, 5 had been exposed to buprenorphine in utero (the 6th was exposed to methadone and other unspecified opioid drugs), a possible indication that a greater understanding of the effects of prenatal exposure to opioids, including buprenorphine, is still needed.
Drugs besides opioids were also observed in significant numbers among the mothers of NAS patients. Gabapentinoids such as gabapentin have increasingly been reported as being misused by substance abuse patients [23], both the drugs by themselves and in combination with opioids in order to potentiate the experienced high [24]. A unique set of NAS symptoms have also been reported among infants who were prenatally exposed to gabapentinoids such as tongue thrusting, back arching, and eye wandering [25]. Although the rise in rates of abuse of opioids is likely to blame for the rise in rates of NAS, these drugs of abuse are not the only ones commonly used by pregnant women and are often co-abused with other non-opioids.
Among the medical conditions observed among the patients, musculoskeletal issues were among the most common. The high rate of muscle and joint tightness seen among these patients can likely be attributed to the care they received during their initial stay at Lily’s Place. Tightly wrapping the body of an infant suffering from NAS in blankets has been shown to be an effective method of soothing these frequently fussy patients [26]. This swaddling keeps the limbs of the infant immobile and close to its body, potentially resulting in muscle and joint tightness that must be remedied by stretching later in the child’s development to avoid long term difficulties.
Examining the different plans for care developed in each appointment also gives insight into the different needs of the patients served by Lily’s Place. A large number of patient interactions involved only reassurance, guidance, or counseling on the part of the physician. Some of the most common issues seen among this patient group, namely muscle/joint stiffness, torticollis, and low tone/muscle weakness, could in fact be remedied through exercises, stretches, and specific recommendations (e.g. stimulating one side of the patient’s face to promote head turning) designed to promote musculoskeletal development [27,28].
This study also revealed important demographic information about patients most likely to receive services from facilities such as Lily’s Place. Over half of all patients included in this study were insured by Medicaid, indicating that the majority of patients seen at Lily’s Place could likely be described as lower socioeconomic status. While substance abuse and socioeconomic status are not necessarily correlated [29,30], families of a lower socioeconomic status traditionally have limited access to quality healthcare [31,32] and children of such families tend to do worse in academic settings [33]. In addition, the majority of patients in this study appeared at their follow-up appointments in the legal custody of someone other than their biological mothers. Stressful early life events and environments, such as those that might be found during a transition between biological and foster parent care, are correlated with poorer cognitive and physical development in children [34,35]. Such considerations may make a significant difference for NAS patients who would benefit from the involvement of social welfare programs as well as the engagement of invested healthcare professionals.
Conclusion
The results of this study may point towards important trends among NAS patients and their families in West Virginia and, potentially, in the wider United States. The data gained from this study should make apparent the importance of regular medical evaluation in the months immediately following treatment for NAS. It should also make apparent the need for facilities such as Lily’s Place that seek to meet the healthcare needs of socioeconomically disadvantaged populations. Increased understanding of the patient population served by a healthcare facility is likely to result in better patient outcomes and shape future policy to provide services better designed to meet the needs of those patients.
Acknowledgement
The authors would like to thank Dr. W. Christopher Risher for his insightful suggestions during the preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Holly Hedegaard, Arialdi M Miniño, Margaret Warner (2020) Drug Overdose Deaths in the United States, 1999–2018. NCHS Data Brief National Center for Health Statistics.
- Scholl L, Kariisa M, Wilson N, Baldwin G (2019) Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Report 67(5152): 1419-1427.
- (2012) National Survey on Drug Use and Health.
- Patrick SW, Davis MM, Lehmann CU, Cooper WO (2015) Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol 35 (8): 650-655.
- Umer A, Loudin S, Maxwell S, Lilly C, Stabler ME, et al. (2019) Capturing the statewide incidence of neonatal abstinence syndrome in real time: the West Virginia experience. Pediatr Res 85(5): 607-611.
- Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW (2018) Incidence and Costs of Neonatal Abstinence Syndrome Among Infants with Medicaid: 2004-2014. Pediatrics 141(4): e20173520.
- Hayes MJ, Brown MS (2012) Epidemic of Prescription Opiate Abuse and Neonatal Abstinence. JAMA 307(18): 1974-1975.
- Brown JD, Goodin AJ, Talbert JC (2018) Rural and Appalachian Disparities in Neonatal Abstinence Syndrome Incidence and Access to Opioid Abuse Treatment. J Rural Health 34(1): 6-13.
- Finnegan LP, Connaughton JF, Kron RE, Emich JP (1975) Neonatal abstinence syndrome: assessment and management. Addict Dis 2(1-2): 141-158.
- (2020) CDC’s Developmental Milestones. National Center on Birth Defects and Developmental Disabilities (NCBDDD). Centers for Disease Control and Prevention.
- Ornoy A (2003) The impact of intrauterine exposure versus postnatal environment in neurodevelopmental toxicity: long-term neurobehavioral studies in children at risk for developmental disorders. Toxicol Lett 140-141: 171-181.
- Ross EJ, Graham DL, Money KM, Stanwood GD (2015) Developmental consequences of fetal exposure to drugs: what we know and what we still must learn. Neuropsychopharmacology 40(1): 61-87.
- Nygaard E, Moe V, Slinning K, Walhovd KB (2015) Longitudinal cognitive development of children born to mothers with opioid and polysubstance use. Pediatr Res 78(3): 330-335.
- Nygaard E, Slinning K, Moe V, Due-Tønnessen P, Fjell A, et al. (2018) Neuroanatomical characteristics of youths with prenatal opioid and poly-drug exposure. Neurotoxicology and Teratology 68: 13-26.
- Johnson H, Diano A, Rosen T (1984) 24 Month neurobehavioral follow-up of children of methadone-maintained mothers. Infant Behavior and Development 7(1): 115-123.
- Fill MA, Miller AM, Wilkinson RH, Warren MD, Dunn JR, et al. (2018) Educational Disabilities Among Children Born with Neonatal Abstinence Syndrome. Pediatrics 142(3): e20180562.
- Sherman LJ, Ali MM, Mutter R, Larson J (2019) Mental Disorders Among Children Born With Neonatal Abstinence Syndrome. Psychiatr Serv 70(2): 151.
- Sirnes E, Oltedal L, Bartsch H, Eide GE, Elgen IB, et al. (2017) Brain morphology in school-aged children with prenatal opioid exposure: A structural MRI study. Early Hum Dev 106-107: 33-39.
- Oei JL, Melhuish E, Uebel H, Azzam N, Breen C, et al. (2017) Neonatal Abstinence Syndrome and High School Performance, Pediatrics 139(2): e20162651.
- Jansson LM, Velez M () Neonatal abstinence syndrome. Curr Opin Pediatr 24(2): 252-258.
- Kraft WK (2018) Buprenorphine in Neonatal Abstinence Syndrome. Clin Pharmacol Ther 103(1): 112-119.
- Kayemba-Kay’s S, Laclyde JP (2003) Buprenorphine withdrawal syndrome in newborns: a report of 13 cases. Addiction 98(11): 1599-1604.
- Vickers Smith R, Boland EM, Young AM, Lofwall MR, Quiroz A, et al. (2018) A qualitative analysis of gabapentin misuse and diversion among people who use drugs in Appalachian Kentucky. Psychol Addict Behav 32(1): 115-121.
- Bastiaens L, Galus J, Mazur C (2016) Abuse of Gabapentin is Associated with Opioid Addiction. Psychiatric Quarterly 87(4): 763-767.
- Loudin S, Murray S, Prunty L, Davies T, Evans J, et al. (2017) An Atypical Withdrawal Syndrome in Neonates Prenatally Exposed to Gabapentin and Opioids. J Pediatr 181: 286-288.
- Blount T, Painter A, Freeman E, Grossman M, Sutton AG (2019) Reduction in Length of Stay and Morphine Use for NAS with the “Eat, Sleep, Console” Method. Hosp Pediatr 9(8): 615-623.
- He L, Yan X, Li J, Guan B, Ma L, et al. (2017) Comparison of 2 Dosages of Stretching Treatment in Infants with Congenital Muscular Torticollis: A Randomized Trial. Am J Phys Med Rehabil 96(5): 333-340.
- Carenzio G, Carlisi E, Morani I, Tinelli C, Barak M, et al. (2015) Early rehabilitation treatment in newborns with congenital muscular torticollis. Eur J Phys Rehabil Med 51(5): 539-545.
- Hanson MD, Chen E (2007) Socioeconomic Status and Substance Use Behaviors in Adolescents: The Role of Family Resources versus Family Social Status. J Health Psychol 12(1): 32-35.
- Patrick ME, Wightman P, Schoeni RF, Schulenberg JE (2012) Socioeconomic status and substance use among young adults: a comparison across constructs and drugs. J Stud Alcohol Drugs 73(5): 772-782.
- Becker G, Newsom E (2003) Socioeconomic status and dissatisfaction with health care among chronically ill African Americans. Am J Public Health 93(5): 742-748.
- Braveman P, Gottlieb L (2014) The social determinants of health: it's time to consider the causes of the causes. Public Health Rep 129 Suppl 2 (Suppl 2): 19-31.
- Thomson S (2018) Achievement at school and socioeconomic background-an educational perspective, NPJ Sci Learn 3: 5.
- Coley RL, Lynch AD, Kull M (2015) Early Exposure to Environmental Chaos and Children's Physical and Mental Health. Early Child Res Q 32: 94-104.
- Berry D, Blair C, Willoughby M, Garrett-Peters P, Vernon-Feagans L, et al. (2016) Household Chaos and Children's Cognitive and Socio-Emotional Development in Early Childhood: Does Childcare Play a Buffering Role? Early Child Res Q 34: 115-127.
-
Taylor Boggess. Trends Among a Population of Neonatal Abstinence Syndrome Patients in Huntington, West Virginia. Open Access J Addict & Psychol 5(4): 2022. OAJAP.MS.ID.000619. DOI: 10.33552/OAJAP.2022.04.000619.
Neonatal abstinence syndrome, Drug abuse, Infant development, Social determinants of health, Qualitative research, Patients in Huntington, NAS patients, Joint tightness, Torticollis, Tremors
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






