 Research Article
Research Article
Obesity and Weight Loss in Male Veterans
Joseph M Latham1*, Stephen Berger2, Terri Verone3, Anna Morales3, Christine Ma3, Ian Gordon3 and Gilly Koritzky2
1Irvine Valley College, USA
2The Chicago School of Professional Psychology – Anaheim, USA
3Department of Veteran Affairs, Long Beach, USA
Joseph M Latham, Doctoral student, Irvine Valley College, USA.
Received Date: September 17, 2022; Published Date: October 19, 2022
Abstract
Obesity is associated with risks to physical and mental health, but behavioral weight-loss programs only see limited success, with few participants achieving their anticipated weight-loss goals. Being able to predict who is likely to benefit from such programs can reduce stress and frustration as well as inform the development of more effective interventions. The predictors offered by psychologists have included aspects of decision-making, such as impulsivity and reward sensitivity. However, the previous studies about weight-loss predictors have been almost exclusively carried out with female participants, and studies on males are scarce. The few studies that looked at gender differences in this context suggest that obesity is associated with different cognitive properties in women and men. Therefore, we cannot assume that what predicts weight-loss outcomes in men with obesity are the same predictors that have been reported for women. In a first-of-its-kind study, a sample of men with obesity have been followed in a weight-loss program, aiming to predict weight-loss by aspects of cognitive (decision-making) style. We hypothesized that compared to unsuccessful dieters, successful dieters (i.e., those who lose weight and achieve weight-loss goal) are less influenced by recent information when making decisions. Reward sensitivity appeared to be a distinct predictor in male participants. Additional variables such as age, self-reported impulsivity, and mental health were identified as predictors in males. The study’s results suggest targeted variables that can assist with weight loss interventions to improve obesity treatment outcomes.
Introduction
Nature of the Study
Obesity is a worldwide epidemic associated with increased morbidity and mortality that imposes an enormous burden on individual and public health [1]. The United States Department of Veterans Affairs (VA) reports that 78% of veterans are overweight or obese [2], which elevates the risk of many health problems, including type 2 diabetes, high blood pressure, stroke, certain types of cancer, sleep apnea, liver and kidney disease, and pregnancy complications [3]. Being able to predict who is likely to benefit from such programs can reduce stress and frustration and can contribute to the development of more effective interventions. The research seems to indicate a prevalent, cognitive difficulty in applying this principal to decision-making about food. This study will focus on the cognitive decision making of obese men in a behavioral weight loss program.
Background
Obesity is defined as abnormal or excessive fat accumulation that presents a risk to an individual’s health [3]. Those who are 20% or more above their ideal weight are considered obese [4]. Body mass index (BMI) is a crude weight-to-height ratio commonly used to define obesity and is calculated by weight (in kilograms) divided by the height squared (in meters) or as a person’s weight (lbs.) divided by height (in2) multiplied by 703. A person with a BMI of 30 or more is considered obese, and a person with a BMI of 25 or more is considered overweight [3]. Globally, a total of 1.9 billion and 609 million adults were estimated to be overweight and obese in 2015, respectively, representing approximately 39% of the world’s population [5]. The Centers for Disease Control and Prevention (CDC) reports that the prevalence of obesity in the US increased from 30.5% to 42.4% and the prevalence of severe obesity increased from 4.7% to 9.2% [6].
The National Heart, Lung, and Blood Institute recommends that the overweight or obese be informed not only by the evidence linking obesity to increased mortality, but also randomized controlled help control diseases exacerbated by obesity, but also decreases the likelihood of developing comorbidities [7].
Problem Statement
The Department of Veterans Affairs [8], reports that 78% of veterans are overweight or obese. Obesity is associated with increased risk for many illnesses, including type 2 diabetes, cardiovascular disease, and several cancers [9]. It is also associated with increased healthcare costs. For example, obesity costs the Veterans Health Administration an estimated $370 per patient per year in additional medical and non‐medical costs [2].
Behavioral weight-loss programs see only limited success, with few participants achieving their anticipated weight-loss goals [8]. Being able to predict who is likely to benefit from such programs can reduce stress and frustration and can contribute to the development of more effective interventions.
A few studies have focused on cognitive (decision-making) predictors of successful weight-loss outcomes [10,11]. However, these studies were limited to female populations. Because there are known differences between obese men and women in several aspects of cognition and decision making [12,13], findings from women cannot be directly generalized to men. Therefore, there is a need to study specifically what may predict weight loss outcomes in obese men. As men comprise the majority of military veterans, this knowledge will particularly benefit this population.
We hypothesize that compared to unsuccessful dieters, successful dieters will show a greater tendency to take time-distant (or long-term) information into account in the process of decisionmaking. That is, successful dieters will have lower scores in the recency parameter of the EV model. Other potential predictors— risk-taking, delay of gratification, impulsiveness, and readiness for change—were included in the study for comparison. The literature has suggested that they predict weight-loss outcomes in women, but no data exist on their predictive power in men.
Purpose of the Study
The main objective of this study was to examine how decisionmaking patterns predict weight-loss outcomes in men, and how these patterns are relevant to clinical psychology. This objective is consistent with the priorities outlined by the leadership of the Department of Veterans Affairs as a part of personalized, proactive veteran-driven care. Specifically, this study focused on two potential predictors: recency (reliance on short-term considerations rather than long-term considerations when making decisions) and reward-sensitivity (being motivated by enjoyment). Other potential predictors — risk-taking, delay of gratification, and impulsiveness — were included in the study for comparison. The literature has suggested that they predict weight-loss outcomes in women, but no data exist on their predictive power in men.
Research Questions and Hypotheses
The following hypotheses were tested:
• Similar to female dieters in past studies, successful male dieters will show greater tendency to take time-distant (or long term) information into account in the process of decision making. That is, they will have lower scores in the recency parameter of the Expectancy Valence model.
• Similar to female dieters in past studies, successful male dieters will show lower motivation to pursue rewards. That is, they will have lower scores in the gain/loss sensitivity parameter of the Expectancy Valence model.
• Other potential predictors – demographic variables, risk taking, delay of gratification, and intelligence – were examined in an exploratory manner.
Theoretical/Conceptual Framework
To predict success in weight-loss interventions, one should search for individual differences within the obese population. These are often more subtle, and harder to detect, than differences between obese and non-obese populations. In a prior study [10], researchers have used a mathematical model called the Expectancy-Valence (EV) model for this purpose. The EV model [14], is a mathematical model that analyzes behavior in complex decision-making tasks. The model is designed to capture individual differences in decision-making and is known to differentiate well between subpopulations with decision-making deficits that are otherwise indistinguishable from one another [15]. Moreover, past research has linked the EV Model’s recency component to activation in the anterior prefrontal cortex, a region associated with effortful information processing and inhibitory control [16,17].
The EV model—essentially a series of mathematical estimations—is applied to data that is collected while a subject performs a decision-making task that involves multiple, repeated decisions (typically the Iowa Gambling Task is used; see [19]). Based on these data, the model estimates that there are three underlying components of an individual’s decision-making style: (1) reward-sensitivity, or the extent to which the person is motivated by pursuing gains versus avoiding losses; (2) recency (learning rate), or the extent to which one’s decisions are affected by new information at the expense of taking all potential outcomes into account, and; (3) consistency of choice.
In their study on predictors of weight-loss success, Koritzky G, et al. [10], found that the EV model’s recency component predicted weight loss, with successful dieters having significantly lower scores (i.e., less recency, or more reliance on long-term thinking) than unsuccessful ones. Successful and unsuccessful dieters were otherwise similar in their demographics, intelligence, and other parameters of decision-making. This study, however, utilized a majority-female sample.
Methods
Participants
The participants were 36 men aged 18 years and older who participated in a weight loss program called MOVE!, which is offered through the VA Healthcare System, at the VA hospital in Long Beach, CA (i.e., they are discharged members of the military). The MOVE! program participants are either obese (BMI>30) or overweight (BMI>25) with obesity-related co-morbidities. Exclusion criteria of the MOVE! are: active cancer, acutely exacerbated chronic medical conditions (e.g., Cardiac Heart Failure, Chronic Obstructive Pulmonary Disease), cognitive impairment and/or dementia, endstage disease (any organ system), active psychosis, or current substance abuse.
An IRB from the Department of Veterans Affairs, Long Beach research department has approved this research study, and data has been collected at this location. The participants were recruited from the MOVE! program, an outpatient weight-loss intervention which is held in the VA’s Nutrition and Food Services department. The program is a 7-week long structured weight- loss intervention that includes weekly clinician-led group meetings. The program aims to help veterans who are overweight or obese to improve their eating habits and is behavioral (i.e., it does not include medication or other medical procedures). Participants’ weight is recorded every week at the meeting. Height is obtained from the system’s medical records.
Participants attended an individual meeting with a research assistant, in which they completed the above-mentioned questionnaires and tasks. These meetings took place at the VA Long Beach campus between February 2017 and May 2020. All participants provided an informed consent. Participants’ responses in the tasks and questionnaires were recorded and saved on a protected computer. Participants’ weight measured weekly as part of the program, and their attendance records, were saved in a similar way. Permission has been given to the present researcher to retrieve these data, in a de-identified form, and use them in this study. The present project was limited to the amount of data collected by the MOVE! program. Nonetheless, prior studies that employed similar methods [10,18], have used smaller sample sizes as well. MOVE! participants were informed about the study upon signing up for the program, and their participation was voluntarily. The study originally began with (N = 37) participants. However, one of the participants has been omitted from the sample. The omitted individual did not meet the inclusion criteria (BMI < 25), as he was in the program to support a fellow colleague.
Instrumentation
Demographics Questionnaire: Used to help identify limitations to the generalization of findings from the study. It includes questions about age, gender, ethnicity, education level, profession, employment, nicotine use, previous weight loss attempts, and exercise levels).
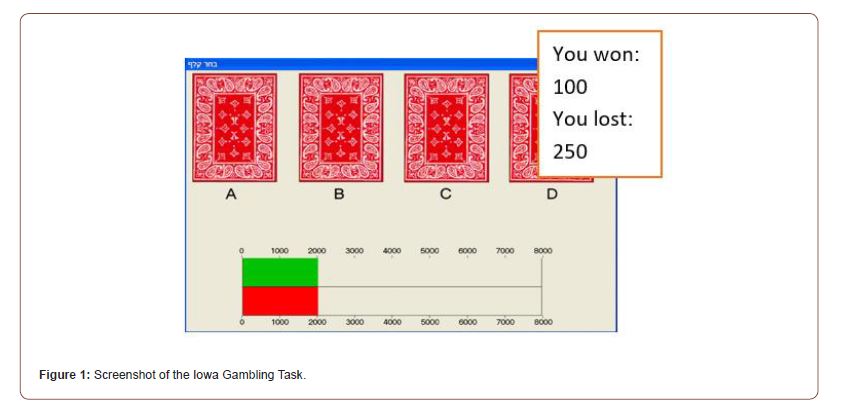
The Iowa Gambling Task (IGT): The Iowa Task is a complex decision-making task, which resembles a computer game [19]. Participants are shown four decks of cards and given a loan of $3,000 in play money. They then must select a card from one of the decks for a number of repeated trials unknown to them (in the present case, 100 trials). Each choice yields a different gain, but losses also occur. Two of the decks are considered “good decks” and the other two are considered “bad decks.” The good decks yield smaller gains and even smaller losses, which result in a net gain. The “bad decks” yield higher gains with occasional large losses, resulting in a net loss. Normal performance on the task is defined as participants learning over the course of the experiment to choose the “good decks.” The task has been used in the past in a study of weight-loss prediction in women [10]. See Figure 1 for a screenshot of the task.
The Expectancy-Valence model [14]: This model will be applied to the data obtained in the Iowa Gambling Task to estimate three numeric scores which correspond to the model’s three parameters:
1) A motivational component indicating the subjective weight the decision-maker assigns to gains versus losses. The sensitivity-to-reward parameter ranges from 0 to 1 and represents the relative weight assigned to gains (rewards) in the evaluation of alternatives.
2) A learning rate component that indicates the degree of prominence given to recent outcomes at the expense of relying on the full range of experience. The recency parameter ranges from 0 to 1 and represents (inversely) the tendency to take long-term considerations into account.
3) A probabilistic component indicating how consistent the decision-maker is between learning and responding. The consistency parameter ranges from 0 to 10 and represents the tendency to choose the alternatives with higher subjective expectations, as opposed to making random selections.
Barratt Impulsiveness Scale: This questionnaire is designed to assess impulsiveness as a trait [20]. This is one of the most widely used assessment tools for gauging impulsiveness. The Barratt questionnaire has an internal consistency coefficient total that ranges from 0.79 to 0.83 for populations of undergraduates, substance-abuse patients, psychiatry patients, and prison inmates [20]. The scale measures multiple factors of impulsivity such as attention, motor, self-control, cognitive complexity, perseverance, and cognitive instability. It also measures the secondary factor of non-planning as this is also attributed to impulsiveness.
Simplified Iowa Gambling Task: This is a variant of the Iowa Task specifically designed to measure risky decision making. Prior research observed differences in task performances between obese and normal-weight men [12]. The task score is used as a measure of risk taking.
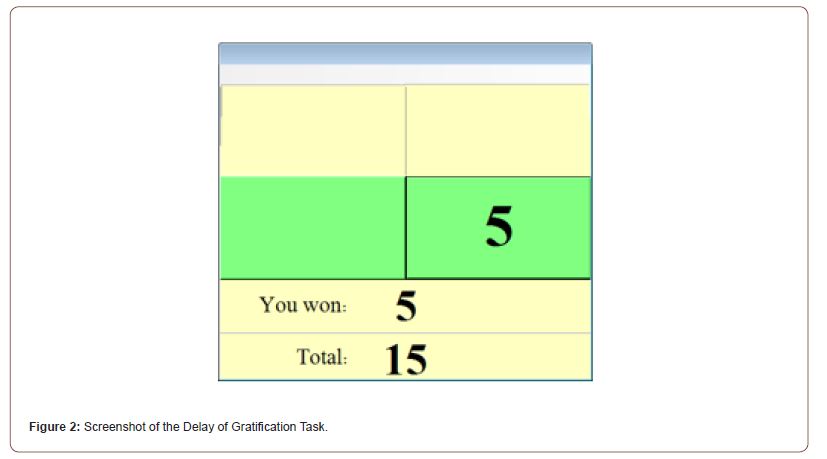
Delayed Gratification Task: Delay of gratification involves postponing immediate satisfaction to obtain an increased reward in the future [21]. In this task, participants repeatedly choose between two unmarked buttons displayed on a computer monitor. Buttons yield a small payoff of five points in either 40% (low frequency) or 80% (high frequency) of the trials. The low-frequency button is available for pressing as soon as each trial begins, while the highfrequency button becomes available after a 10-second delay. In each trial, the participant chooses whether to wait the full 10 seconds for better prospects of reward or to press the low-frequency button immediately and move to the next trial faster. Delay of gratification is measured by the number of times the subject selects the highfrequency (delayed) button. See Figure 2 for a screenshot.
The Raven Advanced Progressive Matrices Test: This is a standard, brief (10-item), non-verbal measure of intelligence, which will be used to control potential confounding effects of intelligence on the study’s results. The test involves observation skills and problem-solving abilities. On each question, the subject is asked to select the visual patterns most suitable to complete a 3x3 matrix of geometric patterns. It is designed to minimize language and cultural bias in intelligence assessment [22].
Statistical Analysis
Comparisons between the two groups (successful dieters and unsuccessful dieters) were done using independent-samples t tests and Chi-square tests as appropriate for each variable. Weightloss success was predicted using logistic regression models with recency and reward sensitivity as the predictor. Weight loss was coded “1” for dieters who lost at least 3% of their initial body weight, and “0” otherwise. Analyses were done using IBM SPSS Statistics 25 software.
Descriptive Statistics
Table 1:Program outcomes of the study sample compared to the population of the MOVE! program on the VALB campus.
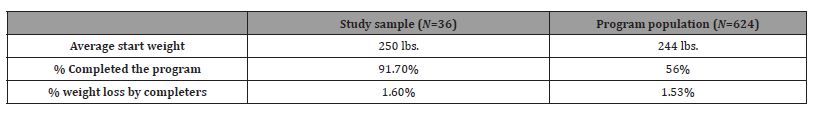
The analytical sample of thirty-six participants was mostly consistent in its characteristics with the population of MOVE! program participants at the Long Beach VA hospital, and also with a larger MOVE! participants population, described by Zenk SN, et al. [23]. The MOVE! 2019 group series on the VALB campus consisted of fourteen different cohorts throughout the year. There were 624 participants in total, and 351 of them completed the program. Two hundred and seventy-three participants dropped out of the program leading to a 43.75% dropout rate. Table 1 shows the program outcomes in the present study’s sample against those of this population.
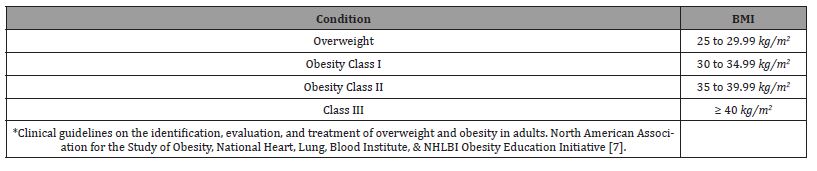
The sample’s (N=36) BMI range was 25.46–50.65 (mean = 36.36, SD = 6.15) and consisted of 13.9% Overweight (n = 5), 39.2% Obesity Class I (n = 14), 14% Obesity Class II (n = 5), and 34.6% Obesity Class III (n = 12) participants. See Table 2 for further information.
Table 2:Current BMI rates and Classifications.
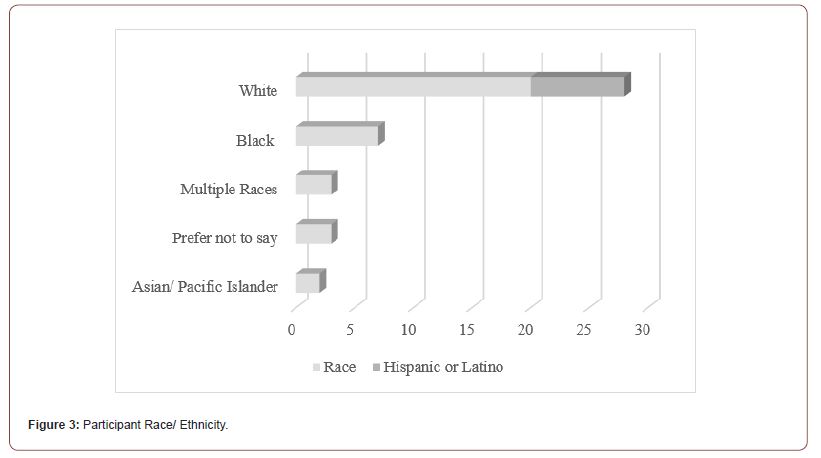
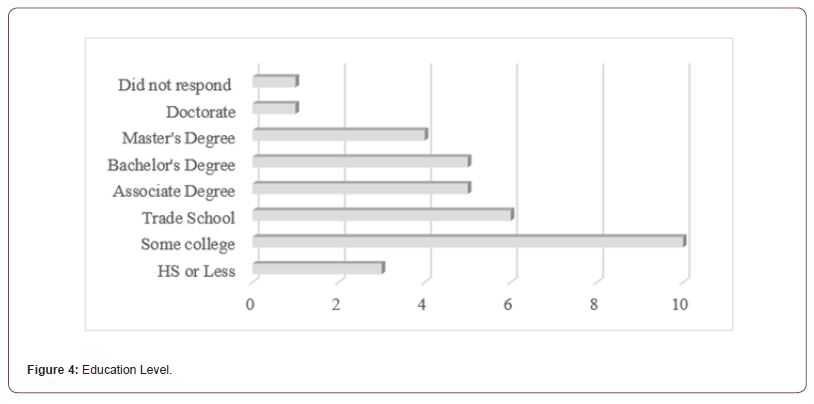
The age range of the participants in the present study was 25– 78 (mean = 58.97, SD = 14.09). There was no variance in gender, as the sample consisted of all male veterans (n = 36). The sample was 58.3% White, 22.2% Black or African American, 5.6% Asian, 5.6% multiple races, and 8.3% preferred not to say. Twenty-two percent (n = 8) of the sample were of Hispanic or Latin descent (subcategory of White). This information is consistent with previous accounts of the MOVE! program population [23].
Since we had access to the sample’s medical information, we also looked at additional variables that are commonly associated with persons with obesity and the veteran population. Out of the entire sample 86.1% (N=31), did not have a history of substance abuse in their medical records, whereas 13.9% (N=5) had a previous or current substance abuse diagnosis. We also looked at the sample’s mental health information. Within our sample, 61.1% (N=22) have received mental health diagnosis in their medical record. 38.9% (N=14) did not have a mental health diagnosis in their record. Lastly, since obesity is commonly related to chronic illnesses, we also examined that variable within our sample. We found that 94.4 % (N=34) did have at least one chronic illness and 5.6% (N=2) did not. Frequency and percentage information for the variables can be seen in Figures 3 & 4.
Of the entire sample, 91.7% (n = 33) completed the weight loss program (attended the required number of meetings and received a certificate of completion), whereas (n = 3) 8.3% did not. The study participants attended 6.29 (SD = 1.23) weekly meetings on average (out of 7). The last recorded weight was used to calculate the weight-loss percentage for each participant. Four of the participants (11.1%) lost 5% or more of their original weight, which satisfied the criterion for successful weight loss, while 32 participants (88.9%) were unsuccessful (they either lost less than 5% of their weight, or their weight increased). We also analyzed those who lost 3% or more of their original weight. 25% (N=9) lost more than 3% of their original body weight.
Program Completion and Weight-loss Outcomes
Weight loss, the primary outcome variable in this study, has been measured using two operational definitions: first, a binary variable indicating whether the participants achieved the weightloss goal of 5% of their original body mass; second, another binary variable indicating whether the participants achieved a weight loss goal of 3% of their original body mass; finally, a continuous variable indicating the change in original weight since pre-treatment (as a percentage of original body mass).
Of the entire sample, 91.7% (n = 33) completed the weight loss program (attended the required number of meetings and received a certificate of completion), whereas (n = 3) 8.3% did not. The study participants attended 6.29 out of 7 (SD = 1.23) weekly meetings on average. The last recorded weight was used to calculate weight-loss percentage for each participant.
Four of the participants (11.1%) lost 5% or more of their original weight, which satisfied the aforementioned criterion for successful weight loss, while 32 participants (88.9%) were unsuccessful (they either lost less than 5% of their weight, or their weight increased). Due to the small number of successful participants, we also applied a less-restrictive criterion of having lost at least 3% of one’s original weight. Twenty-five percent (N=9) met this criterion. Table 3 lists the differences between successful and unsuccessful participants (according to the 3% criterion).
Hypothesis Testing
As noted earlier, the purpose of the present study was to identify significant predictors of successful weight-loss in men. First, we examined whether certain decision-making variables (recency and gain/loss sensitivity), which predicted successful weight loss in past studies with female samples, would also predict weight loss in men in the present study. Second, we conducted an exploratory analysis of other potential predictors of weight loss in men, including demographic variables, risk taking, delay of gratification, and intelligence. The results of this analysis are discussed in the next section.
The first hypothesis of this study was that when compared to unsuccessful male dieters, successful male dieters will exhibit a greater tendency to take time-distant (or long-term) information into account in decision making. That is, that successful dieters will have lower scores in the recency parameter of the EV model than unsuccessful dieters. As can be seen in Table 3, this hypothesis was not confirmed.
The second hypothesis was that when compared to unsuccessful male dieters, successful male dieters will show lower motivation to pursue rewards. That is, successful dieters will have lower scores in the gain/loss sensitivity parameter of the EV model. As can be seen in Table 3, this hypothesis has not been confirmed either.
Predictors of Successful Weight Loss in the Present Sample
The exploratory analysis of the other study variables revealed significant differences between successful and unsuccessful dieters in relation to their age, intelligence score, and having a mental health diagnosis. As can be seen in Table 3, participants’ age was a significant predictor, such that older participants were more successful at losing weight than younger participants.
Table 3:Characteristics of successful and unsuccessful dieters.
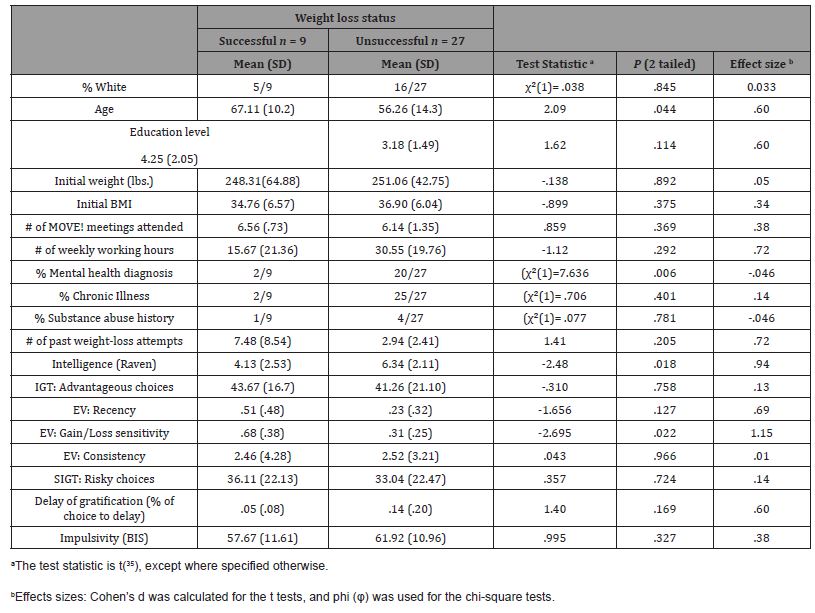
There was also a significant difference in intelligence scores between successful and unsuccessful dieters. The Raven Advanced Progressive Matrices Test yields scores between 0 and 10, and they do not follow a normal distribution. Therefore, we also tested the difference in intelligence scores between the successful and unsuccessful dieters using a non-parametric test, the Mann- Whitney U test. This test also yielded a significant result (U = 52.5, Z = -2.127, p = 0.035). These results suggest that successful dieters have lower intelligence scores than unsuccessful dieters.
A chi-squared test of independence was performed to examine the relationship between having a mental health diagnosis and the ability to successfully lose weight. As can be seen in Table 3, the prevalence of mental illness was significantly lower among successful dieters.
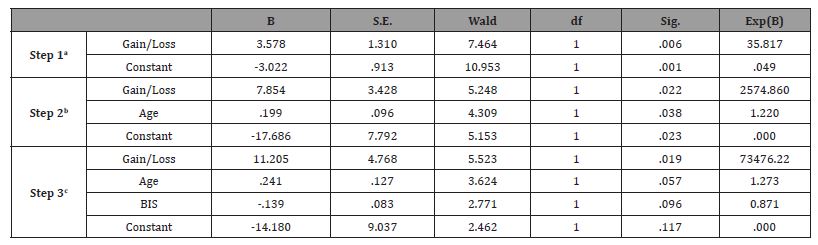
Finally, we conducted a hierarchical, binary logistic regression to identify the best predictors of weight loss in men. The binary outcome variable was having lost at least 3% of one’s start weight. The variables tested were those associated with decision-making: advantageous decision making (as measured by the IGT), risk taking (risky choices in the SIGT), delay of gratification, impulsivity (score on the self-report BIS), and the three EV model parameters of recency, gain/loss sensitivity, and consistency. To these, we added those factors that emerged as significant in the group comparisons shown in Table 3: age, intelligence, and having an existing mentalhealth diagnosis. The method of variable entry was Forward: Wald.
The best model was produced in the 3rd step of the hierarchical regression (χ2(3) = 23.11, p < 0.0001, Cox & Snell R2 = 0.493, Naglekerke R2 = 0.743). It correctly identified 91.2% of the cases. The model included the following predictors: gain/loss sensitivity, age, and impulsivity. The regression parameters are shown in Table 4. As can be seen, higher motivation to pursue reward sensitivity, older age, and lower self-reported impulsivity were associated with higher odds of successfully losing weight.
Table 4:Parameters of the hierarchical logistic regression.
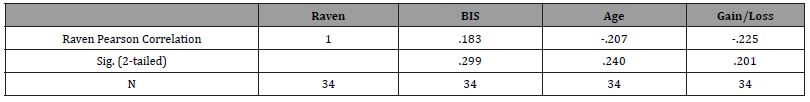
A Pearson’s Correlation examined the relationship between intelligence and the variables that came out significant in the regression model (age, BIS score, and Gain/ Loss sensitivity). As can been seen in Table 5, no significant relationship was found between intelligence, age, impulsiveness, and Gain/ Loss sensitivity.
Table 5:Correlation analysis of significant variables.
Summary, Conclusions, and Recommendations
Interpretation of Findings
Even though we did not confirm our hypothesis in the present study, we did identify a potentially new predictor for men. This study’s data has identified that higher motivation to pursue reward sensitivity, age, and self-reported impulsivity are predictors of weight-loss in men. None of which were similar to previous studies on women. These finding can be looked at as preliminary, but they may have the potential to identify a gender difference in weight loss outcomes. Opposite of the original hypothesis, our study has identified that higher sensitivity to reward can result in better weight loss outcomes in men.
The researchers are mindful that the current sample is very small. Therefore, any interpretation of these findings must be done in awareness of the limited sample size. Due to the COVID-19 pandemic of 2020, hospitals limited access to only essential personnel. The MOVE! program was paused for approximately one year and was later converted to telehealth groups. Therefore, the research assistant was no longer granted access to those participating in the program and the measures utilized required in-person administration. Prior to the shutdown, an analysis was conducted to identify the minimum number of subjects for an adequate study power. The researcher identified that 40 participants were needed, but the pandemic halted data collection. Having access to only 36 participants may have been a primary reason the hypothesis was not met.
Hypothesis One
The first hypothesis was unable to confirm that successful male dieters will exhibit a greater tendency to take time-distant information into account in decision making. In previous findings from Koritzky G, et al. [10], identified that women who engage in weight loss interventions and have long-term objectives will likely to be more successful than those who only view this concept in short-term objectives. This finding does not appear in alignment with the present study’s results, as higher levels of taking timedistant information was not associated with better weight-loss outcomes.
Other previous research has also highlighted the importance of time-distant information when it comes to dieting processes. For example, Brewer and colleagues [24], reported that traditional diet plans tend to fail due to individuals not addressing their relationship with a modern food environment. The authors reported that shortterm information, such as dietary restriction methods, may be counterproductive, simply because individuals do not have the ability to address long-term issues of how psychological stress can trigger maladaptive eating behaviors. Although short-term information can be useful to motivate individuals to change eating patterns and behaviors, it is the long-term issues that need to be addressed; mindfulness eating patterns, enjoying healthy eating, and practicing self-compassion. It has also been stated that it is important to have dieters focus on long-term intrinsic motivations versus short-term motivations is more beneficial over time [24]. However, that research was focused predominately on women. In this study, a difference in the gender was identified in motivation with weight loss. Therefore, weight loss approaches may not be generalized between genders.
Another study of predictors in weight loss [25], found that increased self-efficacy and cognitive restraint, decreased inhibition, and decreases in depressive symptoms were associated as common factors of those who can maintain weight loss. The authors completed an experimental study exploring the differences between groups after a behavioral weight loss intervention. The two groups were separated into weight gainers and maintainers and the predictors were assessed at 0, 6, 12, 18, and 24 months. The authors compared and contrasted the difference between the two groups and identified the predictors associated with weight maintenance over time. The researcher concluded cognitive restraint, decreased inhibition, and decreases in depressive symptoms were the cognitive predictors associated with those who can be successful in a long-term weight loss program. Consistent with most of the literature, this study also included predominately females [25].
Summary
In summary, although this study was unable to confirm the hypothesis that successful male dieters will exhibit a greater tendency to take time-information into account in decision making, the results are not in alignment with long-term information being utilized in decision making. In previous research [10], unsuccessful dieters were found to rely on recent information, whereas successful dieters take time distant information into consideration. It is imperative to understand that to be successful in losing weight and maintain healthy body weight compositions over time, individuals must consider other important long-term information. These long-term practices can change habits leading to a more healthier relationship with food [24].
Hypothesis Two
The second hypothesis was unable to confirm that successful male dieters will show lower reward sensitivity. In relation to previous literature, it has been found that individuals with worse inhibitory control scores at their baseline predicted less weight loss over time. That is, individuals who find it difficult to actively suppress a behavior will more likely find it difficult to lose weight [26]. The sample in this study was predominately White (71%) women (80%), identifying a gap in the research with a predominately male sample. Additionally, other researchers [27], explored the importance of motivation and reward when it comes to dieting. For example, the authors completed a study that investigated whether calorie information and dieting status modulated rewards when evaluating food images. The authors found that dieters were more likely to take caloric information into consideration when viewing images of food than their non-dieter counterparts. In essence, this finding suggests that dieters are more likely to consider caloric information when viewing food images, leading to healthier eating patterns. This in turn, highlights that calorie information has the ability to alter brain responses in food images by reducing reward system activation while increasing control system activation. This study was important to mention because it demonstrates that dieters can regain higher levels of control when viewing food items combined with caloric information. However, the sample in the Courtney AL, et al. [27], study was 79% female, identifying their results may not generalize strongly among a predominately male population.
Researchers who investigated food reward and food choice [28], found that the pleasure and desire of foods influence food choice and intake; that is, reward responses to food are associated with food choice and whether individuals decide to overeat. They recommended that it is imperative that individuals who are dieting are offered more healthy food choices so that they can choose foods that look pleasurable and desirable. This study [28], had both females and males within their sample, the sample utilized were college students ages 18-25, and likely varied is body types (i.e., normal, overweight, underweight).
Summary
In summary, previous research has discussed the importance of understanding inhibitory control and how it is essential that dieters are presented with caloric information with food choices so that they can be more successful at changing their eating patterns. Furthermore, research has suggested that when dieting, individuals should be presented with more healthy food choices, as there is a strong link between pleasure and desire when selecting food.
Recommendations
This study has clinical implications for the field of health psychology and weight-loss management. While the link of obesity to depression may be open to debate with an inconclusive link to causation, some research has found a link between obesity and depression. Studies have found that being overweight or obese can increase the likelihood of a person experiencing symptoms of depression [29,30], through either the food that they consume [31,32], or through eating as a tool to cope with negative emotions [33]. To further illustrate the complexity of the comorbidity of obesity and depression, those who have a depressive disorder have been found to lose less weight more than people who report having other serious mental illness and people without serious mental illness and depressive disorders [34]. Therefore, within the field of health psychology, it is important that professionals focus on ensuring that their clients are following healthier diets such as that of the Mediterranean diet [32]. Because studies have suggested that there is a strong link between gut microbial and the brain, by having individuals follow diets that are higher in vegetables, fish and seafood, nuts, and legumes, will assist in decreasing experiences of depression [31], while also providing them with an ability to focus on healthy eating behaviors and weight loss. Professionals in the field should also ensure that their male older clients focus on more long-term motivations as older individuals tend to focus more so on their overall perceptions of health versus that of losing weight [33].
Within the arena of weight loss management, although older adults tend to focus on their overall perception of health, it would behove health psychologists to have them focus on a combination of dieting behaviors, exercise, and behavior modification [35]. Additionally, focus on an overall lifestyle change rather than just a diet has been a consistent finding in this study with older males and in all-male weight loss clinics. It has been reported [36], that an overall lifestyle changes rather than just dieting alone is an essential consideration within their all-male clinics. A recommendation for gender-specific weight interventions has been made, stating that a socialized lifestyle approach enables increased success for male participants [36]. Doing this can supports more long-term goals that are not only focused on food consumption changes, but also long-term goals that support their overall health. This will allow males to experience an increased motivation for change when it comes to their overall health, not just that of their weight. Health psychologists could utilize such strategies to increase the efficiency and effectiveness of treatment planning and weight loss will come secondary within a lifestyle change.
Attendance, not weight loss, is the only requirement for a veteran to receive additional services. Additional cultural interventions that focus on rewards can be an essential aspect of weight loss in this population. If minimal goals are incorporated throughout the treatment program, and the population receives culturally appropriate rewards, it could potentially increase the program’s efficacy. For this population, a weight loss medal (e.g., 1%, 3%, or 5%) could assist with the reward seeking, increase overall weight loss, and help the program’s efficacy.
Limitations
There are some limitations that must be discussed in this current study. The first limitation that was experienced was the COVID-19 pandemic. Because the researcher started this study before COVID-19 was dominant throughout society, changes in social distancing guidelines, quarantining, and isolation forced the study to be transitioned toward a telehealth platform. Therefore, the experience of COVID-19 and the transitioning of the program to a telehealth platform could have affected the results. Therefore, future studies should be continued to focus on this program, yet via a telehealth model, since the current COVID-19 pandemic is ongoing. Transitioning the assessment battery continuing to be conducted via a telehealth, the researcher will be allowed access to higher number of sample sizes. In this current study, the sample size was smaller than anticipated, due to the researcher not being allowed access to the research site due to social distancing and isolation guidelines as recommended by the CDC.
Another limitation for this study was that of the method that was utilized to collect and manage the data. Because this study was quantitative in nature, a limitation could have occurred in the data, as participants were not allowed to answer questions in any manner that they saw fit; instead, they had to answer the questionnaire based upon certain pre-determined answers [37]. Future research could allow for a more qualitative approach, or include semistructured interviews within the dataset, so that participants could provide additional information of their perceptions and lived experiences, allowing for a more comprehensive understanding of the phenomenon being explored [38].
A final recommendation for future studies is that research should be directed over a longer period with more consistency. For example, because this current study was paused for a period of one year, there lacked a consistent follow-through with the participants. Therefore, future research should include a longitudinal approach, where data can be collected over time, increasing the understanding of the success of weight loss and how it can be affected over the years in older male adults.
Acknowledgement
None.
Conflict of interest
None of the authors have a conflict of interest.
References
- Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, et al. (2015) Genetic Studies of body mass index yields new insights for obesity biology. Nature 518(7538): 197-206.
- The Management of Overweight and Obesity Working Group (2014) VA/DoD Clinical Practice Guideline for Screening and Management of Overweight and Obesity. Department of Veterans Affairs.
- World Health Organization (2018) Obesity.
- American Heart Association (2014) Losing Weight.
- Chooi YC, Ding C, Magkos F (2019) The epidemiology of obesity. Metabolism 92: 6-10.
- Centers for Disease Control and Prevention (2021) Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS Data Brief 360: 1-8.
- The National Heart Lung and Blood Institute (1998) For Health Professionals
- The U.S. Department of Veterans Affairs (2016) Office of Research & Development.
- World Health Organization (2016) Obesity and overweight: Fact sheet.
- Koritzky G, Rice C, Dieterie C, Bechara A (2015) The biggest loser thinks long-term: Recency as a predictor of success in weight management. Front Psychol 6:1864.
- Teixeira PJ, Carraca EV, Marques MM, Rutter H, Oppert JM, et al. (2015) Successful behavior change in obesity interventions in adults: A systematic review of self-regulation mediators. BMC Med 13(1): 84-99.
- Koritzky G, Yechian E, Bukay I, Milman U (2012) Obesity and risk taking. A male phenomenon. Appetite 59: 289-297.
- Weller RE, Cook EW, Avsar KB, Cox JE (2008) Obese women show greater delay discounting than healthy-weight women. Appetite 51(3): 563-569.
- Busemeyer JR, Stout JC (2002) A contribution of cognitive decision models to clinical assessment: decomposing performance on the Bechara gambling task. Psychol Assess 14(3): 253-256.
- Yechiam E, Kanz JE, Bechara A, Stout JC, Busemeyer JR, et al. (2008) Neurocognitive deficits related to poor decision making in people behind bars. Psychon Bull Rev 15: 44-51.
- Hochman S, Shreckengost J, Kimura H, Quevedo J (2010) Presynaptic inhibition of primary afferents by depolarization: observations supporting nontraditional mechanisms. Ann N Y Acad Sci 1198: 140-152.
- Koritzky G, He Q, Xue G, Wong S, Xiao L, et al. (2013) Processing of time within the prefrontal cortex: recent time engages posterior areas whereas distant time engages anterior areas. Neuroimage 72: 280-286.
- Koritzky G, Dieterle C, Rice C, Jordan K, Bechara A (2014) Decision-making, sensitivity to reward, and attrition in weight-management. Obesity 22(8): 1904-1909.
- Bechara A, Damasio AR, Damasio H, Anderson SW (1994) Insensitivity to future consequences following damage to human prefrontal cortex. Cognition 50(1-3): 7-15.
- Barratt ES (1985) Impulsiveness defined within a systems model of personality. In CD Spielberger, JN Butcher (Eds.). Advances in Personality Assessment (pp. 113-132 ). Hillsdale, NJ: Erlbaum.
- Newman JP, Kosson DS, Patterson CM (1992) Delay of gratification in psychopathic and nonpsychopathic offenders. J Abnorm Psychol 101(4): 630-636.
- Raven J (1989) The Raven Progressive Matrices: A review of national norming studies and ethnic and socioeconomic variation within the United States. Journal of Educational Measurement 26(1): 1-16.
- Zenk SN, Tarlov E, Powell LM, Wing C, Matthews SA, et al. (2018) Weight and Veterans’ Environments Study (WAVES) I and II: Rationale, methods, and cohort characteristics. Am J Health Promot 32(3): 779-794.
- Brewer JA, Ruf A, Beccia A L, Essien GI, Finn, et al. (2018) Can mindfulness address maladaptive eating behaviors? Why traditional diet plans fail and how new mechanistic insights may lead to novel interventions. Front Psychol 9: 1418.
- Creasy SA, Ostendorf DM, Blankenship, JM, Grau L, Arbet J, et al. (2022). Effect of sleep on weight loss and adherence to diet and physical activity recommendations during an 18-month behavioral weight loss intervention. Int J Obes (Lond) 46(8): 1510-1517.
- Manasse SM, Flack D, Dochat C, Zhang F, Butryn ML, et al. (2017) Not so fast: The impact of impulsivity on weight loss varies by treatment type. Appetite 113: 193-199.
- Courtney AL, PeConga EK, Wagner DD, Rapuano KM (2018) Calorie information and dieting status modulate reward and control activation during the evaluation of food images. PLoS One 13(11): e0204744.
- Recio Román A, Recio Menéndez M, Román González MV (2020) Food reward and food choice. An inquiry through the liking and wanting model. Nutrients 12(3): 639.
- Carey M, Small H, Yoong SL, Boyes A, BIsquera A, et al. (2014) Prevalence of comorbid depression and obesity in general practice: a cross-sectional survey. Br J Gen Pract 64(620): e122-e127.
- Kress AM, Peterson MR, Hartzell MC (2006) Association between obesity and depressive symptoms among US Military active duty service personnel, 2002. J Psychosom Res 60(3): 263-271.
- Bremner JD, Moazzami K, Wittbrodt MT, Nye JA, Lima, et al. (2020) Diet, stress and mental health. Nutrients 12(8): 2428.
- Parletta N, Zarnowiecki D, Cho J, Wilson A, Bogomolova S, et al. (2019) A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr Neurosci 22(7): 474-487.
- Elran Barak R, Segel-Karpas D (2020) Dieting for weight-control among older adults: the role of perceived health and perceived overweight status. Eat Behavs 36: 101368.
- Littman AJ, Damschroder LJ, Verchinina L, Lai Z, Kim HM, et al. (2015) National evaluation of obesity screening and treatment among veterans with and without mental health disorders. Gen Hosp Psychiatry 37(1): 7-13.
- Bouzas C, Bibiloni MD M, Tur JA (2019) Relationship between body image and body weight control in overweight≥ 55-year-old adults: A systematic review. Int J Environ Res Public Health 16(9): 1622.
- Gray CM, Anderson AS, Clarke AM, Dalziel A, Hunt K, et al. (2009) Addressing male obesity: an evaluation of a group-based weight management intervention for Scottish men. Journal of Men's Health 6(1): 70-81.
- Fryer LK, Larson-Hall, Stewart J (2018) Quantitative methodology. In The Palgrave handbook of applied linguistics research methodology. Palgrave Macmillan, London, pp. 55-77.
- Creswell JW, Poth CN (2016) Qualitative inquiry and research design: Choosing among five approaches.
-
Joseph M Latham*, Stephen Berger, Gilly Koritzky, Terri Verone, Anna Morales, Christine Ma and Ian Gordon. Obesity and Weight Loss in Male Veterans. Open Access J Addict & Psychol 6(2): 2022. OAJAP.MS.ID.000632.
Obesity; Weight Loss; Male Veterans; Behavioral; Mental health; Cognitive; Public health; Sleep apnea; Cardiovascular disease; Healthcare
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






