 Research Article
Research Article
Mastery, Relatedness, and Substance Use: Applying Self-Determination Theory to Homeless Rehabilitation
Joshua Castleberry1*, Michael Leeman2, Justin Watts3 and Haley Moon4
1Department of Counselor Education and Supervision, Kent State University, USA
2Department of Communication Sciences and Disorders, Southeastern Lousiana University, USA
3Department of Rehabilitation Health Services, University of North Texas, USA
4Counseling and Psychological Services, Georgia State University, USA
Joshua Castleberry, Department of Counselor Education and Supervision, Kent State University, USA.
Received Date: August 04, 2023; Published Date: August 24, 2023
Abstract
Homelessness is a complex experience often involving loss, trauma, substance use, and is associated with increased psychiatric issues and decreased well-being. Factors associated with positive outcomes among the homeless population have received less attention in the counseling literature, lending less clarity to potential mechanisms which may improve mental health and substance related outcomes. In a sample of N = 104 homeless adults, we examined the impact of choice, mastery, and relatedness (factors in line with Social Determination Theory; SDT) on substance using behaviors, wellbeing and psychiatric symptoms. Hierarchical regression analyses indicated mastery was the most robust contributor to psychiatric symptoms and well-being, while relatedness accounted for more alcohol and drug use variance. Homeless services can potentially increase recovery outcomes by utilizing SDT concepts like choice, relatedness, and mastery. We conclude by discussing the implications for rehabilitation counselors and providers working with adults experiencing homelessness.
Keywords:Motivation; Choice; Recovery; Homelessness
Introduction
In the United States, approximately 580,000 individuals experience homelessness daily [1]. Homelessness is characterized as a series of losses, including health, shelter, relationships, employment, and well-being. Homeless individuals often face issues related to substance use (78%), mental illness (20%), exposure to traumatic events, stigmatization, and marginalization [2-4]. Homeless individuals also demonstrate increased rates of suicidal ideation and attempt, with 66% reporting suicidal ideation and 34% reporting a suicide attempt [5]. Furthermore, those experiencing homelessness have a significantly higher risk of chronic disease and disability and demonstrate increased mortality rates [6,7].
Even when homeless individuals seek supportive services to address issues related to substance use or mental health, they often encounter systemic barriers such as fragmented service delivery and inflexible appointment times, as well as attitudinal barriers such as judgmental staff, perceived prejudice, and rigid policies and application of rules. These barriers can influence treatment engagement and treatment dropout [8]. The complexity of issues faced by individuals who are homeless can significantly reduce their quality of life, making research outlining mechanisms that may support counseling interventions and improve recovery efforts a critical priority.
Therefore, it is important for researchers and service providers to focus on developing effective interventions that address the unique challenges faced by the homeless population. By addressing systemic and attitudinal barriers, and utilizing evidence-based interventions, counselors and service providers can support the recovery efforts of individuals who are homeless and help them to achieve a higher quality of life.
While Homelessness is a complex issue, and while some individuals who experience homelessness do return to housing, there are still over 100,000 individuals who experience chronic homelessness. These individuals face challenges related to chronic diseases or disabilities, such as severe mental illness, substance use disorder, or physical disabilities. The healthcare services available to these individuals are often confusing and overcrowded, leading to inadequate care, lack of engagement, and motivation [9-12]. However, with adequate support, recovery from homelessness is possible [13,14].
Recovery from homelessness involves addressing various issues, including physical health, substance use, mental illness, exposure to trauma, and interpersonal disturbances [15-21]. Additionally, housing initiatives and vocational development are essential for promoting recovery. However, research has shown that interventions promoting self-determination can facilitate recovery across various domains relevant to homelessness [18,22-24]. Giving individuals experiencing homelessness opportunities to make informed choices about treatment and care in trusted relationships increases their sense of control and promotes recovery [19,25].
Self-Determination Theory
Self-determination theory (SDT) is a macro-theory developed by Edward Deci and Richard Ryan in 2000, which provides a comprehensive framework for understanding motivation, development, and well-being. Central to SDT is the basic psychological need theory (BPNT), which identifies three fundamental psychological needs that are crucial for motivation: competence, relatedness, and autonomy. According to SDT, individuals are more likely to be motivated when their needs for competence, relatedness, and autonomy are fulfilled.
In the context of homeless services, motivation is a critical factor in predicting treatment outcomes. Unfortunately, the historical provision of services to homeless individuals has often relied on control, pressure, or coercion to motivate change, which has a tendency to increase disengagement. However, SDT provides a framework for promoting motivation towards recovery by focusing on concepts related to autonomy and supporting individuals to self-initiate change.
Research has investigated ways to promote basic psychological needs in various therapeutic and performance contexts. For example, Vallerand introduced the concept of autonomous support, which involves supporting individuals to self-initiate rather than exerting pressure to behave in particular ways. Practitioners can utilize autonomous support to positively affect motivation by taking on their client’s perspective, acknowledging their feelings and perceptions, and providing choice and meaningful rationale. Vallerand’s model has been applied successfully in diverse contexts such as work, substance use treatment, interpersonal relationships, homelessness, education, and sports.
Choice
Self-determination theory (SDT) researchers have identified choice as a crucial factor in promoting autonomous motivation [26- 28]. Autonomy support, introduced by Vallerand [28], encourages self-initiation rather than exerting pressure to behave in specific ways, and studies have shown that choice serves as autonomous support, resulting in positive outcomes, also known as “controlled choice” or “autonomous choice” [29-31]. Such research suggests that increased choice significantly influences physiological outcomes. For example, in a sample of 1,006 adults recruited through physician offices, choice increased perceived competence and motivation, leading to increased use of cessation medications and 6-month prolonged abstinence from tobacco [32].
Greenwood & Manning [33], conducted a longitudinal study (N = 197) examining autonomous support in a sample of individuals experiencing homelessness, focusing on choice and its relationship to mastery and psychiatric symptoms. Similarly, Manning & Greenwood [19], discovered that this relationship carried through several recovery domains (e.g., physical health, psychiatric symptoms, and community integration) in a similar sample of individuals experiencing homelessness (n = 160).
However, many homeless services impose administrative rules and regulations that restrict choice and limit agency, such as visitation policies that prohibit guests in rooms or require routine room checks [22,34,35]. These restrictions are often perceived as condescending and impede the agency of the service user. Although such rules are sometimes necessary for service facilitation, treatment providers can provide environmental support that restores an individual’s sense of mastery by offering choices and increasing perceived opportunities for personal control [26,36]. Hence, choice is essential in influencing outcomes and promoting well-being.
Mastery
Mastery, as defined by Pearlin & Schooler [37], is the belief that one possesses the skills, attributes, and knowledge to successfully meet life stressors and includes the perception of having control over them. Similarly, choice has been linked to positive outcomes [33], and mastery has been associated with well-being, hope, mental health functioning, empowerment, and recovery [38,39]. Given that mastery is susceptible to external forces, autonomous support can be used to promote its development [19,26]. Autonomous support can help individuals regain self-confidence and reclaim perceived control over their lives, while controlling environments may lead to the development or return to unhealthy coping strategies, such as avoidance or antisocial behavior [26].
Mastery may play a unique role in the relationship between relatedness and outcomes. For instance, Ramakrishnan & Masten [40], found that children experiencing homelessness with higher levels of mastery reported fewer socioemotional problems and more prosocial behavior. Similarly, in a sample of homeless individuals surveyed through the Homeless Enumeration and Survey project, Gory ML, et al. [41], found that mastery predicted depressive symptoms and mediated the effect of mental hospitalization and health on depression. Additionally, Manning & Greenwood [22], found that mastery mediated the relationship between choice and psychiatric symptoms in a sample of 101 homeless service users in Ireland. These findings align with self-determination theory, where higher scores in relatedness correspond to more positive relations and higher perceptions of social support, enhancing mastery. Although previous literature has linked motivation, social functioning, and mastery [42,43], these associations remain understudied among individuals experiencing homelessness.
Relatedness
Relatedness is a fundamental psychological need that has been linked to numerous psychological outcomes [26,44]. According to Self-Determination Theory (SDT), relatedness involves developing positive, fulfilling, and high-quality connections with others, fostering a sense of belonging and connectedness [26,45]. Past literature has emphasized the importance of relatedness in vocational rehabilitation service engagement and outcome literature [46]. Tansey TN, et al. [46], found that relatedness predicted autonomy and optimized the stages of change for employment in a sample of individuals with disabilities (N = 277), using the Working Alliance Inventory to measure relatedness. A meta-analysis conducted by Horvath [47,48], found that the working alliance predicted positive therapeutic outcomes, with an overall effect size (r = .275). Additionally, Tansey TN, et al. [46], evaluated a self-determination model of work motivation and found that relatedness played the most prominent role in facilitating change directly and indirectly on engagement and outcomes in a sample of people with disabilities (n = 277). This suggests that relatedness, or the therapeutic relationship between the counselor and client, was the strongest predictor of autonomy and treatment engagement. Furthermore, Osborn & Stein [49], investigated the relationship between provider directiveness, relatedness, and well-being, finding that relatedness was the most robust predictor of well-being in a sample of 60 adults with serious mental illness in an inpatient psychiatric hospital. These findings further suggest the importance of relatedness in promoting the well-being of individuals in recovery.
Research has highlighted the significance of enhancing social ties in psychiatric, traumatic, and substance use recovery domains related to experiences of homelessness [20,21,50]. Additionally, relatedness has been found to mediate the relationship between the low and high senses of autonomy in individuals with disabilities, suggesting that the service-provider-client relationship supersedes an individual’s perceived limitations, and higher relatedness levels predict a higher quality of life.
Given the unique needs of individuals experiencing homelessness (e.g., increased alcohol and drug use, emotional disorders, and worsening well-being), relatedness may be a crucial consideration for supporting their recovery. Therefore, supportive factors in recovery from homelessness are a critical counseling concern. The American Counseling Association (ACA) Code of Ethics calls for professional counselors to “honor diversity and embrace a multicultural approach in support of the worth, dignity, potential, and uniqueness of people within their social and cultural context.” Homelessness is a unique experience within social and cultural contexts that inherently deprives individuals of worth, dignity, and potential.
Recovery Outcomes
Homelessness poses a multitude of challenges, including traumatic experiences, problematic alcohol and drug use, social isolation, stigma, and exacerbated psychiatric symptoms [15,19]. Consequently, recovery from homelessness is a complex process that often requires addressing psychiatric symptoms, substance-related behaviors, and interpersonal issues that are associated with homelessness. Psychiatric symptoms and alcohol and drug use are primary domains that service providers use to measure outcomes and evaluate success [17]. Substance-related issues can lead to a loss of control, increased trauma, and emotional distress, and decreased service utilization among individuals experiencing homelessness. Additionally, the daily stressors of homelessness exacerbate psychiatric symptoms and increase substance use, prolonging homelessness.
Self-determination theory provides a useful framework for understanding how the variables of choice, mastery, and relatedness influence psychiatric symptoms, substance use, and well-being [19,25,26,51,52]. However, the connection between the effects of choice and the need for relatedness and mastery has yet to be fully explored [53]. While previous research has primarily focused on choice as a predictor of mastery [19], evidence suggests that relatedness is also crucial [54]. Thus, this study aims to clarify how these factors influence one another and impact recovery outcomes for individuals experiencing homelessness.
Present Study
The purpose of this study was to explore the role of choice, mastery, and relatedness regarding homeless service settings. Experiences of homelessness can result in feelings of powerlessness and isolation. Allowing for choice and working to build relationships in a service setting may be an effective way to help repair that damage and promote recovery in various domains. We fourth wanted to determine the ability of SDT constructs to contribute to the prediction of psychiatric symptoms, drug and alcohol use, and well-being among individuals experiencing homelessness. The researchers investigated the following research questions:
1. What are the associations between choice, mastery, relatedness, psychiatric symptoms, alcohol and drug use, and well-being?
2. What is the contribution of choice, mastery, and relatedness to the changes in psychiatric symptoms, alcohol and drug use, and well-being in a population of individuals experiencing homelessness?
We expect that:
Hypothesis 1. We predict that choice, mastery, and relatedness will correlate negatively with psychiatric symptoms and alcohol and drug use and correlate positively with well-being.
Hypothesis 2. We predict mastery will account for significant variance above and beyond choice and relatedness in psychiatric symptoms and alcohol and drug use. In contrast, relatedness will uniquely account for a significant amount of variance above and beyond choice and mastery in well-being.
Method
After obtaining IRB approval, we recruited participants aged 18 or older from two urban shelters in the southeastern U.S. Recruitment was conducted by a researcher, who presented the study details during classes and through posted flyers. The study took place during the COVID-19 pandemic, necessitating both online (Qualtrics) and in-person data collection. A total of 37 participants completed online surveys, and 71 completed in-person surveys, totaling 108 participants. Our final sample comprised 104 adults experiencing homelessness (66 women, 37 men, one other), who were ethnically diverse and primarily unemployed. Most had at least a high school education and received support services like food stamps.
Data collection included both service provider assessments and researcher surveys, encompassing measures like the Colorado Symptom Index, Global Appraisal of Individual Need Scale, and BBC Well-being Scale. Services provided to the participants were based on a continuum of care model. With the agreement of the service organization’s executive leadership, we gained access to client data. During the shelter lockdown, recruitment was conducted via flyers and informational sessions. Participants who consented completed surveys including the Consumer Choice survey, Pearlin’s Self-Mastery Scale, and Working Alliance Inventory. Collected data was matched with service organization data using a client-provided ID. All participants were compensated $5, regardless of survey completion.
Measures
Demographic Questionnaire: Demographic data included participants’ racial and ethnic identity, gender identity, and age. The questionnaire also asked participants to include their Client ID number for provider data collection purposes.
Choice: The Consumer Choice Scale [55], is a 15−item scale where participants report the amount of choice they perceive to have in the shelter regarding housing, treatment, and services. The measure has good internal consistency within a sample of individuals experiencing homelessness α = .94 [19]. Items measure perceptions of how much choice an individual has in housing in terms of place, who they room with, and how their home is decorated and furnished. These items also included choice in treatment, including the type of services and the choice to engage or not. Items are scored on a 5-point Likert scale from 1 (None) to 5 (Completely my choice), higher scores indicate more perceived choice. Sample items include how much choice do you perceive in “the people you live with,” “how you spend your day,” and “whether or not to participate in services.” The CCS demonstrated a high degree of internal consistency (α = .93) among this sample.
Mastery: Mastery was measured with the seven-item Pearlin Self-Mastery Scale [37]. Participants rate each item on a 4-point Likert scale (1 = strongly agree to 4 = strongly disagree), measuring a participant’s appraisal of mastery, with higher scores indicating higher perceived levels of mastery. A sample item includes “I have little control over the things that happen to me.” Five negative items are reverse-scored. This measure has been used with individuals experiencing homelessness and has shown acceptable internal consistency reliability α = .75 [19]. They demonstrated an acceptable level of internal consistency for this sample (α = .70).
Relatedness: Relatedness was evaluated using the Working Alliance Inventory-Short Revised [56,57], commonly used to measure relatedness in homeless populations [46,58]. The WAI-SR is a self-administered, 12-item assessment scored on a 5-point Likert scale from 1 (never) to 5 (always), where higher scores indicate greater relatedness. The tool elicits perceptions of the participant’s relationship with their service provider, including agreement on therapeutic goals and tasks, and the bond between client and provider. Participants were asked to reflect on their relationship with their primary service provider. Items were rephrased from first-person declarative to second-person interrogatory (e.g., “I feel uncomfortable with…” to “How often do you feel uncomfortable with…?”), allowing the survey to be read to clients in case management programs. The assessment focused on services provided at the facility, such as case management, housing services, meal access, substance use recovery groups, individual counseling, group counseling, education, and employment support. Specifically, the questions targeted the relationship formed in the context of these services. The WAI-SR shows strong psychometric properties demonstrating excellent internal consistency in this sample (α = .94).
Psychiatric Symptoms: Psychiatric symptoms were assessed by the Colorado Symptom Index [59]. The CSI is a 14−item brief, a self-report measure which asks participants to report the frequency with which they experience specific mental health symptoms. This measure has been used with individuals experiencing homelessness and shown excellent internal consistency α = .90 [19]. An example item is “How often have you felt nervous, tense, worried, frustrated, or afraid?” Items are answered with respect to how often one has experienced symptoms within the last month on a 5-point scale from 1 (not at all) to 5 (everyday). Sum scores on the CSI range from 14-70, with higher scores indicating greater frequency of psychiatric symptoms. The CSI had an excellent degree of internal consistency reliable among this sample (α = .90).
Alcohol and Drug Use: Substance use was assessed with the 6-item Substance Problem Subscale of the Global Appraisal of Individual Need Scale [60]. It has been used with persons experiencing homelessness [60]. This scale is used to measure the frequency of alcohol and drug use in the past month on a scale from 1 (0 times) to 6 (20-30 times). Higher sum scores indicate higher need for alcohol and drug use treatment. Alphas for this measure are not typically recorded due to qualitative differences between the different types of substances recorded [61]. The GAIN had a Cronbach’s alpha of .94 in this study.
Well-being: Well-being was assessed by the BBC Well-being scale [62], which is a 24-item self-report measure of well-being with three subscales (psychological well-being, physical health, and well-being and relationships). Items are scored on a 4-point Likert scale 1 (strongly disagree) to 4 (strongly agree), measuring a participant’s appraisal of well-being. A greater sum score is indicative of greater general well-being. This measure has been used with individuals experiencing serve mental illness either experiencing homelessness or at high risk of homelessness and shown excellent internal consistency α = .91 [49]. The BBC had excellent internal consistency reliability among this sample (α = .90).
Results
Preliminary Analysis
Power analysis: Consistent with Frazier et al. recommendations, a priori power calculations were conducted using G*Power [63], to provide guidance on the appropriate sample size to detect hypothesized main and interaction effects for correlation and regression analysis. The following input parameters were used a medium effect size (f2 = .15, 1-β err prob = .80, α = .05, 3 predictor variables), indicating a minimum total sample size of 98 was adequate to detect a meaningful effect. Our sample size of N = 104 was sufficient to achieve adequate power.
Prior to conducting the primary analyses, data were examined to ensure statistical assumptions were met for correlational and regression analysis. Examination of boxplots, and an analysis of standardized residuals indicated no extreme outliers (those falling outside of 3 standard deviations from the mean). In order to inspect patterns of missing data (2.4%), Little’s MCAR test was conducted indicating that data were missing completely at random 𝜒2 = 273.72, p = .135 [64,65]. Four participants were removed due to high levels (>50%) of missing data. Tests of univariate skewness and kurtosis of the residuals revealed that the distributions for all continuous variables were well within the parameters for univariate normality [66]. Tests to see if the data met the assumption of collinearity indicated that multicollinearity was not a concern (Choice, Tolerance = .91, VIF = 1.09; Mastery, Tolerance = .85, VIF = 1.17; Relatedness, Tolerance = .93, VIF = 1.07). Finally, data were screened for other potential violations of assumptions, including linearity, homoscedasticity using scatter plots, and independence of residuals (Psychiatric symptoms, Durbin-Watson = 1.88; Alcohol and Drug use, Durbin-Watson = 2.28; Well-being, Durbin-Watson = 1.91). Scatter plots of the standardized residuals and standardized predicted values of the dependent variable alcohol and drug use indicated a slight degree of heteroscedasticity.
The presence of heteroscedasticity may have implications such as generating biased standard error estimates, potentially leading to incorrect inferences from statistical tests including inflated Type I error rates [67]. Despite these potential risks, the researchers assessed these considerations and concluded that the observed level of heteroscedasticity was not substantial enough to present a significant concern. The reasoning for progressing despite the minor violation of the homoscedasticity assumption is primarily two-fold. First, the observed heteroscedasticity was only minor, thus reducing the chances of severe impacts on our results [68]. Secondly, the significant potential benefits of this research, including crucial contributions to understanding and treating alcohol and drug use, were deemed to outweigh the potential drawbacks of minor heteroscedasticity [69]. Therefore, the decision was made to proceed with the data analysis, being mindful of the slight heteroscedasticity when interpreting the results.
Primary Analysis
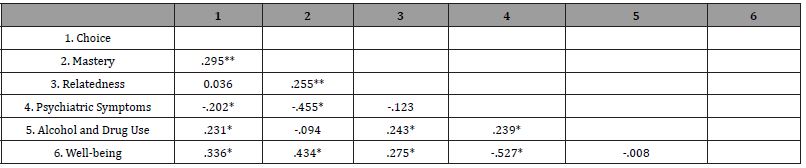
Pearson’s correlation coefficients were calculated to test the first hypothesis that choice, mastery, and relatedness would correlate negatively with psychiatric symptoms, alcohol and drug use, and positively to well-being, excluding cases pairwise. Findings indicated significant correlations among a number of study variables (Table 1). Choice and mastery were negatively and moderately correlated with psychiatric symptoms (Choice, r = − .202, p = .039; Mastery, r = − .455, p = .000). Choice, mastery, and relatedness were positively and moderately correlated with well-being (Choice, r = .336, p = .000; Mastery, r = .434, p = .000; Relatedness, r = .275, p = .005). Additionally, choice and relatedness were positively correlated with alcohol and drug use (Choice, r = .231, p = .018; Relatedness, r = .243, p = .013). Amongst the independent variables choice and relatedness were positively and moderately correlated to mastery (Choice, r = .295, p = .002; Relatedness, r = .255, p = .009) while choice and relatedness were not significantly correlated. This pattern indicates that as choice, mastery, and relatedness increased, so did well-being, while psychiatric symptoms decreased as choice and mastery increased. These findings partially support our first hypothesis.
Table 1:Correlations for Study Constructs.
The second hypothesis was that mastery accounts for a significant amount of variance in psychiatric symptoms and alcohol and drug use, and relatedness would uniquely account for a significant amount of variance in well-being. To test this hypothesis, we conducted a series of hierarchical regression analyses on our three dependent variables (Psychiatric symptoms, Alcohol and Drug Use, and Wellbeing). First, the researchers entered choice in Step 1 as it is the theorized autonomous support promoting mastery and relatedness [19]. Researchers then entered mastery in Step 2 as previous work has shown it is a predictor of our recovery outcomes [33,51]. Finally, relatedness was entered in Step 3 as it is the newest variable to be tested in this model (Tables 2-4).
Table 2:Hierarchical Linear Regression Analyses for Psychiatric Symptoms.
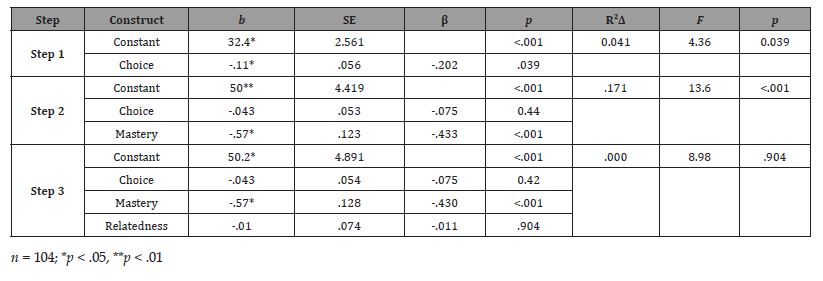
Table 3:Hierarchical Linear Regression Analyses for Alcohol and Drug Use.
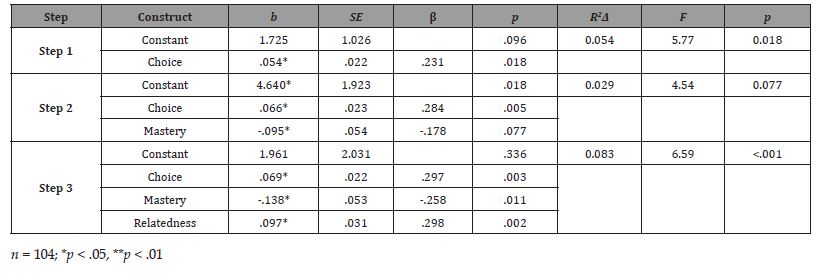
Table 4:Hierarchical Linear Regression Analyses for Well-being.
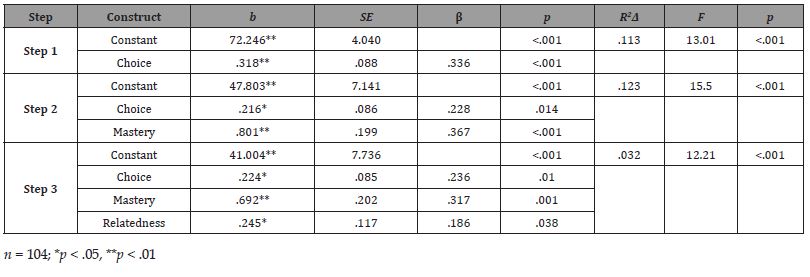
With psychiatric symptoms (CSI) as the dependent variable, choice (CCS) predicted 4.1% of the variance in Step 1 (R2Δ = .041, FΔ = 4.360, p = .039), mastery (MSS) predicted 17.1% of the variance in Step 2 (R2Δ = .171, FΔ = 21.960, p = .000), and relatedness (WAI) did not predict a significant amount of variance in Step 3 (R2Δ = .000, FΔ = .015 p = .904; see Table 2). With alcohol and drug use (GAIN) as the dependent variable, choice (CCS) predicted 5.4% of the variance in Step 1 (R2Δ = .054, FΔ = 5.776, p = .018), mastery (MSS) did not predict alcohol and drug use (GAIN) in Step 2 (R2Δ = .029, FΔ = 3.183, p = .077). However, Relatedness (WAI) predicted 8.3% of the variance in Step 3 (R2Δ = .083, FΔ = 9.908, p = .002) (Table 3). Finally, with well-being (BBC) as the dependent variable, choice (CCS) predicted 11.3% of the variance in Step 1 (R2Δ = .113, FΔ = 13.017, p = .000), mastery (MSS) predicted 12.3% of the variance in Step 2 (R2Δ = .123, FΔ = 16.240, p = .000), and relatedness (WAI) predicted 3.2% of the variance in Step 3 (R2Δ = .032, FΔ = 4.398, p = .038) (Table 4). Thus, hypothesis 2 was partially supported.
Discussion
As the first study to examine the effect of choice, mastery, and relatedness on the recovery outcomes of psychiatric symptoms, alcohol and drug use, and well-being in individuals engaging in homeless services, our findings make a significant contribution to the existing literature. For the first research question, the associations uncovered largely affirm previous findings that choice, mastery, and relatedness are correlated with recovery outcomes including psychiatric symptoms, alcohol, and drug use, and well-being [22,70,71]. Choice and mastery were negatively correlated with psychiatric symptoms and positively correlated with well-being. As participants’ choice and mastery increased, their observed psychiatric symptoms decreased, and their well-being increased. A surprising finding was the significant positive correlation between the variables’ choice and relatedness to alcohol and drug use. While unexpected, these results are not unique as Manning & Greenwood [19], previously found a nonsignificant positive correlation between alcohol use and mastery amongst individuals experience homelessness. This study also found a unique relationship between choice and alcohol and drug use that mirrors the findings of Manning & Greenwood [19], between choice and mastery.
Consequently, we cannot differentiate if these relationships are with the use of alcohol or with drugs. Additionally, relatedness did not correlate with psychiatric symptoms, though it significantly correlated with well-being and alcohol and drug use. These findings are not surprising as prior work has shown relatedness to be a poor predictor of symptom reduction and more closely associated with growth-related variables such as well-being [52]. One explanation of these findings is that service consumers frequently underreport alcohol and drug use in homeless service settings [3,61]. This underreporting may result from a lack of trust between consumer and provider. Self-determination theory indicates that when relatedness fosters autonomous motivation, feelings of trust and safety are promoted. Our findings suggest that participants who reported greater relatedness were more self-determined, thus more likely to feel safe to disclose alcohol and drug use.
Overall, our findings show that increased choice, mastery, and relatedness in our sample was significantly related to reductions in psychiatric symptoms and higher levels of well-being. This finding is consistent with previous research showing the relationship between choice, mastery, and recovery in individuals experiencing homelessness [19,22], and generalizes beyond psychiatric symptoms to well-being. Our findings are also consistent with self-determination theory [54] and highlight the importance of attending to the need for relatedness in providing services to individuals experiencing homelessness. These findings indicate that perceived choice, mastery, and relatedness are critical in these recovery outcomes. Services that aim to prompt recovery from homelessness should prioritize approaches that offer choice and nurture belonging and connectedness.
This study is unique in that it is the first to examine the relationship between choice, mastery, relatedness, and recovery outcomes with adults experiencing homelessness who are engaged in services that are provider-led in their structure. When combined with the added effect of relatedness, positive outcomes promote psychiatric symptom reduction, alcohol and drug use, and enhanced well-being. This study adds to a body of literature used to advocate for choice amongst homeless services by adding the contribution of relatedness. This is also important in highlighting that, where choices may be limited, mastery is still being developed. In the absence of choice, relatedness significantly acts as a buffer to psychiatric symptoms while promoting well-being. The literature is well-supported in its claims that choice is essential to recovery [19,70]. As choices are limited in homeless services that rely on abstinence and compliance with rules and regulations, mastery could be stripped away. Our findings suggest that, even in these settings, choice can still promote the development of mastery. With efforts to foster relatedness, services may still promote self-determination amongst their service users.
Implications for Rehabilitation Counseling Practice
Rehabilitation counselors are likely to encounter clients who may experience housing insecurity or homelessness due to the high rates of chronic disease, disability, employment issues, and mental health related issues among those experiencing homelessness [3,6]. Individuals experiencing homelessness are significantly more likely to disengage from services (whether this is treatment disengagement or dropout), making identifying mechanisms which can enhance treatment engagement worthwhile. While issues related to homelessness have received less attention in the counseling literature, the current study provides a starting point for working with those experiencing homelessness who demonstrate substance related or mental health issues. The current study emphasized concepts like choice, relatedness and mastery, which are in line with a significant number of strength-based theoretical approaches in the rehabilitation counseling field, including person centered approaches, motivational interviewing and SDT, adding to the body of literature that advocates for choice and relatedness in homeless services [8,33]. This study highlights the central role of relatedness and mastery and the supportive role of choice in the recovery process as it relates to improvements in well-being, psychiatric symptoms and drug and alcohol use among individuals experiencing homelessness. Since all three are significantly associated with recovery outcomes, interventions should focus on choice, relatedness and mastery to enhance self-determination among adults experiencing homelessness. Practitioners would do well to create a therapeutic environment in which they dialog with clients, support them in choosing and attaining their own goals, and agree on paths and supports to attaining those goals. Through the working alliance, clinicians can support clients’ need for relatedness, thus enhancing their recovery outcomes. In addition to a strong focus on the working alliance, rehabilitation counselors should also consider peer-support groups as an additional layer of support for clients with substance use disorders as they provide recovery-oriented, social support network that focuses on attaining and sustaining recovery efforts [72].
Additionally, counselors trained in motivational interviewing [8], may increase perceived choice, thus supporting a client’s mastery. Motivational interviewing seeks to enhance self-determination by intrinsically motivating clients to change problematic behavior through exploring and resolving ambivalence. As motivation is a critical variable in enhancing treatment outcomes in homeless services, person-centered approaches like MI, which emphasize collaboration, and relatability (on the part of the practitioner) have shown significant moderate effects on issues related to substance use and mental health, even for clients who demonstrate high levels of distress [73]. It is important to mention that although employment is a major goal of vocational rehabilitation, application of MI would involve collaboratively setting goals (i.e., not necessarily pushing toward change) with clients which could include a variety of factors (many of which would need to be addressed before successful employment could be attained). Further in light of the high rates of trauma among this population, practitioners and agencies working with homeless adults should engaged in trauma-informed practice, which has also shown to enhance treatment outcomes [74].
Limitations and Suggestions for Future Research
Findings from this study should be considered in light of a few limitations. First, this data was collected during the COVID-19 pandemic, as such, survey responses may be affected by the changing landscape of health concerns. Our sample was also a convenience sample (not randomized), which limits generalizability of findings. Finally, service providers experienced a 70% loss in service users during this study due to CDC-guided restrictions. It could be that the participants who self-selected into our study were further along in their recovery journey and were more motivated to engage in services, and so were more willing to talk about their experiences relative to other homeless individuals who left service due to increased restrictions, or whom may still be battling addiction or coping with trauma. Our sample is likely not representative of the subgroup from which they were drawn or representative of the population of homeless services users. However, given the similarity of our findings to those of other studies [19], we believe our findings do have some generalizability to individuals experiencing homelessness in different contexts and service structures.
Additionally, this study used cross-sectional, correlational designs. Thus, causal conclusions should not be made. Although the data were consistent with the theoretical model of self-determination, other models may be consistent with the data. Additionally, recovery can have unpredictable paths in which individuals experience setbacks in addition to forwarding progress. Longitudinal research is necessary to uncover further the nature of these relationships, as well as following the recovery journey in homelessness over time could address causality.
Conclusion
These findings, together with previous research [19,22,71], expand on the importance of choice, mastery, and relatedness to recovery (e.g., psychiatric symptoms, alcohol and drug use, and well-being) among homeless services users. Furthermore, the present study extends previous research by examining a growth-related dimension of recovery (e.g., well-being) and differences in relationships between the counselor and client (e.g., relatedness). This finding suggests that preserving homeless service users’ choices is essential as it will directly affect their well-being.
Additionally, in a context where choice cannot be preserved, relatedness may act as a buffer, along with mastery, against psychiatric symptoms and alcohol and drug use and promote well-being. It would benefit service providers and clinicians to invest in ways to engage with their clients, identify which build trust, and offer opportunities to develop relatedness. This work adds to the body of literature focusing on identifying support for homeless people and developing ways in which service providers can interact with this population to promote recovery and develop policies that will reduce the negative impact of homelessness.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- The U.S. Department of Housing and Urban Development: Office of Community Planning and Development (2020) The 2018 Annual Homeless Assessment Report (AHAR) to Congress.
- Iwanaga K, Umucu E, Wu JR, Yaghmaian R, Lee HL, et al. (2017) Assessing vocational outcome expectancy in individuals with serious mental illness: A factor-analytic approach. J Mental Health 29(1): 116-123.
- O'Toole TP, Conde-Martel A, Gibbon JL, Hanusa BH, Freyder PJ, et al. (2004) Substance-abusing urban homeless in the late 1990s: How do they differ from non-substance-abusing homeless persons? Journal of Urban Health 81(4): 606-617.
- Tsemberis S, Eisenberg RF (2000) Pathways to housing: supported housing for street-dwelling homeless individuals with psychiatric disabilities. Psychiatr Serv 51(4): 487-493.
- Eynan R, Langley J, Tolomiczenko G, Rhodes AE, Links P, et al. (2002) The association between homelessness and suicidal ideation and behaviors: Results of a cross-sectional survey. Suicide Life Threat Behav 32(4): 418-427.
- Davies BR, Allen NB (2017) Trauma and homelessness in youth: Psychopathology and intervention. Clin Psychol Rev 54: 17-28.
- Fischer PJ, Breakey WR (1991) The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol 46(11): 1115.
- Miller JA, Carver H, Masterton W, Parkes T, Maden M, et al. (2021) What treatment and services are effective for people who are homeless and use drugs? A systematic ‘review of reviews’. PLoS One 16(7): e0254729.
- Muñoz M, Vázquez C, Bermejo M, Vázquez JJ (1999) Stressful life events among homeless people: Quantity, types, timing, and perceived causality. Journal of Community Psychology 27(1): 73-87.
- Terry M, Gurpreet B, Patel N (2010) Healthcare needs of homeless youth in the United States. J Pediatr Sci 2(1).
- Felner RD, Farber SS, Primavera J (1983) Transitions and stressful life events: A model for primary prevention. In: RD Felner, LA Jason, JN Moritsugu, SS Farber (Eds). Preventive psychology: Theory, research and practice. Pergamon Press, pp. 199-215.
- Thoits PA (1982) Conceptual, methodological, and theoretical problems in studying social support as a buffer against life stress. J Health Soc Behav 23(2): 145-159.
- Liberman MC, Gao J, HeDZ, Wu X, Jia S, et al. (2002) Prestin is required for electromotility of the outer hair cell and for the cochlear amplifier. Nature 419(6904): 300-304.
- Polcin DL (2009) A model for sober housing during outpatient treatment. J Psychoactive Drugs 41(2): 153-1561.
- Anthony WA (1993) Recovery from mental illness: The guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal 16(4): 11-23.
- Carlson EB, Dalenberg CJ (2000) A conceptual framework for the impact of traumatic experiences. Trauma, Violence, & Abuse 1(1): 4-28.
- Green CA, Yarborough MT, Polen MR, Janoff SL, Yarborough BJH (2015) Dual recovery among people with serious mental illnesses and substance problems: A qualitative analysis. J Dual Diag 11(1): 33-41.
- Johnstone M, Parsell C, Jetten J, Dingle G, Walter Z (2016) Breaking the cycle of homelessness: Housing stability and social support as predictors of long-term well-being. Housing Studies 31(4): 410-426.
- Manning RM, Greenwood RM (2019) Recovery in homelessness: The influence of choice and mastery on physical health, psychiatric symptoms, alcohol and drug use, and community integration. Psychiatr Rehabil J 42(2): 147-157.
- Urcuyo KR, Boyers AE, Carver CS, Antoni MH (2005) Finding benefit in breast cancer: Relations with personality, coping, and concurrent well-being. Psychology & Health 20(2): 175-192.
- Whitley R, Drake RE (2010) Recovery: A dimensional approach. Psychiatr Serv 61(12): 1248-1250.
- Greenwood RM, Manning RM (2017) Mastery matters: Consumer choice, psychiatric symptoms and problematic substance use among adults with histories of homelessness. Health Soc Care in the Community 25(3): 1050-1060.
- Martins P, Ornelas J, Silva AC (2016) The role of perceived housing quality and perceived choice to recovery: An ecological perspective on a housing first program in Lisbon. Journal of Environmental Psychology 47: 44-52.
- Shank JW, Iwasaki Y, Coyle C, Messina ES (2015) Experiences and meanings of leisure, active living, and recovery among culturally diverse community-dwelling adults with mental illness. American Journal of Psychiatric Rehabilitation 18(2): 129-151.
- Krabbenborg MA, Boersma SN, van der Veld WM, Vollebergh WA, Wolf JR (2017) Self-determination in relation to quality of life in homeless young adults: Direct and indirect effects through psychological distress and social support. The Journal of Positive Psychology 12(2): 130-140.
- Deci EL, Ryan RM (2000) The "what" and "why" of goal pursuits: Human needs and the self-determination of behavior. Psychological inquiry 11(4): 227-268.
- Gagne M (2003) Autonomy support and need satisfaction in the motivation and well-being of gymnasts. Journal of Applied Sport Psychology 15(4): 372-390.
- Vallerand RJ (1997) Toward a hierarchical model of intrinsic and extrinsic motivation. In: MP Zanna (Ed). Advances in experimental social psychology. 29: 271-360, Elsevier.
- Mancini MA (2007) The role of self–efficacy in recovery from serious psychiatric disabilities: A qualitative study with fifteen psychiatric survivors. Qualitative Social Work 6(1): 49-74.
- Sterling RC, Gottheil E, Glassman SD, Weinstein SP, Serota RD, et al. (2001) Correlates of employment: A cohort study. Am J Drug Alcohol Abuse 27(1): 137-146.
- Tafarodi RW, Milne AB, Smith AJ (1999) The confidence of choice: Evidence for an augmentation effect on self-perceived performance. Personality and Social Psychology Bulletin 25(11): 1405-1416.
- Williams GC, McGregor HA, Sharp D, Levesque C, Kouides RW, et al. (2006) Testing a self-determination theory intervention for motivating tobacco cessation: Supporting autonomy and competence in a clinical trial. Health Psychol 25(1): 91.
- Greenwood RM, Schaefer-McDaniel NJ, Winkel G, Tsemberis SJ (2005) Decreasing psychiatric symptoms by increasing choice in services for adults with histories of homelessness. Am J Community Psychol 36(3–4): 223-238.
- Cornes M, Manthorpe J, Joly L, O'Halloran S (2014) Reconciling recovery, personalization and Housing First: Integrating practice and outcome in the field of multiple exclusion homelessness. Health Soc Care in the Community 22(2): 134-143.
- Lyon-Callo V (2008) Inequality, poverty, and neoliberal governance: Activist ethnography in the homeless sheltering industry. University of Toronto Press, Canada.
- White S (2001) New labour: the progressive future?
- Pearlin L, Schooler C (1978) The structure of coping. J Health Soc Behav 19(1): 2-21.
- Badger TA (1993) Physical health impairment and depression among older adults. Image J Nurs Sch 25(4): 325-330.
- Rosenfield S (1997) Labeling mental illness: The effects of received services and perceived stigma on life satisfaction. American Sociological Review 62(4): 660-672.
- Ramakrishnan JL, Masten AS (2020) Mastery motivation and school readiness among young children experiencing homelessness. American Journal of Orthopsychiatry 90(2): 223-235.
- Gory ML, Ritchey F, Fitzpatrick K (1991) Homelessness and affiliation. The Sociological Quarterly 32(2): 201-218.
- Baumeister RF, Vohs KD, Tice DM (2007) The strength model of self-control. Current Directions in Psychological Science 16(6): 351-355.
- Furrer C, Skinner E (2003) Sense of relatedness as a factor in children's academic engagement and performance. Journal of Educational Psychology 95(1): 148-162.
- Ryff CD, Singer B (1998) The contours of positive human health. Psychological Inquiry 9(1): 1-28.
- Ryan RM (1993) Agency and organization: Intrinsic motivation, autonomy, and the self in psychological development. In: J. E Jacobs (Ed). Nebraska Symposium on Motivation, 1992: Developmental perspectives on motivation. pp:1-56.
- Tansey TN, Iwanaga K, Bezyak J, Ditchman N (2017) Testing an integrated self-determined work motivation model for people with disabilities: A path analysis. Rehabil Psychol 62(4): 534-544.
- Horvath AO, Del Re A, Flückiger C, Symonds D (2011) Alliance in individual psychotherapy. Psychotherapy 48(1): 9-16.
- Horvath AO, Greenberg LS (1989) Development and validation of the working alliance inventory. Journal of Counseling Psychology 36(2): 223-233.
- Osborn LA, Stein CH (2018) Recovery-oriented services in an inpatient setting: The role of consumers' views of therapeutic alliance and practitioner directiveness on recovery and well-being. Am J Orthopsychiatry 89(1): 115-123.
- White MK (2007) Maps of narrative practice. WW Norton & Company.
- Ng JY, Ntoumanis N, Thøgersen-Ntoumani C, Deci EL, Ryan RM, et al. (2012) Self-determination theory applied to health contexts: A meta-analysis. Perspect Psychol Sci 7(4): 325-340.
- Reis HT, Sheldon KM, Gable SL, Roscoe J, Ryan RM (2000) Daily well-being: The role of autonomy, competence, and relatedness. Personality and Social Psychology Bulletin 26(4): 419-435.
- Katz I, Assor A (2007) When choice motivates and when it does not. Educational Psychology Review 19(4): 429.
- Ryan RM, Deci EL (2008) A self-determination theory approach to psychotherapy: The motivational basis for effective change. Canadian Psychology/Psychologie Canadienne 49(3): 186-193.
- Srebnik D, Livingston J, Gordon L, King D (1995) Housing choice and community success for individuals with serious and persistent mental illness. Community Ment Health J 31(2): 139-152.
- Busseri MA, Tyler JD (2003) Interchangeability of the working alliance inventory and working alliance inventory, short form. Psychol Assess 15(2): 193-197.
- Hatcher RL, Gillaspy JA (2006) Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research 16(1): 12-25.
- Stergiopoulos V, Gozdzik A, O'Campa P, Holtby AR, Jeyaratnam J, et al. (2014) Housing First: Exploring participants' early support needs. BMC Health Serv Res 14: 167.
- Shern DL, Wilson NZ, Coen AS, Patrick D C, Foster M, et al. (1994) Client outcomes II: Longitudinal client data from the Colorado treatment outcome study. Milbank Q 72(1): 123-148.
- Dennis ML, Titus J, White M, Unsicker J, Hodgkins D (2002) Global appraisal of individual needs-initial (GAIN-I). Chestnut Health Systems.
- Morral AR, McCaffrey DF, Beighley C, Mukherji A, Ridgeway G (2006) The relative effectiveness of 10 adolescent substance abuse treatment programs in the United States. 346: Rand Corporation.
- Kinderman P, Schwannauer M, Pontin E, Tai S (2011) The development and validation of a general measure of well-being: The BBC well-being scale. Qual Life Res 20(7): 1035-1042.
- Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 41(4): 1149-1160.
- Little RJ (1988) A test of missing completely at random for multivariate data with missing values. Journal of the American statistical Association 83(404): 1198-1202.
- Fichman M, Cummings JN (2003) Multiple imputation for missing data: Making the most of what you know. Organizational Research Methods 6(3): 282-308.
- Chou CP, Bentler PM (1995) Estimates and tests in structural equation modeling. In R. H. Hoyle (Ed.), Structural equation modeling: Concepts, issues, and applications. pp. 37-55.
- Long JS, Ervin LH (2000) Using heteroscedasticity consistent standard errors in the linear regression model. The American Statistician 54(3): 217-224.
- Hayes AF, Cai L (2007) Using heteroskedasticity-consistent standard error estimators in OLS regression: An introduction and software implementation. Behav Res Methods 39(4): 709-722.
- Neter J, Kutner MH, Nachtsheim CJ, Wasserman W (1996) Applied linear statistical models.
- Inguglia C, Ingoglia S, Liga F, Coco AL, Cricchio MGL (2015) Autonomy and relatedness in adolescence and emerging adulthood: Relationships with parental support and psychological distress. Journal of Adult Development, 22(1): 1-13.
- Tsemberis S, Gulcur L, Nakae M (2004) Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health 94(4): 651-656.
- O’Sullivan D, Blum J, Watts J, Bates J (2015) SMART recovery: Continuing care considerations for rehabilitation counselors. Rehabilitation Counseling Bulletin 58(4): 203-216.
- Lundahl B, Kunz C, Brownell C, Tollefson D, Burke B (2010) Meta analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice 20(2): 137-160.
- O’Sullivan D, Watts J, Strauser D (2019) Trauma-sensitive rehabilitation counseling: Paradigms and principles. Journal of Vocational Rehabilitation 51(3): 299-312.
-
Joshua Castleberry*, Michael Leeman, Justin Watts and Haley Moon. Mastery, Relatedness, and Substance Use: Applying Self-Determination Theory to Homeless Rehabilitation. Open Access J Addict & Psychol 7(3): 2023. OAJAP.MS.ID.000664.
Leadership; Managers; Dark leadership; Leader–member exchange; Dark traits; Personality; High-quality relationships; Psychopathy; Machiavellianism; Psychological maturity
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






