 Conceptual Paper
Conceptual Paper
Leading from Post Covid Stress Disorder Toward Post Covid Growth
Gary B. Bailey, MA, MSW, Ph.D., LCSW, CEAP*
Lecturer, School of Social Work, NC State University, USA
Gary B. Bailey, MA, MSW, Ph.D., LCSW, CEAP, Owner and clinical director of Alamance Life Works EAP, PLLC in Burlington, NC 27217, USA. Lecturer, School of Social Work, NC State University, USA
Received Date: September 16, 2022; Published Date: May 22, 2023
Abstract
This article examines the impact of Covid-19 on society using the lenses of micro, mezzo, and macro levels. Moreover, the writer’s research on emotional intelligence will focus primarily on a micro lens level Thus, seven strategies for leading individuals, groups, and organizations from Post- Covid Stress Disorder (PCSD) toward Post Covid Growth (PCG) will be introduced. Finally, the authors acknowledge that the terms PCSD and PCG have not been defined in the literature. However, we propose that these terms be used because of the impact this disease has and will shape society on micro, mezzo, and macro levels historically and in the future.
Introduction
The experience of Covid-19 and its variants on society has had its impact on all aspects of society from macro, mezzo, and micro levels. This microscopic virus has disrupted economic, educational, business, and health care systems all over the world. The residual impact of the virus is impacting levels of both the physical and emotional states throughout the world. For example, anxiety and depressive symptoms reported to the US Census Bureau, Household Pulse Survey increased from May to June 2020 by approximately 6% [1,2]. In addition, this has affected health care workers specifically, mental health therapists dramatically. This article will examine this impact and what it will take to reach post covid growth (PCG).
Post-traumatic stress disorder (PTSD) is a disorder that develops in some people who have experienced a shocking, scary, or dangerous event. Covid-19 has impacted families and significant others with serious physical and emotional levels synonymous with these events. It is natural to feel afraid during and after traumatic situations. Moreover, events around perceived threats elicit the emotion of fear which in turn triggers many split-second changes in the body to help defend against danger or to avoid it. This “fight-orflight” response is a typical reaction meant to protect a person from harm. Nearly everyone will experience a range of reactions after trauma, yet most people recover from initial symptoms naturally. Those who continue to experience problems may be diagnosed with PTSD. People who have PTSD may feel stressed or frightened, even when they are not in danger. Not only has the mental and emotional response to this been noticed but there are also research articles and books written on the emotional impact on the physical body in response to the actual disease of Covid-19 [2,3].
While most but not all traumatized people experience shortterm symptoms, the majority do not develop ongoing (chronic) PTSD. In addition, not everyone with PTSD has been through a dangerous event. Some experiences, like the sudden, unexpected death of a loved one, can also cause PTSD. Symptoms usually begin early, within 3 months of the traumatic incident, but sometimes they begin years afterward. Symptoms must last more than a month and be severe enough to interfere with relationships or work to be considered PTSD. The course of the illness varies. Some people recover within 6 months, while others have symptoms that last much longer. In some people, the condition becomes chronic. A mental health professional who has experience helping people with mental illnesses, such as a clinical social worker, psychiatrist, or psychologist, can diagnose PTSD. To be diagnosed with PTSD, an individual must have all the re-experiencing mood symptoms such as flashbacks of reliving the trauma over and over, including physical symptoms like a racing heart or sweating, bad dreams, and frightening thoughts. Re-experiencing symptoms may cause problems in a person’s everyday routine. The symptoms can start from the person’s thoughts and feelings. Words, objects, or situations that are reminders of the event can also trigger re-experiencing symptoms. Avoidance symptoms include staying away from places, events, or objects that are reminders of the traumatic experience and avoiding thoughts or feelings related to the traumatic event.
Things that remind a person of the traumatic event can trigger avoidance symptoms. These symptoms may cause a person to change their routine. For example, after having been isolated from being either exposed or having the actual Covid-19 symptoms, one’s arousal state of being easily startled, feeling tense or “on edge”, having difficulty sleeping, and having angry outbursts. Arousal symptoms are usually constant, instead of being triggered by things that remind one of the traumatic events. These symptoms can make the person feel stressed and angry. They may make it hard to do daily tasks, such as sleeping, eating, or concentrating.
Covid-19 residual effects such as what is referred to as “brain fog” may result in cognition and mood symptoms such as trouble remembering key features of the traumatic event, negative thoughts about oneself or the world, distorted feelings like guilt or blame if a loved one becomes seriously ill or dies. Further symptoms can lead to loss of interest in enjoyable activities and further cognition and mood symptoms can begin or worsen. Furthermore, an individual may have increased substance use after the isolation from being exposed or having experienced having the virus. These symptoms can make the person feel alienated or detached from friends or family members. Although there have been signs of increased use of mental health services, there are several individuals who have experienced what is known as post-traumatic growth (PTG) [4].
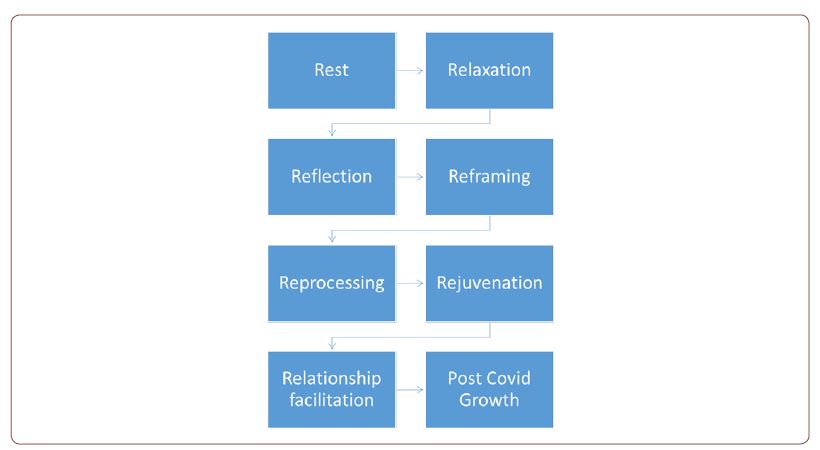
PTG is the positive psychological change that some individuals experience after a life crisis or traumatic event. Post-traumatic growth was identified by psychologists Richard Tedeschi and Lawrence Calhoun in the 1990s. PTG is not a denial of deep distress but rather suggests that adversity could have an unintentional effect of causing changes in understanding oneself, others, and the world. Post-traumatic growth can co-exist with post-traumatic stress disorder. This writer suggests that one could potentially increase the chances of transforming the negative reactions of PTSD to PTG by having wellness days. Wellness days are days for persons to practice 7 (seven) Rs — Rest, Relaxation, Reflection, Reframing, Reprocessing, Rejuvenation, and Relationships facilitation. These seven Rs are defined in detail next.
Rest
The first R is rest. Rest is important for better health overall including increased concentration and memory, a healthier immune system, reduced stress, improved mood, and even a better metabolism. The next R is relaxation.
Relaxation
Relaxation is taking both the physical and psychological time to distress without distractions. There should be only visual, auditory, and kinaesthetic sensory input that causes the body to be in a calming state Another R is reflection.
Reflection
Reflection is to think actively about one’s thoughts, feelings, and behavior during the day and what one has gained from those positive highs during the day, and then to journal about one’s thoughts, feelings, and behavior listing in detail or making a list of the former. This also requires a sense of gratitude for what you have and not for what you do not have.
Reframing
Reframing the experience is paying close attention to the opportunities for growth that accompany stress and choosing those situations that have personal value. It is also noticing how you perceive the stressor, and regulating your physiological response, such as doing biofeedback or simply taking one’s blood pressure while breathing deeply to see if you notice the blood pressure level decreasing.
Reprocessing
Reprocessing memories or unconscious information can be done by utilizing several mechanisms either external or internal means. This process may be more difficult if one has a complicated traumatic past. If this is the case, a skilled therapist may assist in this processing by utilizing somatic experiencing therapies such as eye movement desensitization reprocessing or EMDR, Brain Spotting, or Flash techniques.
Rejuvenation
Rejuvenation is a way of recuperation by taking the time by creating space in one’s schedule in a proactive way recognizing that this space is like the space between two musical notes and is as important as the note before and after the space. It is also a renewal of the energy that revitalizes and recharges the positive spirit that lies within each of us that would allow room for regrowth or PTG. Finally, the last R recommended is relationship facilitation.
Relationships Facilitation
Relationships facilitation would be joining a group of likeminded or bodied people with similar experiences or goals. The group experience is a powerful way of synergistically connecting to other people that is therapeutic and enlightening by utilizing the power of the group. This also helps to facilitate post-covid growth. The following graphic illustration is not meant as a sequential continuum as either of the Rs could be practiced before, after or simultaneously”. The graphic illustration is as follows:
Conclusion
In conclusion, this article has been condensed primarily from a micro perspective. However, this framework could be applied as a template for the mezzo and macro levels based on parallel processes for organizations. Every individual is unique in their journey from PTSD to PTG. If either of the 7 (seven) (R) strategies Rs — Rest, Relaxation, Reflection, Reframing, Reprocessing, Rejuvenation, and Relationships facilitation are difficult to process or practice, a licensed mental health professional may be indicated. The Covid-19 pandemic has caused many challenges but also some new opportunities for Regrowth. Just as pruning away dead branches on a tree or plant facilitates healthier growth, so can the changing of old thoughts, feelings, and behaviors. The primary author and other writers have researched how emotional intelligence is positively correlated with transformational leadership for individuals and organizations [5-10]. Finally, the process of increasing one’s emotional awareness can be a transformative experience. If there are questions about this process, the writers may be contacted at the email addresses in this article [11].
Acknowledgement
None.
Conflict of interest
None of the authors have a conflict of interest.
References
- Hellebuyck M, Halpern M, Nguyen T, Fritze D (2019) 2019 State of Mental Health in America Report. Mental health America.
- The Department of Health and Human Services (2018) The U.S. health workforce chartbook part IV: Behavioral and allied health. HRSA.
- Van DKB (2014) The body keeps the score: Brain, mind, and body in the healing of trauma.
- Porges SW, Dana D (2018) Clinical applications of the polyvagal theory: The emergence of polyvagal-informed therapies. Prati LM, Karriker JH (2010) Emotional intelligence skills: The building blocks of defense against emotional labor burnout. International Journal of Work Organisation and Emotion 3(4): 317-335.
- Tedeschi RG, Park CL, Calhoun LG (Eds.) (1998) Posttraumatic growth: Positive changes in the aftermath of crisis. Posttraumatic growth: conceptual issues. Erlbaum, Mahwa, NJ, pp. 1-22.
- Armstrong AR, Galligan RF, Critchley CR (2011) Emotional intelligence and psychological resilience to negative life events. Personality and Individual Differences 51(3): 331–336.
- Bailey GB (2021) The association of emotional intelligence and transformational leadership to job satisfaction of social work leaders. University of Maryland Baltimore.
- Follesdal H, Hagtvet K (2013). Does emotional intelligence as ability predict transformational leadership? A multilevel approach. The Leadership Quarterly 24(1).
- George JM (2000) Emotions and Leadership: The Role of Emotional Intelligence. Human Relations 53(1): 1027-1055.
- Harms PD, Crede M (2010) Emotional intelligence and transformational and transactional leadership: A meta-analysis. Journal of Leadership & Organizational Studies 17: 5-17.
- Lindebaum D, Cartwright S (2010) A critical examination of the relationship between emotional intelligence and transformational leadership. Journal of Management Studies, 47(7): 1317-1342.
- Tagoe T, Quarshie EN (2017) The relationship between emotional intelligence and job satisfaction among nurses in Accra. Nurs Open 4(2): 84-89.
-
Gary B Bailey*. Leading from Post Covid Stress Disorder Toward Post Covid Growth. Open Access J Addict & Psychol 7(2): 2023. OAJAP.MS.ID.000658.
Post Covid; Stress Disorder; Post Covid Growth; Covid-19; Emotional response; Behavioral; Mental health; Cognitive; Traumatized people; Trauma; Avoidance symptoms; Traumatic events; Brain fog; Deep distress; Rejuvenation; Negative reactions
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






