 Research Article
Research Article
Burnout Impact on Medical Students’ Performance in the Eastern Province, Saudi Arabia
Aziza A Alzubaidi1*, Abdullah A Al Shakhs2, Fatimah M Alshakhs2, Latifah A Alhashim2, Mohammed A Almuhanna2, Abdullah J Al Abbas3, Meral F Alzimam4, Yasir G Alrashdan4 and Ahmed A Alsaleh5
1Pediatric senior resident, Saudi program, Kingdom of Saudi Arabia
2King Faisal University, Kingdom of Saudi Arabia
3Imam Abdulrahman Bin Faisal University, Kingdom of Saudi Arabia
4Hail University, Kingdom of Saudi Arabia
5Majmaah University, Kingdom of Saudi Arabia
Aziza A Alzubaidi, Pediatric senior resident, Saudi program, Kingdom of Saudi Arabia.
Received Date: February 01, 2020; Published Date: February 11, 2020
Introduction
Burnout is a mental condition described as a prolonged response to chronic emotional and interpersonal stressors on the job [1]. It is characterized by emotional exhaustion, energy depletion, a feeling of personal inefficacy and cynicism. Many studies concluded that medical student have high level of burnout, ranging from 45% to 50% [1-4]. One huge study done in Saudi Arabia, have reported that burnout level was very high among medical students (76.8%) [5]. Other study done in Lebanon found that burnout was higher among students in pre- clinic years comparing to clinic years (71%) [6,7].
Medical students usually experience more stressors than students from other departments [8-13]. These stressors have many negative impacts on both comprehension of medical students and their cognitive functioning [14]. Medical education stressors might also associate with negative impacts on the physical and mental health of medical students [11-15]. Which might affect not only the personal health of medical students and doctors but may affect the quality of patients care too [16,17].
In Saudi Arabia, our curriculum still considers traditional. We didn’t have any noteworthy changes in our pre-clinical and clinical years teaching techniques [17-21]. However, many researchers have concluded that medical students experience more stress when entering clinical environs. They become more inclined to experience compassion fatigue and burnout [22-25].
Despite the extensive data on medical student burnout increasing prevalence, to our knowledge, no national study has evaluated the factors associated with stress, burn out and depression among medical students and its effects on their performance [26-28].
Methods
We carried a cross-sectional study with an online-based data questionnaire on medical students from King Faisal University and Imam Abdel Rahman bin Faisal in Saudi Arabia. 328 medical students were invited to participate in the study Participation was entirely voluntary, and responses were anonymized.
Ethical consideration
Confidentiality was assured to all participants who agreed to participate in the study. The respondents were given a brief description of the study and its objectives.
Data analysis
After data extracted, were revised, coded, and fed to statistical software, IBM SPSS version 22. All statistical analysis was performed using two-tailed tests and an alpha error of 0.05. A P-value less than or equal to 0.05, considered to be statistically significant. Composite mean was calculated for different burnout domains and overall mean then categorized into the mild level if the mean was less than 50%, moderate for a mean of 50% to < 75%, and severe for a mean of 75% up to 100%. Descriptive analysis based on frequency and percent distribution was done for all demographics and burnout data. The relation between burnout level and students’ personal data or their GPA was tested using the Pearson chi-square test.
Results
Table 1:Personal characteristics of medical students in Eastern region, Saudi Arabia.
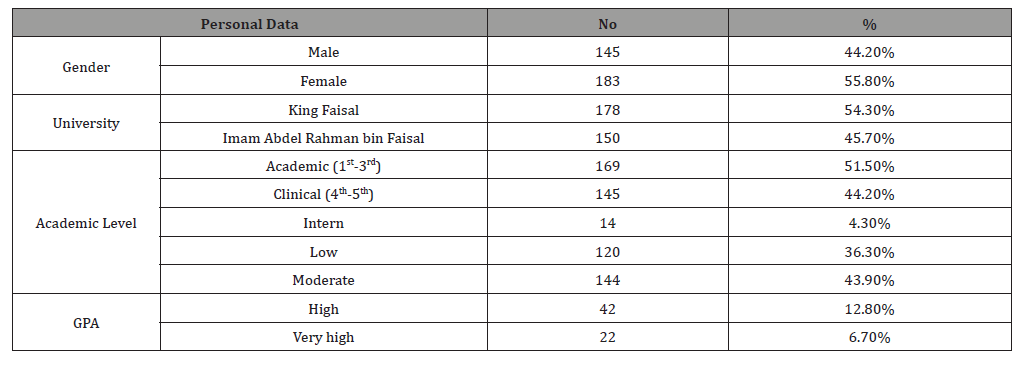
The study included 328 medical students, of which 55.8% were females and 54.3% from King Faisal University and 45.7% from Imam Abdel Rahman bin Faisal University. 51% of the students were at the preclinical stage (first to the third year), and 44.2% were at the clinical years, while 4.3% was an intern. Regarding GPA, 36.3% of the students had a low GPA, and 19.5% had either high or very high grades (Table 1).
Table 2 illustrates the frequency distribution of different burnout domains among the sampled students. Approximately onehalf (51%) of the students mostly feel Burn out, and 28.7% mostly feel the inability to take it anymore. As for work/study-related burnout, about one-half of the students (50.3%) had enough energy for family and friends during leisure time, and 37.2% feel that every working hour is tiring for them while only 8.8% feel worn out at the end of the working day. Considering colleagues related burnout, 64.9% of the participants wonder how long you will be able to continue working with colleagues, 64.1% tired in working with colleagues while 56.4% find it hard to work with colleagues. Considering teachers related burnout, 64.1% of the participants tired in working with teachers, 45.1% find it hard to work with teachers, and 47.9% wonder how long you will be able to continue working with teachers. Overall, 66.5% of the participants had mild personal burnout, while 2.7% had severe burnout. Additionally, 67% of the students had mild work/study-related burnout, and 3.7% had severe burnout. As for colleague related burnout, it was mild among 26.5% of the students and severe among 41.2% of the sample. About teachers’ related burnout, it was mild among 28% of the participants, while severe among 32.3% of them. Overall, 44.8% of the participants had mild burnout levels, and 7% had severe burnout (Figure 1).
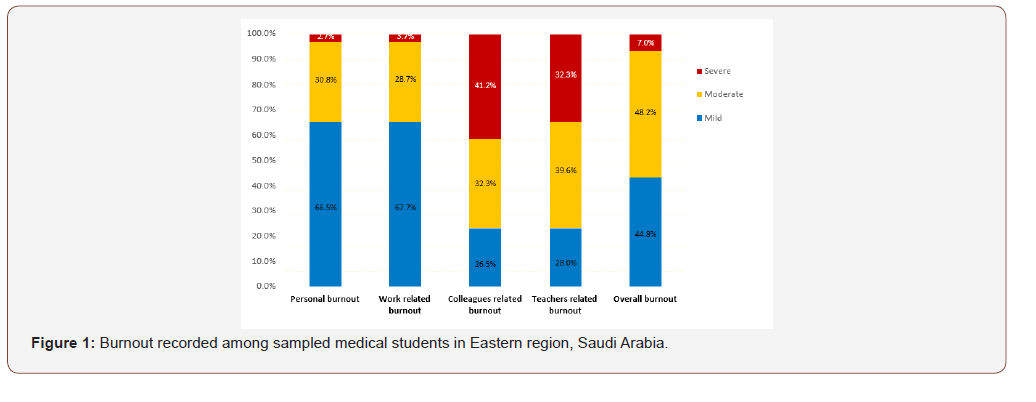
Table 2:Frequency distribution of different burnout domains among medical students in Eastern region, Saudi Arabia.
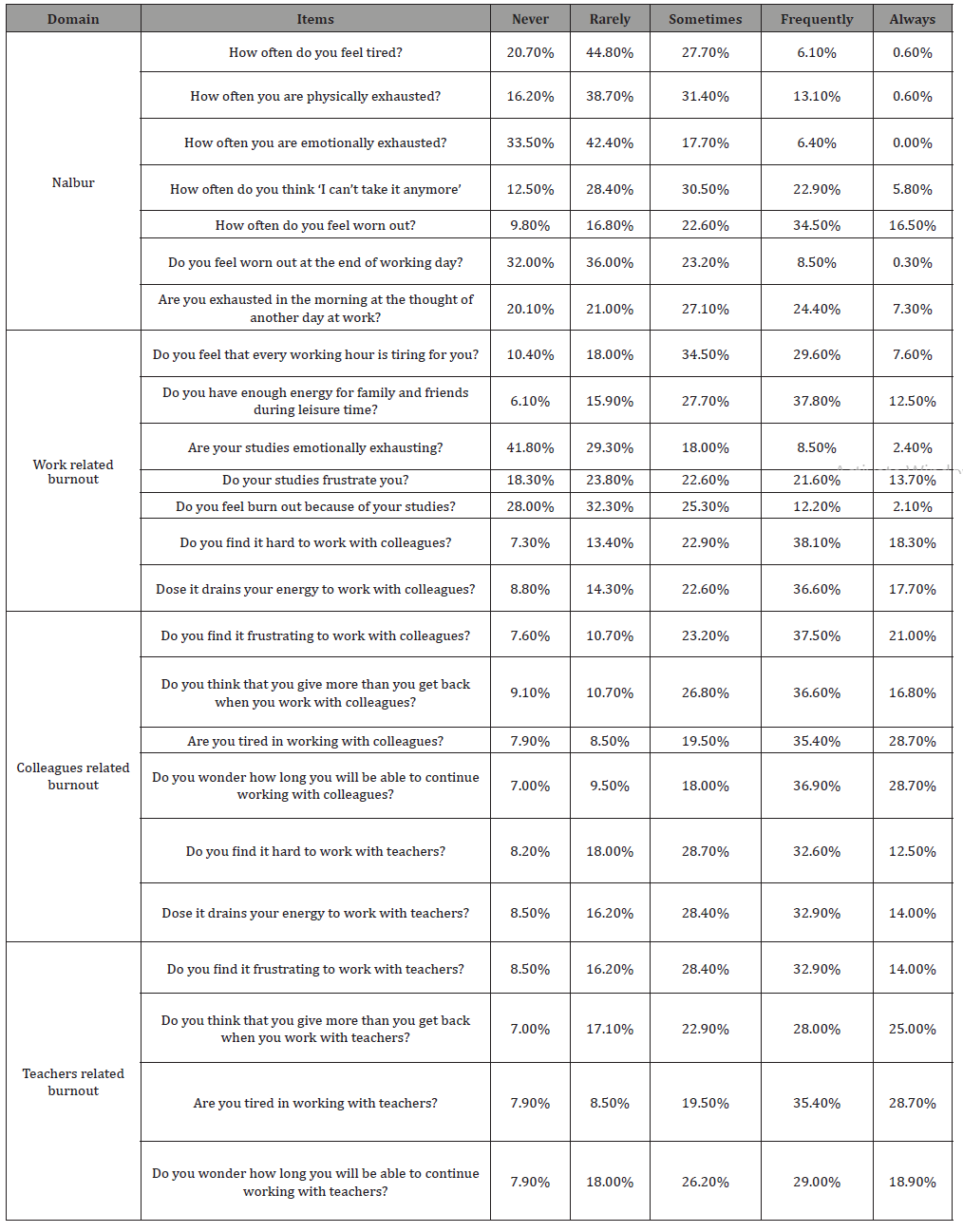
Table 3:Distribution of burnout level among sampled medical students according to their personal data.
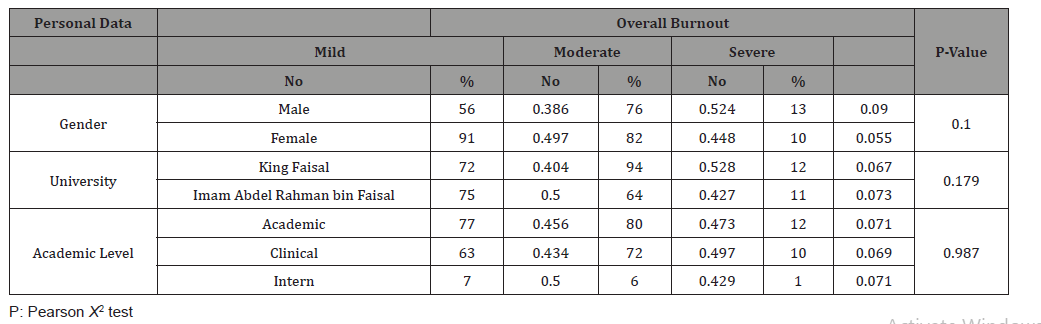
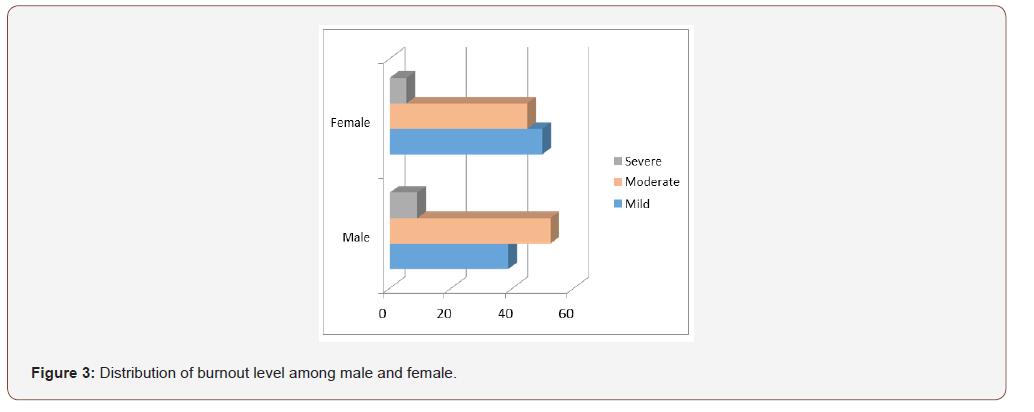
On relating burnout to participants’ personal data (Table 3), 9% of male students had severe burnout compared to 5.5% of females without recorded statistical significance (P=.100). As for the university, severe burnout was recorded among 6.7% of King Faisal University students compared to 7.3% of Imam Abdel Rahman bin Faisal University students (P=.179). Regarding academic year, 7.1% of preclinical students and interns had severe burnout compared to 6.9% for students in the clinical years (P=.987); however, the differences were not statistically significant (P> 0.05).
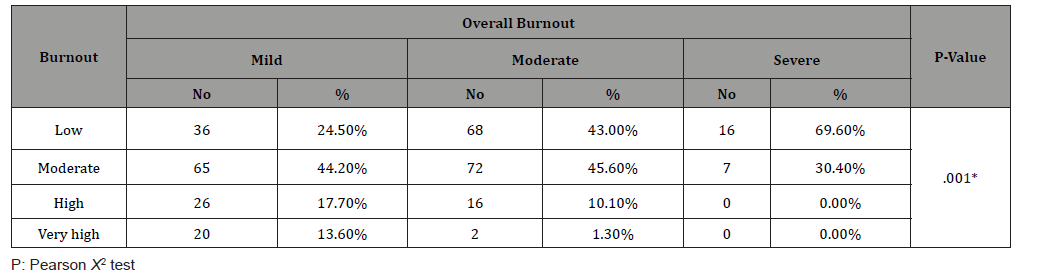
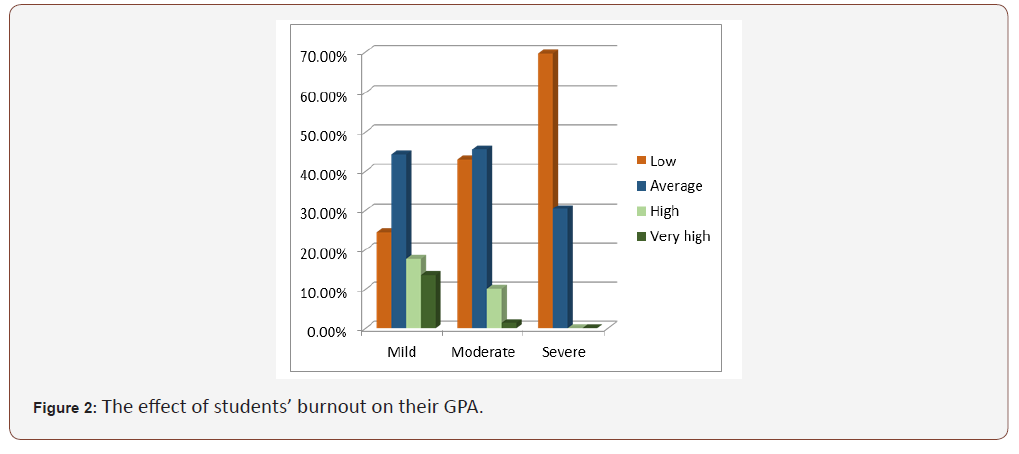
Finally, Table 4 shows the effect of students’ burnout on their GPA. Exact of 69.6% of students with severe burnout had a low GPA compared to 24.5% of those with mild burnout. Also, 30.4% of the students with severe burnout had a moderate GPA, while none of them recorded a high GPA compared to 44.2% and 31.3% of those with mild burnout, respectively. This association was found to be statistically significant (P=.001) (Figure 2).
Table 4:Relation between burnout level and students’ GPA among sampled medical students according to their personal data.
Discussion
The definition of burnout was introduced by Freudenberger in his psychosocial literature [29,30]. According to WHO, burnout is a syndrome linked to unresolved, long-term, work-related stress [31]. In 2019, the WHO concluded that burn our must be work related [31]. Based on the current classification by WHO (ICD-11), burnout might arise from unsuccessful management of chronic work-related stress, resulting in an occupational syndrome characterized such symptoms as “ cynicism associated with one’s job, feelings of negativism or feelings of energy depletion; and reduced professional efficacy” [32].
Many studies found that burnout is nosologically, etiologically and clinically like depression [33-36]. One study done by Bianchi et al. 2013 directly compared clinically depressed people and depressive symptoms in burned-out workers, no significant differences found in the diagnosis of both groups. clinically depressed people had similar depressive symptoms with burned out workers [37].
medical students’ mental health must always be under the focus as, besides their study-related affairs, responsibilities, and high burden are placed on these students because in medicine they are responsible for their community health care with the unacceptability of errors, favoring the development of anxiety and stress [38-40] (Figure 3).
The current study aimed to detect burnout among medical students in the eastern region of Saudi Arabia and assess its relationship with their educational achievement. Our results revealed that more than half of the students had moderate to severe burnout. The most recorded area of burnout was their deal with colleagues, as about 40% of the students had severe burnout in this area, followed by their relationship with teachers. This indicates that the main area of defect in medical students’ life is personal relations and how to overcome other disadvantages.
In Saudi Arabia, Almalki SA, et al. [41] did a cross-sectional study aimed to evaluate the influence of extracurricular activities on burnout and assess burnout level of medical students. They concluded that burnout levels of medical students at King Saud bin Abdulaziz University in Riyadh were very high. The authors suggested that medical curriculum must include leadership skills [41].
Regarding the determinants of burnout, none of the students’ characteristics were related to the degree of burnout. With regard to the effect of burnout on students’ educational achievement, there was a negative association between the degree of burnout and students’ GPA as none of the students with severe burnout had a high GPA while nearly half of those with mild burnout recorded either high or very high grades.
A study conducted by dos Santos Boni, 2018 [42], to determine the prevalence and the associated factors of burnout among medical students in the first years of undergraduate school. The study revealed that a total of 187 students (187/265, 70.6%) presented high levels of emotional exhaustion, 140 (52.8%) had high cynicism, and 129 (48.7%) had low academic efficacy. Another study conducted by Ebrahim et al. 2018 [43] to detect medical students’ occupational burnout and its relationship with professionalism. The researchers found that 54.3% of the students had low, 35.2% moderate, and 10.4% high job burnout, which is very similar to the current research findings. However, they also found that there was no significant relationship between the increase in academic years and burnout in contrast to our results.
In the present study, on relating burnout to participants’ personal data, 9% of male students had severe burnout compared to 5.5% of females without recorded statistical significance (P=.100).
Mutual proactive and reactive coping strategies between the medical students and the universities are encouraged to prevent and manage burnout among medical students. Various stress management interventions have been suggested to help improve students’ health and well-being in the workplace or study environment and lower stress levels. Training employees in ways to control stress in the workplace have also been suggested to be effective in preventing burnout [44-46].
Conclusion and Recommendations
The present study showed a moderately high prevalence of burnout among medical students, especially in their relationships with colleagues and teachers. Also, burnout recorded a major effect on their educational achievement, which was reflected in their GPA. Our study highlights the fact that burnout syndrome has a considerable effect, with great involvement mainly on achievement areas regardless of the academic year or gender. These findings established the need to develop preventive measures focused on the personal relations of the students, providing a better performance, motivation, and social skills in the subsequent stages of their life.
Acknowledgement
None.
Conflict of Interest
No conflict of Interest.
References
- Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol 52: 397-422.
- Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, et al. (2008) Burnout and suicidal ideation among U.S. medical students. Ann Intern Med 149(5): 334-341.
- Muzafar Y, Khan HH, Ashraf H, Hussain W, Sajid H, et al. (2015) Burnout and its associated factors in medical students of Lahore,Pakistan. Cureus 7(11): e390.
- Dahlin ME, Runeson B (2007) Burnout and psychiatric morbidity among medical students entering clinical training: a three-year prospective questionnaire and interview-based study. BMC Med Educ 7: 6.
- El-Masry R, Ghreiz SM, Helal RM, Audeh AM, Shams T (2013) Perceived stress and burnout among medical students during the clinical period of their education. Ibnosina J Med Biomed Sci 5(4): 179-187.
- Fares J, Saadeddin Z, Al Tabosh H, Aridi H, El Mouhayyar C, et al. (2016) Extracurricular activities associated with stress and burnout in preclinical medical students. J Epidemiol Glob Health 6(3): 177-185.
- Mazurkiewicz R, Korenstein D, Fallar R, Ripp J (2012) The prevalence and correlations of medical student burnout in the pre-clinical years: a cross- sectional study. Psychol Health Med 17(2): 188-195.
- Tarnowski M, Carlotto MS (2007) Burnout Syndrome in students of psychology. Temas em Psicologia Tarnowski M, Carlotto MS. Burnout Syndrome in students of psychology. Temas em Psicologia 15(2): 173-180.
- Carlotto MS, Camara SG (2008) Preditores da Síndrome de Burnout em estudantes universitá Pensamiento Psicologico 4(10): 101-109.
- Dahlin M, Joneborg N, Runeson Bo (2005) Stress and De-pression among Medical Students: A Cross Sectional Study. Med Educ 39(6): 594-604.
- Dyrbye LN, Thomas MR, Shanafelt TD (2005) Medical students distress: causes, consequences, and proposed solutions. Mayo Clin Proc 80(12): 1613-1622.
- Saipanish R (2003) Stress among medical students in a Thai medical school. Med Teach 25(5): 502-506.
- Sherina MS, Lekhraj R, Nadarajan K (2003) Prevalence of emotional disorder among medical students in a Malaysian university. Asia Pac Fam Med 2: 213-217.
- Zaid ZA, Chan SC, Ho JJ (2007) Emotional disorders among medical students in a Malaysian private medical school. Singapore Med J 48(10): 895-899.
- Aguiar SM, Vieira APGF, Vieira KMF, Nabrega JO, Aguiar SM (2009) Burnout syndrome and associated fac-tors among medical students: a cross- sectional study. Clinics (Sao Paulo) 58(1): 34-38.
- Dahlin ME, Runeson Bo (2007) Burnout and psychiatric morbidity among medical students entering clinical training: a threeyear prospective questionnaire and interview-based study. BMC Medical Education 7: 6.
- Willcock S, Daly MG, Tennant CC, Allard BJ (2004) Burn-out and psychiatric morbidity in new medical graduates. Med J Aust 181(7): 357-360.
- Amr M, El-Gilany A, El-Sayed M, El-Sheshtawy E (2007) study of stress among medical students at Mansoura university. Banha Medical Journal 37(5): 25-31.
- Abdelghanni HM (2008) Stress and depression among medical students: A cross sectional study at a medical college in Saudi Arabia. Pak J Med Sci 24(1): 12-17.
- El-Gilany AH, Amr M, Hammad S (2008) Perceived stress among male medical students in Egypt and Saudi Arabia: effect of sociodemographic factors. Ann Saudi Med 28: 442-448.
- FAIMER International Medical Education Directory (2006) [Internet]: Foundation for Advancement of International Medical Education and Research. IMED.
- Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, et al. (2006) Personal life events and medical student burnout: a multicenter study. Acad Med 81(4): 374-384.
- Dyrbye LN, Thomas MR, Huschka MM, Lawson KL, Novotny PJ, et al. (2006) A multicenter study of burnout, depression, and quality of life in minority and nonminority US medical students. Mayo Clin Proc 81(11): 1435-1442.
- Kearney MK, Weininger RB, Vachon MLS, Harri-son RL, Mount BM (2009) Self-care of physicians caring for patients at the end of life: “Being connected a key to my survival”. JAMA 301(11): 1155-1164.
- Balch CM, Shanafelt TD, Sloan JA, Satele DV, Freischlag JA (2011) Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg 254(4): 558-568.
- Maslach C, Jackson S, Leiter (1996) Maslach Burnout Inventory Manual. (3rd edn). Consulting Psychologists Press, CA, USA.
- Spickard A Jr, Gabbe SG, Christensen JF (2002) Mid-career burnout in generalist and specialist physicians. JAMA 288(12): 1447-1450.
- Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, et al. (2009) Burnout and career satisfaction among American surgeons. Ann Surg 250(3): 463-471.
- Freudenberger HJ (1974) Staff burn-out. Journal of Social Issues 30(159): 65.
- Maslach C (1976) Burned-out. Human Behavior 5(16): 22.
- (2019) Burn-out an occupational phenomenon: International Classification of Diseases. WHO Geneva, Switzerland.
- Renzo Bianchi, Irvin SamSchonfeld (2016) IS Burnout is associated with a depressive cognitive style. Personality and Individual Differences 100: 1-5.
- Ahola K, Hakanen J, Perhoniemi R, Mutanen P (2014) Relationship between burnout and depressive symptoms: A study using the person-centred approach. Burnout Research 1(1): 29-37.
- Bianchi R, Schonfeld IS, Laurent E (2014) Is burnout a depressive disorder? A re-examination with special focus on atypical depression. International Journal of Stress Management 21(4): 307-324.
- Bianchi R, Laurent E (2015) Emotional information processing in depression and burnout: An eye-tracking study. European Archives of Psychiatry and Clinical Neuroscience 265(1): 27-34.
- Bianchi E, Schonfeld IS, Laurent E (2018) Burnout syndrome and depression. In: YK Kim (Ed) Understanding depression: Clinical manifestations, diagnosis and treatment 2: 187-202.
- Bianchi R, Boffy C, Hingray C, Truchot D, Laurent E (2013) Comparative symptomatology of burnout and depression. J Health Psycho 18(6): 782-787.
- De Almeida GC, De Souza HR, De Almeida PC, De Almeida BC, Almeida GH (2016) The prevalence of burnout syndrome in medical students. Rev Psiquiatr Clin 43: 6-10.
- Dyrbye L, Shanafelt T (2016) A narrative review on burnout experienced by medical students and residents. Med Educ 50(1): 132-149.
- Shanafelt TD, Dyrbye LN, West CP, Sinsky CA (2016) Potential Impact of Burnout on the US Physician Workforce. Mayo Clin. Proc 91(11): 1667-1668.
- Almalki SA, Almojali AI, Alothman AS, Masuadi EM, Alaqeel MK (2017) Burnout and its association with extracurricular activities among medical students in Saudi Arabia Int J Med Educ 8: 144-150.
- Dos Santos Boni RA, Paiva CE, De Oliveira MA, Lucchetti G, et al. (2018) Burnout among medical students during the first years of undergraduate school: Prevalence and associated factors. PloS one 13(3): e0191746.
- Ebrahimi S, Atazadeh F (2018) Medical Students’ Occupational Burnout and its Relationship with Professionalism. J Adv Med Educ Prof 6(4): 162-167.
- Altannir Y, Alnajjar W, Ahmad SO, Altannir M, Yousuf F, et al. (2019) Assessment of burnout in medical undergraduate students in Riyadh, Saudi Arabia. BMC medical education 19(1): 34.
- AlSayari RA (2019) Using single item survey to study the prevalence of burnout among medical residents-influence of gender and seniority. Saudi Journal of Kidney Diseases and Transplantation 30(3): 581-586.
- William D, McLaurine A correlational study of job burnout and organizational commitment among correctional officers. Capella University. School of Psychology, USA, p. 92.
-
Aziza A A, Abdullah A A S, Fatimah M A, Latifah A A, Mohammed A A, et al. Burnout Impact on Medical Students’ Performance in the Eastern Province, Saudi Arabia. Open Access J Addict & Psychol. 3(3): 2020. OAJAP.MS.ID.000562.
Burnout, Cynicism, Lebanon, Medical, Cognitive functioning, Researchers, Fatigue, Anxiety, Stress, Demographic
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






