 Research Article
Research Article
Dementia Caregivers During Pandemic Covid-19
Dr. Tatomirescu Liviu Florian*
Francisc Rainer Institute of Medical Anthropology, Romania
Tatomirescu Liviu Florian, Francisc Rainer Institute of Medical Anthropology, Romania
Received Date: October 31, 2022; Published Date: December 01, 2022
Abstract
Globally, there are officially 50 million people who have dementia, and a new case occurs every 3 seconds, which makes dementia itself a pandemic in an aging society. The double blow, dementia, and the COVID-19 pandemic, raises concerns and problems for both people suffering from dementia and their careers.
The paper aims to analyze how forced social isolation has influenced the life and professional activity of dementia caregivers. Patients have difficulty understanding and remembering the public health information issued and the rules of protection. In turn, caregivers, either family members or care workers, were exposed to stress related to the fear of infection, but also to the condition of patients and developed an increased level of anxiety and signs of exhaustion. Because patients with dementia had anxiety, family members discontinued cognitive or physical therapies. The quality of care for the patient with dementia depends on the well-being of the caregiver. We measured the six Ryff factors, 1989 on a group of 15 caregivers (11- family members, 4- care workers). For them, the psychological well-being in relation to the care activity and the adaptation to the current environment are done with increased efforts in the COVID-19 pandemic.
Therefore, more than ever, the pandemic has indicated the need for collaboration between public health services, care workers and the family, to ensure the continuity of therapies for patients with dementia and the well-being of the caregiver.
Keywords: Dementia; Caregiver; Psychological Well-Being; COVID-19 Pandemic
Working Hypothesis
Globally, there are officially 50 million people who have dementia, and a new case appears every 3 seconds, which makes dementia, itself, a pandemic in an aging society. The double blow, dementia, and the COVID-19 pandemic raise concerns and problems for both people suffering from dementia and their caregivers. The paper aims to analyze how forced social isolation has influenced the life and professional activity of dementia caregivers. Patients have difficulty understanding and remembering the public health information issued and the rules of protection. In turn, caregivers, either family members or care workers, were exposed to stress related to the fear of infection, but also to the condition of patients, and developed a level of increased anxiety and signs of exhaustion. Because dementia patients experienced anxiety, family members discontinued cognitive or physical therapies. The well-being of the caregiver depends on the quality of care of the patient with dementia.
Psychological well-being refers to “the effort to achieve perfection, that is, to realize the true potential of the person” (Ryff & Keyes, 1995, p. 100). The success of the individual’s adaptation to the environment, expressed by the psychological well-being, is captured by six factors (Ryff, 1989): Self-acceptance refers to the presence of positive attitudes directed towards oneself; awareness and acceptance of multiple aspects relating to oneself, whether good or bad; positive feelings about one’s own past. Positive relationships with others refer to the presence of warm, satisfying and trusting relationships with others; concern about the well-being of others; being capable of empathy, affection, and strong intimacy; understanding the benefits and costs in human relationships. Autonomy refers to being self-determined and independent; being resistant to social pressures about one’s own beliefs and behaviors; behavioral regulation on one’s own initiative; evaluating the self in relation to personal standards.
Environmental control refers to having a sense of mastery and competence in managing the environment; controlling a wide range of external activities; valuing the opportunities around you; being able to choose and influence contexts that are favourable to one’s own needs and values. Meaning in life, or purpose in life, refers to having goals in life and a sense of a clear direction; to feel that there is meaning in the present and past life; the preservation of beliefs that give life a purpose; it has goals and purposes for which it lives. Personal development refers to having a sense of continuous development; it defines one’s self as being in a continuous development and expansion; it is open to new experiences; it has a sense of realizing one’s own potential; it perceives improvements over time in one’s own self and behaviors; it is adaptable in such a way as to reflect more effectiveness and self-knowledge; it has a sense of realizing one’s own potential; it perceives improvements over time in one’s own self and in one’s own behaviors; it is adaptable in such a way as to reflect more efficacy and self-knowledge; Throughout life, people face events, diverse life situations and challenges that they have to face and that develop their existence. The quarantine, isolation and restrictions measures imposed by the COVID-19 pan-demic represent an exceptional event in the life of caregivers, which has also affected healthy individuals and has determined perceptible and concrete changes, in terms of the well-being of caregivers of people with dementia.
Caregivers are facing many difficulties anyway, and outside of the pandemic. They carry an increased risk of burden, stress, depression, and a variety of other health complications. Numerous studies show that caring for a person with dementia is more stressful than caring for a person with physical disabilities. In addition to the specific challenges of caring for people with dementia, family careers face difficulties in meeting care with other requirements, including raising children, careers, and relationships.
Method Used
We measured the six factors Ryff, 1989 on a group of 15 caregivers (11- family members, 4- care workers). For them, psychological well-being in relation to the care activity and adaptation to the current environment are being made with increased efforts in the COVID-19 pandemic. The testing was done in April 2021, about a year and a month after the onset of restrictions in Romania.
The testing was done individually, by applying the questionnaires by pencil-paper method. The environment in which the questionnaires were filled in was an appropriate one (without disruptive factors). The subjects voluntarily participated in this research. Verbally, there was a specific training, communicated to the volunteers. The training was the same for all subjects, being done at the beginning, asking questions from the subjects so as to ensure that the task was understood. The subjects were told the purpose of the research. The anonymity and confidentiality of the data were guaranteed to the participants, according to the deontological norms specific to the Romanian legislation.
The only conditions for participation in the study were for the volunteer to be the caretaker of a person with dementia and to live (and care for a person) in Romania. The patients cared for by the participants have various forms of dementia, Alzheimer’s dementia (AD), Lewy body dementia (DLB), frontotemporal dementia (FTD) and vascular dementia (VD), mixed dementia. Data on the sex of the participants, rural/urban areas, the type of care – paid – in the centers or at the patient’s/no home, the age of the patient and the form of dementia were also collected. The scale of Ryff’s psychological well-being (PWB-R) was developed by Ryff in 1989 and measures the degree of the individual’s psychological wellbeing. It contains 42 items, with responses from 1 to 6, where 1 is “strong disagreement” and 6 “strong agreement”.
The items are divided into 6 subscales: autonomy (e.g. item: “I trust my opinions even if they are contrary to the general opinion.”), control over the environment (e.g. item: “I managed to build a home and a lifestyle that is largely to my liking.”), personal development (e.g. item: “I think it is important to live new experiences that pose a challenge to the way you think about the world.”), positive relationships with others (e.g. item: “I like personal and shared conversations with family members or friends.”), purpose in life (e.g. item: “I like to make plans for the future and turn them into reality”) and self-acceptance (e.g. item: “The past had ups and downs, but in general I would not want to change it.”). High elevations represent a high level of aspects of psychological well-being. For the calculation of the score, the average is calculated for the items of each subscale, the maximum average score is 6, the minimum average score is 1.
Research Results
The 15 volunteers recorded the following total scores, average scores, with the following lower and higher values:
a) Autonomy: total score 12, minimum value 7, maximum value 12, average score 1, 71,
b) Environmental control: total score 17, minimum value 10, maximum value 12, average score 2.42.
c) Personal development: total score 11, minimum value 7, maximum value 11, average score 1.57.
d) Positive relations with others: total score 19, minimum value 15, maximum value 20, average score 2.71.
e) Goal in life: total score 22, minimum value 20, maximum value 25, average score 3.14.
f) Self-acceptance: total score 27, minimum value 25, maximum value 30, average score 3.8 6 (Figure 1).

Interpretation of Results
The low values of the Autonomy indicator mean that the caregiver is concerned about the expectations and evaluations of others; it relies on the judgments of others to make important decisions; it conforms to social pressures to think and act in certain ways. Such an attitude can be attributed to the fact that he feels alone in front of the problems caused by dementia, he shows a fear of being commented on by the people around the patient, by the decision she will take regarding the patient.
The low values of the Environmental Control indicator mean that the career has difficulty managing his day-to-day affairs; he feels unable to change or improve the surrounding context; he is not aware of the opportunities around him; he does not have a sense of control over the external world. Such an attitude can be attributed to the fact that he finds himself restricted in his current activity, sometimes reaching to give up even his professional activity to devote himself to the care of the patient.
The low values of the Personal Development indicator mean that the caregiver has a feeling of personal stagnation; lacks a feeling of improvement or expansion over time; feels bored and uninterested in life; feels unable to develop new attitudes or behaviors. Such an attitude can be attributed to the frustration caused despite the fact that he cares for and dedicated himself to the patient, but he does not see positive changes in the evolution of the disease, but he does not see a burden that is difficult to carry especially to the family caregivers (wife, wife, son, daughter).
The relatively low values of the positive relationships with others indicator mean that the career has few close and trusting relationships with others; he finds it difficult to be warm, open, and concerned about others; he is isolated and frustrated in human relationships; he is not willing to compromise to sustain important connections with others. Such an attitude can be attributed to the fear of making mistakes, of being scolded by others, he considered himself responsible and guilty of everything that can happen to the patient. The relatively average values of the Purpose in Life indicator mean that the caregiver has few goals or targets; he does not see the purpose of the past life; he does not have perspectives or beliefs that give meaning to life, he focuses on caring for the patient and keeping his role as caregiver in balance with his other roles, gaining a purpose dedicated to the one he cares for. The average values of the Self-acceptance indicator signify that the caregiver feels at peace with his role, is relatively fulfilled in his work, if in the first phase he suffers, then he feels delighted with what he is doing.
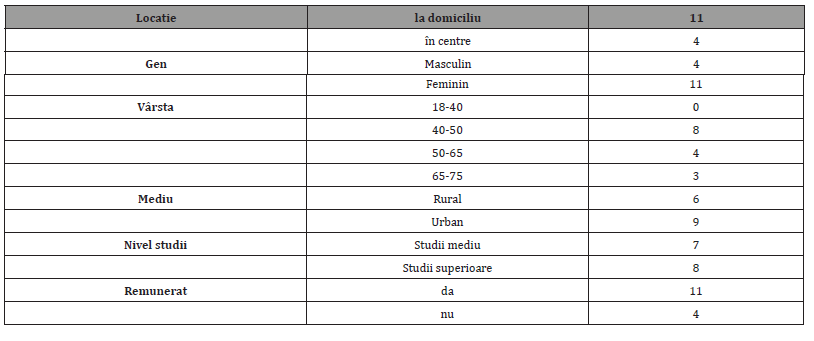
The demographic characteristics of the participants are represented in Table 1. Out of 15 caregivers, it stands out that 11 are women and 4 are men. Out of 4 men, 3 are home careers and 1 care center worker; out of 11 women, 8 are careers at home and 3 are workers in care homes. There is a tendency for family caregivers, informal caregivers, to become formal caregivers, by hiring as a personal assistant to the patient with dementia, in this case, 2/3 of the family caregivers being personal assistants. Also, out of 15 caregivers, 6 live and work in rural areas and 9 in urban areas, 7 have secondary education and 9 have higher education. As for the age of the patients cared for, 10 of them are over 75 years old and 5 under 75 years old. As for the age of caregivers, the average age is around the age of 50 (Table 1).
Table 1: Demographic characteristics of participants.
Although the sample tested is low, the breakdown by sex confirms the finding that it is women who traditionally assume and perform the role of caregivers of patients in the family. It is noted that families in rural areas prefer home care of patients in the family, compared to families in urban areas, who resort to hospitalization in care centers / elderly centers since the middle stages of dementia. Rural families generally later resort to hospitalization of family members diagnosed with dementia as the disease progresses and caregivers are increasingly exhausted. The costs of care in dedicated centers can be prohibitive for some families, especially those in rural areas, where household incomes are lower than those in urban areas. Also, traditionally, families in rural areas prefer home care, placing the elderly in centers being blamed in small communities.
It is noted that paid caregivers develop less anxiety, depression, insomnia than unpaid ones, who are usually the spouse or children of the person being cared for. Against the background of physical exhaustion, family caregivers develop insomnia, because the patient does not sleep. There is a reversal of the sleep-wake rhythm, an accentuation of the state of fatigue, increased worry, up to the stage of anxiety. In the moment of anxiety, the solution is to formalize care, either by being admitted to caring homes or by dedicating the patient’s caregiver and hiring a personal assistant. After the moment of accepting the situation, the family caregiver acquires resilience, anxiety and depression are relieved.
Study Limits and Future Research Suggestions
The limits of the study are related to the low number of participants, the willingness of the caregivers to answer the questions asked, in the context in which their time is limited, and, as far as the caregivers in the family are concerned, their time is largely seized by the caregivers, the state of physical and mental exhaustion in which they find themselves. The suggestions for future studies are related to the use of open tools, such as structured interview, narrative interview, which complement the method used and also fulfill a therapeutic role, allowing caregivers to communicate their fears and worries, positive communication with other people, cover the need to be listened to by medical staff.
Conclusion
The purpose of this study was to examine the concerns of caregivers of patients with various forms of dementia during the COVID 19 pandemic. Data collected from the RYFF scale shows us that caregivers have taken on additional duties to care for patients as well as their families, have reported concerns about the spread of covid 19 and finally symptoms of anxiety. Also, those with anxiety reported less functional independence compared to those who did not report anxiety. Health professionals should be mindful of the concerns expressed by dementia caregivers for their well-being during this pandemic. Family caregivers of people with dementia have been particularly concerned about the absence of paid caregivers during the pandemic.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Brodaty H, Marika Donkin (2009) Family caregivers of people with dementia. Dialogues Clin Neurosci 11(2): 217-28.
- Edelman P, D Kuhn, B R Fulton (2004) Influence of cognitive impairment, functional impairment, and care setting on dementia care mapping results. Aging Ment Health 8(6): 514-23.
- Kállay E, Rus C (2014) Psychometric properties of the 44-item version of Ryff’s psychological well-being scale. European Journal of Psychological Assessment 30(1): 15-21.
- Ryff CD (1989) Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology 57(6): 1069-1081.
- Ryff CD, Dienberg Love G, Urry HL, Muller D, Rosenkranz MA, et al. (2006) Psychological well-being and ill-being: Do they have distinct or mirrored biological correlates? Psychotherapy and Psychosomatics 75(2): 85-95.
- Scholzel Dorenbos CJ, Teake P Ettema, Joke Bos, Ellen Boelens van der Knoop, Debby L Gerritsen, et al. (2007) Evaluating the outcome of interventions on quality of life in dementia: selections of the appropriate scale. Int J Geriatr Psychiatry 22(6): 511-519.
- Sloane PD, Dawn Brooker, Lauren Cohen, Carolinda Douglass, Perry Edelman, et all. (2007) Dementia care mapping as a research tool. Int J Geriatr Psychiatry 22(6): 580-589.
- Woods RT (1989) Alzheimer’s Disease: Coping with a Living Death. Souvenir, London.
-
Dr. Tatomirescu Liviu Florian*. Dementia Caregivers During Pandemic Covid-19. Open Access J Arch & Anthropol. 3(5): 2022. OAJAA.MS.ID.000573.
-
Physical disabilities, Lewy body dementia, Physical exhaustion
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






