 Review Article
Review Article
Eight Physiological Benefits of Regular Exercise for Diabetic Patients
Keith Chittenden*
DPM, DPT, MS, ACSM-EP, CSCSD, Resident Physician, Department of Podiatric Medicine, St. Barnabas Hospital, Bronx, NY, USA.
Keith Chittenden, DPM, DPT, MS, ACSM-EP, CSCSD, Resident Physician, Department of Podiatric Medicine, St. Barnabas Hospital, Bronx, NY, USA
Received Date:January 22, 2024; Published Date:February 07, 2024
Abstract
Summary of 8 major physiological complications from diabetes. Each complication is discussed and the benefits from exercise that a patient with diabetes can get as a result in engaging in regular exercise is discussed for each one of the 8 complications. The eight areas of benefits from exercise are controllable heart rate and blood pressure, stabilized blood sugar, better healing of venous statis wounds, improved flexibility, Improved balance/proprioception, improved mental health, improved skin health, and decrease in body mass index.
Introduction
There are many articles written on modalities for treating a diabetic patient. Modalities in the form of drug therapy (i.e., Insulin such as glargine for type 1 diabetes and metformin for type 2 diabetes), podiatric medical checkups, compression stockings (for those patients with lower extremity edema), orthotics and special shoe wear are all popular nonsurgical treatment options for patients with both type 1 and type 2 diabetes. Out of all these mentioned modalities, which are not without criticism from other medical and health professionals due to its physiological side effects, there is one modality that has had positive benefits and almost zero risks or complications unlike others. That modality is exercise. Exercise is one of the most cost effective (no equipment needed or out of pocket expenses), easily implemented modality that any diabetic patient can do and maintain without any side effects. Exercise has been studied in peer reviewed journals for over 70 years and has yet to be seen in any article that points out any negative results towards patients with stable chronic diseases (with the exception of a patient recovering from foot or ankle surgery). Exercise is a modality that needs to be implemented more by diabetic patients not only for their health, but to maintain vascular, musculoskeletal and neurological function. Regular exercise helps to keep toes and portion of the diabetic foot intact, minimize ulcerations from forming, promotes vascular health, and reduce incidents of toe and foot amputations.
It should be the responsibility of the medical provider (MD, DO, DPM) to educate and insistently encourage their diabetic patients to start exercise regimes and maintain them regularly. It is also important to know about what type of exercises will be most beneficial to their patients and then encourage them to engage in the exercise throughout the patient’s quarterly or yearly check-ups. The physician should ask their patient how their exercise regime is going. If a patient does not know how to exercise or needs instruction, the physician or health care provider should refer that patient to an exercise physiologist, fitness trainer, or a physical therapist that is specifically trained in supervising exercise programs and execution of correct form of these exercise programs. The American College of Sports Medicine has had a program for years called exercise is medicine which educates both patients and medical providers the benefits of regular exercise. Patients with both type 1 and type 2 diabetes are the main patients that can benefit the most from regular exercise regimes. The American College of Sports Medicine and American Diabetes Association recommend that patients with both type 1 and type 2 diabetes participate in at least 150 minutes of moderate intensity exercise weekly with resistance training two or three times weekly [1]. Here are 8 benefits of regular exercise for a diabetic patient.
a) Reduced and controlled vitals. Most vital measurements that medical and allied healthcare providers focus on to give a summary of a patient’s health are heart rate (HR), blood pressure (BP), O2 saturation, these markers indicate how a diabetic patient is doing as far as their health is. Exercise has been proven to lower cholesterol, decrease resting heart rate, and decrease blood glucose levels indefinitely if regular fitness levels are also sustained over months of duration. Studies have shown that regular aerobic and resistive exercise can change the morphological state (i.e. weight) of the body, reducing the effort of the pumping heart to work hard to overcome resistance in the arteries that is encountered when a diabetic patient has hypertension. Hypertension can increase resting heart rate and blood pressure [2]. Exercise can decrease both of these vitals. Research has suggested that the mechanism of improvement comes from the increased effectiveness of the autonomic nervous system to stimulate an improvement of the circulation system through increased output from the cardiovascular system and increased stroke volume of left ventricle function. The duration of exercise also improves aerobic capacity of cardiovascular muscles or type 1 aerobic muscular fibers designed for muscular endurance for prolonged work which is measured as VO2 max. The strength of type 1 muscular or endurance type of muscles decreases the heart rate and effort force of contractile muscular tissue of both the heart and endocardium muscular of arteries. This decreases blood pressure and heart rate.
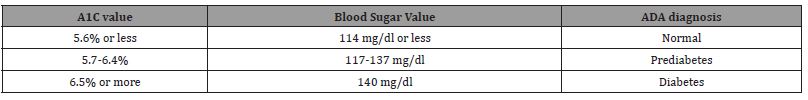
b) Stabilized Blood Sugar. Blood sugars are measured in 2 ways; fasting blood sugars which can be measured daily by monitoring blood glucose levels with a monitor. The normal blood sugar levels should be in the range of 70-100 mg/dl. If blood sugar is elevated (i.e. 120+ mg/dl) then blood sugars are not being managed correctly. The other method is during a blood test when the patient goes for their checkups with their primary care physician. This blood test is called the HBA1C test. This test is a blood test that measures a person’s average blood glucose levels over the average amount of time which is usually approximately 3 months. This blood test can be done with any blood test such a CBC which looks at other blood levels such as hemoglobin (HB). The glycated hemoglobin A1C (HBA1C) test shows the average percentage of blood sugar-binding to a hemoglobin in a blood sample. When blood sugar is measured the blood sugar will attach to a hemoglobin molecule and will allow the tester to know how high a diabetic patient’s blood sugar is at a given point of time. This test will determine if blood sugar is at safe and manageable levels. The normal/safe blood sugar should fall in the range of 5.6-6.5% of glycosylated hemoglobin. If the HbA1C is over 6.5% during a patient’s checkup, then this indicates the patient’s blood sugars are not under control and will need intervention. In medicine the traditional intervention is usually a pharmaceutical such as using insulin (i.e. glargine) for type 1 diabetes or metformin for type 2 diabetes [3]. Here are A1C values according to the American Diabetes Association (Table 1). When a diabetic patient engages in regular aerobic exercise (i.e. 2-3 times a week for over an hour), the body’s uptake in glucose almost doubles. As the heart rate increases, the demands for oxygen, glucose and blood flow also increases. As a diabetic patient increases their exercise tolerance steadily, the glucose uptake demand of the organs of the heart, liver, lungs and peripheral blood vessels will also increase their demand for glucose. This will reduce the blood sugar level and increase demand for insulin to be secreted for the demands of glucose to be transported into the organs of the cardiorespiratory system. The oxidation of carbohydrates and fatty acids in a person that exercises on a higher frequency vs. a person that seldomly or not at all exercises is almost double. The more oxidation of carbohydrates and fatty acids is done at rest (within a person that exercises) the lower their resting blood sugar will be. This will keep the diabetic patient’s daily/ weekly blood sugar under control and will maintain their A1C at normal levels (i.e., 5.7 and lower) [4].
Table 1:
c) Exercise has been proven to aid in the healing of diabetic and venous statis wounds. One of the contributory mechanisms in the lower extremity for increasing blood flow and draining of venous blood is the activity of the gastrocnemius muscle pumping function. Exercise can aid in decreasing pooling of venous blood in the lower extremity of diabetic and venous statis wounds. In pooling of edema and venous blood, the calf muscle pump ineffectively pumps blood from the legs to the heart due to venous insufficiency and obstruction One of the benefits of exercise is the increase of blood flow throughout the body and specifically to the areas of exercise (i.e., foot/ankle regions). With an increase of blood flow, there will be more optimization for healing of wounds. Exercises that target lower extremity function such as squats, cycling, calf raises [5]. These exercises can help facilitate more optimal blood flow in the lower extremity. Exercise also improves endothelial function of the blood vessels. With improved endothelial function, cardiovascular risks are minimized which helps decrease chronic venous insufficiency. One point that is important to note with this intervention is the high importance of patient adherence/compliance to carrying out this self-directed exercising. It goes without saying that high adherence and compliance must be present for this intervention to work. The studies have shown that those participants who adhere to an exercise program as an adjunctive treatment in combination with standard care are more likely to heal and have better functional outcomes than those who do not adhere to the exercises in conjunction with standard care (standard care generally comprises of compression dressings and elevation for venous statis wounds).
d) Improved Flexibility. Diabetic patients often are found in a position known as equinus. Equinus means the foot is pointed downward or plantarflexed. In an equinus deformity, the ankle joint measures <5 degrees in dorsiflexion or can’t reach neutral in which the foot can be taken out of plantarflexion. The patient will complain the ankle is stiff and doesn’t move out of that position. When the foot is in equinus, the plantar surface of the foot is subject to break down and an increase of pressure throughout the surface of the plantar foot occurs. These areas of increased pressure can result in ulceration and or buildup of hyperkerotic skin around the area most common as the “met-heads”. The toe bones are also known as the metatarsal bones. The met heads is the portion of the metatarsal bone that meets the phalanges, which as considered the tips of the toes which are both proximal and distal the toenail. The plantar surface around this area is a common place for skin break down, ulcerations and callous formations. When the foot is in a plantarflexed position, the bones of the metatarsals, specifically the metatarsal heads will be positioned planarly which could in turn cause ulcerations and result in non-healing wounds on plantar surface of the forefoot. Routine stretching done at least 2 times a day can help prevent the metatarsal bones and ankle joint from being adaptively positioned in these compromised positions [6].
e) Prevention of falls for diabetic patients. Diabetic neuropathy is a one of the most common complications from both type 1 and type 2 diabetes. Disorders coming from damage from the peripheral nerves of the feet include loss of protective sensation from mechanoreceptors found in the epidermis of the skin and disruption of proprioception from the feet and ankles. Proprioception is the ability to judge movement and the position of the body in space. When a person loses their proprioception, falls can be a direct consequence. Validation of this relationship is illustrated in studies using balance based functional tests such as the Timed up and go (TUG) and the Berg Balance test. Diabetic patients with a history of diabetic neuropathy have a high TUG score as their neuropathy will negatively affect their gate speed. A normal TUG score of 10 seconds or less is considered normal. According to research, Diabetic patients with neuropathy are scoring higher TUG scores which would be indictive of higher fall risks. Exercises such as resistance training, cardio, and non-impact activities such as swimming have been shown to improve balance, lower extremity strength, increased range of motion in the ankle joint as well as increase sensitivity within the receptors or epidermis and joint receptors which contribute to proprioception [7].
f) Improved skin health. Regular exercise has already been sited to improve vascular components including increased blood flow to the areas of the foot, specifically dorsally. With an increase of blood flow to the peripheral blood vessels and capillaries of the skin, other components within the blood flow have been shown to improve skin health. Nitric oxide is a vasodilator that improves the volume of blood flow by keeping the small blood vessels and capillaries open to allow the blood flow to be uninterrupted. Other components within blood flow include prostaglandins (PG), and endothelialderived hyperpolarizing factor (EDHF) are delivered to the skin of the dorsal and plantar foot. If blood flow is normal and non interrupted, these components can keep the skin soft, non-hyperkerotic, supple, and moveable. Regular exercise has been shown to promote collagen growth in the skin. Collagen is an important component as it will improve skin turgor. This will help keep the skin movable and decrease the incidence of callous formation. Callous formation can promote eventual formation of ulcerations plantarly or on other surfaces of the foot [8].
g) Promotes Mental Health. Research has shown exercise has improved mental status by decreasing rates of manic depression, bi-polar like disposition, anxiety in diabetic patient’s personalities. Exercise has been shown as the catalysts for the brain to secrete endorphins which contribute to stable mental health and feeling of focus and de-stressing your body. Exercise has also been documented to decrease depression and anxiety via increase neurotransmitters activation and increased serotonin and dopamine circulatory levels [9].
h) Decrease in Body Mass index. In many cases, diabetes and obesity are a common cofactor of each other, especially in the case of type 2 diabetes. One of the key pathophysiological factors that contributes to obesity in diabetic patients is the state of Insulin resistance (hyperinsulinemia or hyperglycemia). In this state there is both peripheral and central insulin resistance which may contribute to the development of abnormal autonomic cardiovascular control in diabetes [10]. The decrease of sensitization of skeletal muscle sensory neurons by insulin or glucose as well as impairment of insulin transport to the central nervous system including decreasing the activity of the insulin signaling pathway in the brain, is also a major contributing factor to how obesity can exacerbate diabetic patients’ symptoms. Another mechanism of exercise is the significant reduction in visceral fat accumulation. During .obesity, visceral fat accumulation is very prevalent throughout the mid-section of the body. These deposits of highly concentrated triglycerides statically accumulate on the body and contributes to the exacerbation of type 2 diabetes. Exercise training has been cited to show significant improvements in lowering fat deposits on the body and a reduction of diabetic related exacerbations including the proper control of blood sugars. This is accomplished by increasing lean body mass replacing the fat mass of the body as a result of growth of the diameter of muscle fibers in the body. This theory falls under the space occupying theory. One form of tissue that is heavier and denser will replace another type of tissue that is lighter, fluffier and more space filling [11].
Conclusion
Diabetes can cause many negative physiological impacts to a patients’ well-being. The complications summarized in this article are some of the most common complications as a result of diabetes. Diabetes can be managed medically through pharmalogical interventions, surgery, orthotics, bracing, proper diet, proper hydration. Exercise therapy has been a modality that has been proven over the decades to be an effective and low risk to the diabetic patient. Exercise is an evidence based viable intervention for the control of physiological response to diabetes. According to the American College of Sports Medicine recommendations of physical activity for people with both type 1 and type 2 diabetes [12].
a) Regular aerobic exercise training improves glycemic management in adults with type 2 diabetes, with less daily time in hyperglycemia and 0.5%-0.7% reductions in overall glycemia (as measured by A1C)
b) High-intensity resistance exercise training has greater beneficial effects than low-to-moderate-intensity resistance training in terms of overall glucose management and attenuation of insulin levels.
c) Greater energy expenditure postprandially reduces glucose levels regardless of exercise intensity or type, and durations ≥45 min provide the most consistent benefits.
d) Small “doses” of Physical activity throughout the day to break up sitting modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index.
e) Weight loss can be accomplished through lifestyle changes, proper diet and Physical activity of >5% of waking time in a patient’s day to day activities seems to be necessary for beneficial effects on A1C, blood lipids, and blood pressure.
References
- Dugan JA (2016) Exercise recommendations for patients with type 2 diabetes. JAAPA (1): 13-18.
- (2019) Reduce your A1C levels: Lifestyle, diet, and nutrition.
- Wellens Rita I, A F Roche, H J Khamis, A S Jackson, M L Pollock, et al. (1996) Relationships between the body mass index and body composition. Obes Res 4 (1): 35-44.
- Sickel Amy E, Jason D Seacat, Nina A (2014) Nabors Mental health stigma update: A review of consequences. Advances in Mental Health 12(3): 202-215.
- Crane Justin D, Lauren G MacNeil, James S Lally, Rebecca J Ford, Adam L Bujak, et al. (2015) Exercise‐stimulated interleukin‐15 is controlled by AMPK and regulates skin metabolism and aging. Aging cell 14 (4): 625-634.
- Bird Marie-Louise, Keith Hill, Madeleine Ball, Andrew D Williams (2009) Effects of resistance-and flexibility-exercise interventions on balance and related measures in older adults. J Aging Phys Act 17(4): 444-454.
- Lepesis, Vasileios, Jonathan Marsden, Joanne Paton, Alec Rickard, Jos M Latour (2022) Experiences of foot and ankle mobilisations combined with home stretches in people with diabetes: a qualitative study embedded in a proof-of-concept randomised controlled trial. J Foot Ankle Res 15(1): 7.
- Lee, Hyun Suk, Junga Lee (2021) Effects of exercise interventions on weight, body mass index, lean body mass and accumulated visceral fat in overweight and obese individuals: A systematic review and meta-analysis of randomized controlled trials. Int J Environ Res Public Health 18(5): 2635.
- Picard Mathilde, Igor Tauveron, Salwan Magdasy, Thomas Benichou, Reza Bagheri, et al. (2021) Effect of exercise training on heart rate variability in type 2 diabetes mellitus patients: A systematic review and meta-analysis. PLoS One 16(5): e0251863.
- O Brien Jane, Kathleen Finlayson, Graham Kerr, Helen Edwards (2017) Evaluating the effectiveness of a self‐management exercise intervention on wound healing, functional ability and health‐related quality of life outcomes in adults with venous leg ulcers: a randomised controlled trial. Int Wound J 14(1): 130-137.
- Kear BM, Guck TP, McGaha AL (2017) Timed Up and Go (TUG) Test: Normative Reference Values for Ages 20 to 59 Years and Relationships with Physical and Mental Health Risk Factors. J Prim Care Community Health 8(1): 9-13.
- Kanaley Jill A, Colberg Sheri R, Corcoran Matthew H, Malin Steven K, Rodriguez Nancy R, et al. Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement from the American College of Sports Medicine. Med Sci Sports Exerc 54(2): 353-368.
-
Keith Chittenden*. Eight Physiological Benefits of Regular Exercise for Diabetic Patients. Iris On Journ of Sci. 1(2): 2024. IOJS. MS.ID.000506.
-
Medium, phenomenology of truth, objective epistemology, language, consciousness, pure I
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






