 Research Article
Research Article
Non-Motor Symptoms among Patients with Parkinson’s Disease: The Prevalence and its Effect on Quality of Life
Lamiaa Hassnin Eita*
1Department of Nursing Science, Faculty of Health Sciences, University of Eastern Finland, Kuopio, Finland
Lamiaa Hassnin Eita, Assistant Professor of Psychiatric and Mental Health Nursing, Faculty of Nursing, Menoufia University, Egypt.
Received Date: January 10, 2020; Published Date: January 28, 2020
Abstract
Though traditionally Parkinson’s disease has been considered as a motor disorder, common and disabling non motor symptoms have an increasingly important role in Parkinson’s disease. The non-motor symptoms (NMSs) of Parkinson’s disease are a hallmark cause of disability and associated with the deterioration of life quality.
Aim: The aim of the study was to assess prevalence of NMSs among patients with Parkinson’s disease and its effect on quality of life QOL.
Methods: A quantitative descriptive correlational research design was used. A sample of 96 patients with PD was recruited from psychiatric outpatients’ clinics at Menoufia University Hospital. The Non-motor symptoms questionnaire (NMSs Quest) to detect the presence or absence of symptoms based on yes-no answers and EQ-5D visual analogue scale (EQ-5DVAS) to assess health-related quality of life.
Results: all patients with PD were complaining from one or more of non-motor symptoms and there were negative significant correlations between QOL total score and grand total scores of NMSs as well as its nine domains.
Conclusion: the present study showed that the non-motor symptoms had an effect on the quality of life. Recommendation: More assessment and management of NMSs are recommended for improvement of the quality of life of patients with PD and the involvement of a PD nurse specialist (PDNS) to offer education to the patients with PD and their families, the wider community, and training of clinical and non-clinical staff.
Keywords: Parkinson’s disease; Non-Motor symptoms (NMSs); Quality of life
Introduction
Parkinson’s disease is one of the common neurodegenerative movement disorders after Alzheimer disease. The cardinal manifestations of Parkinson disease are rest tremors, rigidity, bradykinesia and postural instability were described by Jamen Parkinson in 1817. He also described certain non- motor manifestations such as sialorrhea, urinary incontinence, sleep disturbances, feeling light-headed and falling, unpleasant sensations in leg and constipation. It was classified into nine domains which are; urinary, cardiovascular, gastrointestinal, sexual, cognition (apathy/attention/memory), hallucinations/delusions, anxiety/ depression, and sleep and miscellaneous [1]. Parkinson’s disease (PD) is a common and complex disorder, a good knowledge regarding it is essential for taking the best decisions about the diagnosis and management in standard clinical practice [2].
PD affects approximately 1% of general population worldwide, especially those over the 60 years and about 4% in highest age and it is a rare before 50 years [3,4]. In patient with PD, many symptoms not observed if the patient is not to be asked about them. The emphasis in the last decade has been on the motor symptoms of PD, focusing mainly on tremor, postural instability, rigidity, and bradykinesia. Now, it is recognized that the disease is more pervasive with various non -motor symptoms, also, NMS happen throughout the course illness from early to late diseases and at any time [5]. NMSs are not mentioned by the patients with PD unless asked. These symptoms are undeclared because the embarrassment patient’s sensation, or their caregivers and the motor symptoms take the more chance during the patient interviewing. Moreover, the patients are not asked regarding their symptoms which are overlooked.
The non-motor symptoms (NMSs) of Parkinson’s disease (PD) are a hallmark cause of disability and associated with the deterioration of life quality. Therefore, detection of NMSs is very important to optimum health care for patient with PD in clinical practice.
A few studies investigated the NMSs profile in Egyptian PD patients. The prevalence of PD among Egyptians is the highest ratio comparing with other Arabic countries, which may be due to environmental and genetic factors [6]. As much as, 90% of people with PD report NMSs and a number of studies have shown a negative correlation between NMS and quality of life [7]. Nonmotor symptoms (NMSs) of PD include a variety of symptoms such as neuropsychiatric problems (as cognitive impairment, anxiety, depression, psychosis, compulsive disorders and apathy), autonomic manifestation (bowel problems such as constipation, urinary complaints, sleep disorders, fatigue sensory symptoms, and sexual dysfunction [8].
Non- motor symptoms (NMSs) are affected on health-related quality of life (HRQOL), so their searches started to deal with this issue and in some cases their burden can be more disabling when compared with motor symptoms [9]. In the past two decades, studies about HRQOL have revolved around the effect of motor symptoms such as rigidity, bradykinesia, tremor, gait, and balance problems. More recently, few non-motor symptoms of Parkinson’s disease studies have measured the impact of these symptoms on HRQOL in a holistic manner [9]. It is important to ask and detect the problems of non-motor symptoms and assess their severity in order to improve patient care quality.
Some patients were embarrassed to declare these symptoms with the health care provider (HCP) unless they were prompted such as incontinence of bowel or sexual complains, patients were not aware that these symptoms have been related to PD such as drooling and health care provider (HCP) mainly preoccupied by motor symptoms than non-motor symptoms.
There is now urgent indication for the need of a nurse-led clinic for patients with PD. This nurse is in a unique position to provide information, nursing care, and education to enhance the quality of life [10]. As well as nursing duties, the PD specialized nurse carry out other highly important roles such as providing education, information and therapies regarding the patient and the career. The role of the specialized nurse may reduce unnecessary hospitalization and reduce waiting time of patients and lower costs to the system [11]. Nursing care of patients with PD focus on the bio- psychosocial approach and must be based on legal, ethical and theoretical assumptions for health promotion, treatment, prevention of complications and enhance rehabilitation [12]. So, this study aimed at assessing the prevalence of non-motor symptoms, considered as a whole, and its effect on quality of life in patients with Parkinson’s disease.
Significance of the study
Not much is studied concerning NMSs profiles in patients with Parkinson’s disease. Nursing staff have had an active role regarding PD cases to reduce unnecessary hospitalization and costs of care. NMSs are in a less focus for patients’ families, and people who provide nursing in the care of patients [13]. Recognizing and treating these symptoms are essential for high functional outcome.
This information could help psychiatric staff recognize nonmotor symptoms related to PD and manage them early to improve their quality of life. The development of severe NMSs in PD influences rates of nursing homes and adds to the cost of health care of PD. Rigorously applying non-motor symptoms assessment by trained nursing staff would complement the motor assessment which made by the physician.
Aim of the study
The aim of the study was to assess prevalence of NMSs among patients with Parkinson’s disease and its effect on quality of life QOL.
Research questions
a. What is the frequency of each of NMSs?
b. What is the frequency of NMSs domains?
c. What is the degree of severity of each of NMSs domain?
c. What is the degree of severity of each of NMSs domain?
c. What is the degree of severity of each of NMSs domain?
Parkinson’s disease (PD): Is a multisystem neurodegenerative disorder that is characterized by a combination of motor and nonsymptoms (NMSs). PD is an idiopathic movement disorder which is characterized by resting tremor; bradykinesia, pill-rolling tremor and mask like face [14]. Non -Motor symptoms (NMSs) of PD theoretically include a variety of symptoms such as autonomic manifestations (bowel problems such as constipation, sexual dysfunction, and urinary complaints, neuropsychiatric problems (cognitive impairments depression, anxiety and psychosis), sleep disorders, fatigue and sensory symptoms [15]. In the present study, NMSs operationally defined as the percentage of each non motor symptom and its severity or the mean of each NMS domain, that was measured by non -motor symptoms questionnaire which was developed by Chaudhuri [16].
Quality of life: Is theoretically defined as a state of wellbeing. This is a concept that includes domains related to physical, mental, emotional, and social functioning [17]. QOL in the present study is operationally defined as the total score which the patient with PD is reported on the visual Analogue scale (VAS).
Subjects and Methods
Research Design
A quantitative descriptive correlational research design was used.
Setting: The study was conducted at psychiatric outpatients’ clinics at Menoufia University Hospital, Menoufia, Egypt.
Subjects: A convenience sample of 96 patients with PD. All participants with a confirmed PD diagnosis and who agreed to participate, all ages and both genders were enrolled, and no specific exclusion criteria were set. All patients were on pharmacological and non-pharmacological therapies (e.g occupational, speech therapies, and physical to achieve optimal functioning.
Tools of data collection: Three tools were utilized by the researcher
Tool (I): Personal and medical data: structured interview schedule. This tool was developed by the researcher after reviewing the related literature for the purpose of collecting sociodemographic characteristics which include age, gender, and onset of the disease and duration of it.
Tool (II): The Non-Motor Symptoms Questionnaire (NMSs Quest) which developed by Chaudhuri et al. It is a 30 item, validated, self-completed yes-no-type comprehensive questionnaire. All items detect the presence or absence of symptoms based on yesno answers. It was classified the 30 questions into 9 domains: urinary, cardiovascular, gastrointestinal, sexual, cognition (apathy/ attention/memory), hallucinations/delusions, anxiety/depression, sleep and miscellaneous. Seven questions i.e., dribbling of saliva, reduced taste or smell, dysphagia, nausea, constipation, bowel incontinence and incomplete bowel emptying were included in gastrointestinal domain. While urinary domain included questions on urgency and frequency of micturition. Cardiovascular domain included 2 questions-feeling light-headed and falling (syncope) while feeling sad and feeling anxious/ frightened were questions in anxiety/depression domain. Presence of hallucinations and delusions were the two questions in hallucinations/depression domain, while reduced interest and difficulty in performing sex were included in a sexual domain. Memory problems, loss of interest and difficulty in concentration were classified under memory domain Sleep domain included 5 questions on insomnia, increased drowsiness with difficulty in staying awake, vivid dreams, talking or moving in sleep (rest sleep behavioral disorders), unpleasant sensations in leg (restless leg syndrome) whereas the last 5 questions on unexplained pains, changes in weight, swelling of feet, excessive sweating, and double vision were included in miscellaneous domain. Positive responses are summed up to yield a total score. (NMSs QT) ranges from 0 to 30. Higher scores indicate worse NMSs condition.
Tool (III): EQ-5D visual analogue scale (EQ-5DVAS) This scale has been developed by Boer et al [18] to assess healthrelated quality of life. It is designed for self- completion and asks respondents to rate their own quality of life on a thermometer- like 20cm visual analogue scale form 0 (worst imaginable health state) to 100 (best imaginable health state).
Validity of the tools: The content validity of the tools was tested by a panel of five experts specialized in psychiatric nursing.
Reliability of the tools: The reliability of all tools was tested by intra class reliability coefficient. It was 0.9 for tool I and 0.80 and Cronbach’s alpha above 0.80 for tool II and the internal consistency of tool III was 0.87 and test- retest was 0.90.
Administrative approval: Before starting the study, an administrative approval was obtained from directors of university hospital and psychiatric unit after explanation of the purpose of the study.
Ethical Consideration: Permission to conduct the study was obtained from the hospital authorities of Menoufia University Hospital. Prior to the initial interview, the researcher introduced herself to patients and their relatives and explained the purpose and nature of the study, and then an informed consent was obtained from participants who accept to participate in the study. Anonymity and confidentiality were assured through coding the data.
Pilot Study
A pilot study was carried out on 10% of patients representing the study sample to test the feasibility and clarity of the used tools; modifications were done based on the results. The sample of the pilot study was included [n the final study sample because no modification s was done in the study tools.
Procedure of Data Collection
Data were collected over a period of 11 months from September 2018 to August 2020.The researcher collected the data during the morning at one day/week from 10 AM to 11.15 AM.Statistical analysis
Statistical analysis
After the NMSs questionnaire was filled in by all of the PD patents; Data was entered and analyzed by using SPSS (Statistical Package for Social Science) statistical package version 22. Graphic was done using Excel program. Quantitative data were presented by mean (X) and standard deviation (± SD). Correlation coefficient (r) was used to study the correlation between Quality of life and Non- Motor domains, grand total scores of NMSs; as well as correlation of demographic characters and grand total NMSs score. Qualitative data were presented in the form of frequency distribution tables, number and percentage.
Results
Table 1: Showed that, 96 patients with Parkinson’s disease were enrolled, more than half of them were males (53.1%), and 46.9% were females. The mean age of patients with PD was 65.1±5.4 years, mean age of onset of PD was 57.9±3.6 years, and mean duration of illness was 7.1±2.3 years (Table 1).
Table 1: Personal and medical data of patients with Parkinson’s disease (N. =96).
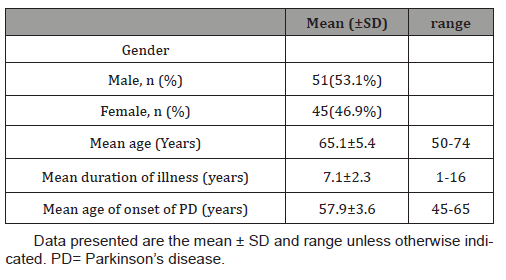
Table 2: Revealed that, all the patients (100%) presented at least one NMSs. Also, high prevalence of urinary urgency (86.5%), followed by nocturia (81.2%), followed by difficulty concentration (78.1%), and then feeling lightheaded dizzy (74%). 63.5% swelling in the legs. 61.5% of patients suffer from the feeling sad or blue. 62.5% had problems with sex (find it difficult to perform sex) and 59.4% had constipation (Table 2).
Table 2: Frequency of each Non -Motor items among studied PD patients (N=96).
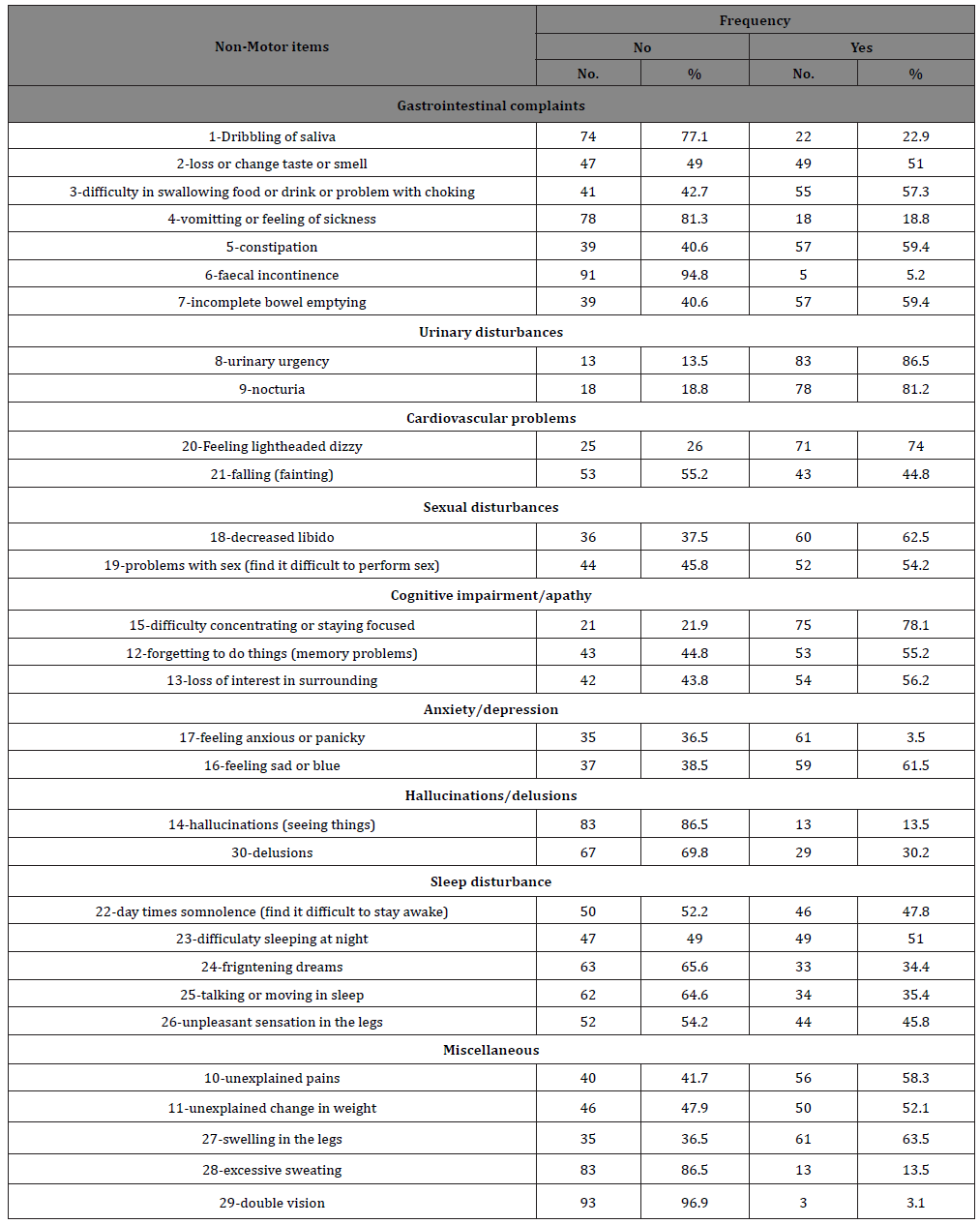
Table 3: Demonstrated that all patients with PD were complaining from one or more of non-motor symptoms. Cognitive impairment/ apathy domain was the most common prevalence one (89.6%), followed by miscellaneous domain (85.6%), GIT complains (82.3%), and urinary disturbance cardiovascular problems (75%). The mean total score of NMSs was 14.7±7.4 and a range of 1-24. The mean QOL score was 57.8±7.2 with a range of 45-80 (Table 3).
Table 3: Frequency and mean of each Non-Motor domains, grand sum NMSs, and mean QOL among studied patients (N=96).
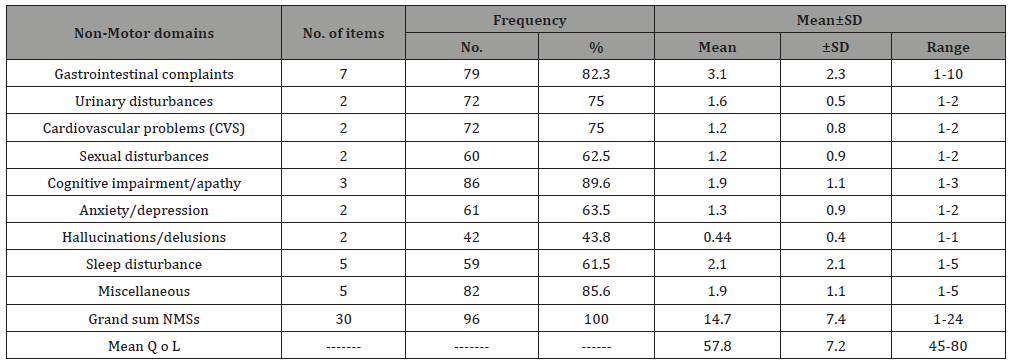
Figure 1: Illustrated that cognitive impairment/apathy domain was the most severe domain (9.9), followed by miscellaneous domain (9.5), GIT complains (9.1), and urinary disturbance cardiovascular problems (8.3 &8.1) respectively (Figure 1).
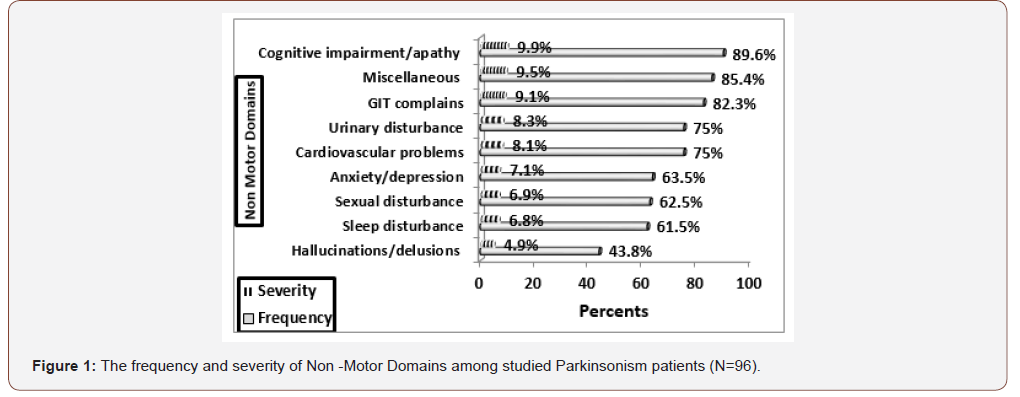
Table 4: Correlation between Quality of life and Non-Motor domains.
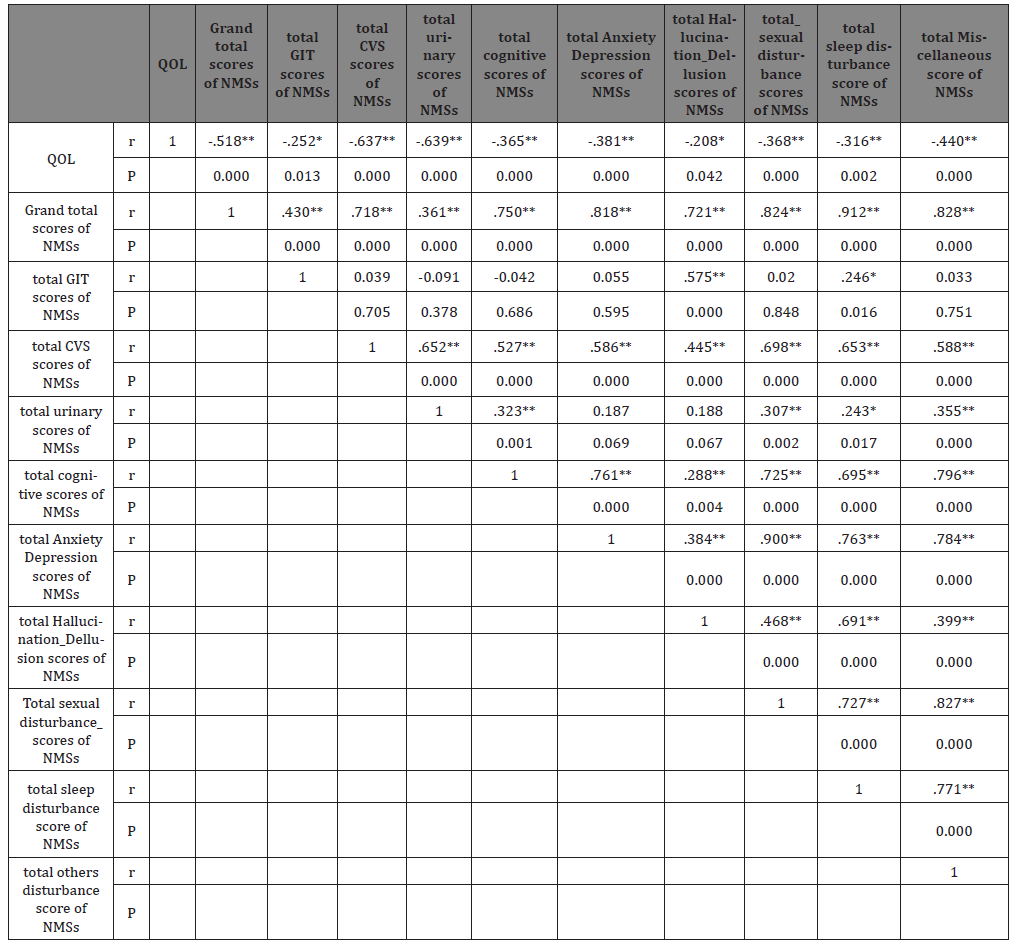
Table 4: Showed that there were negative significant correlations between QOL total score and grand total scores of NMSs as well as its nine domains (Table 4).
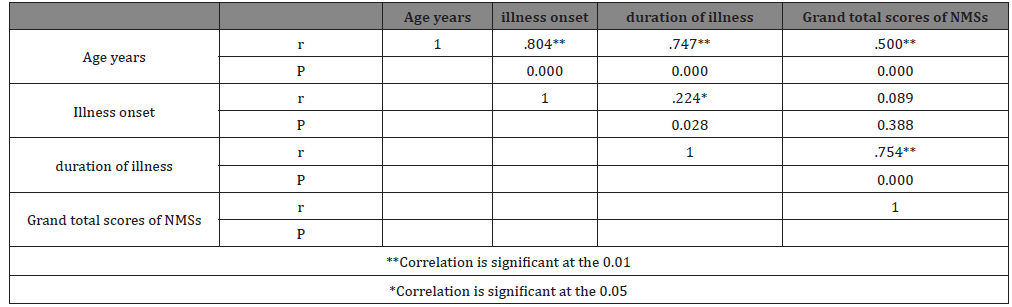
Table 5: There was a positive significant correlation between grand total scores of NMSs and age of patients (the older the patients, the higher is the grand total scores of NMSs (r=0.500). Also, there was a positive significant correlation between grand total scores of NMSs and duration of illness of patients (the longer the duration of illness of patients, the higher is the grand total scores of NMSs (r=0.754). However, this correlation was not observed with illness onset (r=0.089) (Table 5).
Table 5: Correlation of Personal and medical data and grand total NMSs score.
Discussion
Based on the massive research on this issue, it was found that, this study was the first study to be carried in Menoufia to evaluate NMS in PD patients. In this study, the researcher observed a high prevalence rate of NMSs. The general prevalence of NMSs in this study was closing similar to that of previous studies in other countries. This is an indicator of that NMS are very frequent and universal concerns in patient with PD. This study aimed at assessing the effect of non-motor symptoms, considered as a whole, on quality of life in patients with Parkinson’s disease. Non-motor symptoms prevalence varies widely between studies ranging from 17% to 100% depending on the clinical tools used for assessment.
In the current study, the researcher collected data from 96 patients with PD. The basic characteristics included that 53.1% male and 46.9% female with mean age in years was 65.1±5.4. The mean duration of illness was 7.1±2.3 years with range from 1 to 16 years. The mean age of illness onset in years was 57.9±3.6 with range from 45-65 years. These results similar to Tallawy and colleagues [19], who reported that the overall study population consisted of 15.452 subjects with PD in Al Kharga district, Egypt, in which 53.7% male and 46.3% female, aged ≥ 40 years. On the same line, investigated ninety-seven Egyptian patients with PD, 58 males (59.8%) and 39 females (40.2%). The mean age of them 55.3±10.8 years and mean disease onset 50.1±11.2 years [20], also reported that there were 35 men (53%), and 31 women (47%) regarding their study, and the mean age was 59.5 ± 9.3. This result also was congruent with study of Shakthi et al., (2020) who presented that the mean age was 59.3 with range 33-80 years.
The finding of the present study was in harmony [21] who collected data from 210 patients with PD (100 females, 110 male) with mean age 66.1±9 years, and also was congruent with result of Fonticoba and Garcia, who explored that there was a predominance of males and the duration of disease was around 5 years. In the same context [22] stated that the mean age equaled 74.2±8.8 years (range: 47-96years). Duration of the disease was 7.6±5.9 years (range: 0.1-35 years), and age at onset amounted to 66.8±10.1 years (range: 35-88 years). On the other hand, females were more common (51%) and (49%) were males in their study. The result of current study was also similar [23] who reported that the mean age was 64.48 (±9.92) years old, and disease duration was 8.07 (±5.75) years.
This study showed that the grand total score of NMSs was 14.7±7.4 and total quality of life score was 57.8 with range 45- 80. This result was consistent with Chaudhuri et al., (2010) who reported the total mean NMSs Quest was 10.9±5.6 and it also in consistent [22] who found that, non-motor symptoms were reported by 99.6% of the PD participants. On the other hand, stated that the mean of NMSs was 29.6±0.7, and the NMSs mean sum score [24] study was 87.9±48.9.
Lee and Koh [25] reported that the mean NMSs Quest total score was 6.76±4.22, this result in comparing with the result of present study was low, this means that the prevalence of NMSs in this study was high. This high difference in the results may be due to different reasons as the using of different tools, the duration of the disease severity, education, economic status, availability of psychiatric services, and treatment strategies were predictors of NMSs prevalence.
Regarding the frequency and prevalence of NMSs among the current studied sample, all the patients (100%) presented at least one NMSs, this finding can be explained by the so relatively long disease duration of 16 years and the present results were in line with previous studies [26] also stated that the NMSs presented in 98.7% of patient with PD. A similar high prevalence of NMSs and frequency of NMSs domains were reported in Upper Egypt [27]. The NMSs profile was consistent with depression and anxiety in Egyptian patients.
In the present study, out of the nine NMSs domains, the cognitive domain had the highest prevalence, and highly severity, (89.6% with 9.9% severity). Difficult concentration was the most prevalent cognitive domain (78.1%). The previous domain was followed by miscellaneous domain (85.6%with 9.5% severity). Swelling in the legs and unexplained pains were common in miscellaneous domain (63.5 and 58.3%) respectively. Gastrointestinal domain was the third prevalent one (82.3%) and constipation was the dominant complain (59.4%) The fourth prevalent domains were urinary and cardiovascular (75%of each).
Anxiety and depression domain presented in 61.5% of patients. These results may be due to the old age of the present sample. So, the increasing age, the increasing prevalence of NMSs, and also using of different tools [28] reported that some studies have found association between increasing age and the total load of non-motor symptoms. A growing body of literature suggests that advancing disease severity and duration are associated with a higher frequency of non-motor symptoms and increasing age [29,30]. Eerme et al. reported “The higher rate of cognitive impairment among our patients might at least partly be explained by the older mean age and more advanced disease severity, that is, the mean age was 74.2years”.
Regarding the frequency of NMS, the present study revealed that urinary urgency was more frequent, followed by nocturia, then difficulty concentration and feeling lightheaded dizzy. Feeling anxious was more than feeling sad or blue. Other studies asserted opposite results with high prevalence of other symptoms. The most common non-motor symptoms were the following: nocturia, urgency, remembering, constipation, sad and blue, anxiety and (drooling) dribbling.
Tibar et al evaluated that the most common NMS were urinary dysfunction (82.6%), sleep (80.6%), and gastrointestinal (80%), other autonomic symptoms as cardiovascular troubles (50.9%) and sexual dysfunctions 47.9%. Depression presented in 47.9% and fatigue symptoms in 23.1%. Regarding the frequency of NMSs in study [31], they found that the more frequent symptoms are urinary disturbances, gastrointestinal complaints, sexual disturbance and cognitive impairment (73.2%, 67.86%, 51.7%and 46.4%) respectively. However, anxiety and depression were 28.5 %. This study indicated that 61.5% of patients had feeling sad or blue. This result was in the same line [32], who stated “Patient with non-motor symptoms demonstrated more doubts and anxieties”. Besides, fatigue was the most frequent symptom (81.8%), followed by mood symptoms (sadness 75%, anxiety or nervousness 69 %, and lack of motivations was 68.5 %, forgetfulness was 65.5%, and urinary symptoms was 58.6 %. The study results of Fonticoba and Garcia, reported the percentages of patient who represented NMS as 65% suffer from fatigue, 55% urinary problem 45% concentration problems. They also stated “1out of every 4 presented with cognitive impairment criteria, 18 % had depression, 63% pain, and 20%falls”.
Regarding the effect of NMSs on quality of life on patients with PD, many studies have declared that non-motor features have a greater effect on PD patient’s quality of life than motor symptoms. In general, the current study revealed that there was a negative correlation between NMSs and quality of life. It means that NMSs domains were correlated with the quality of life. The most severe and frequent NMSs are, the more impaired QOL. In the present study, the mean quality of life score was 57.8 (35-80). Shalash (2018) et al., results revealed “The mean score of quality of life which is measured by PQ-10 was 6.9±1.5 (1-10) and another score by EUROHIS-QOL-8 item index was 29.6±3.5 (19-37)”. The research results were interpreted due to using different quality of life instruments by Liu et al, and Shalash et al.
A study of Eerme et al, reported that non-motor symptoms had a quite positive relationship with a decreasing in the quality of life, otherwise, other studies revealed no relationship [33]. In this study, although the cardiovascular and urinary symptoms were the most prevalent in patient with PD, the correlation between cardiovascular and urinary symptoms and quality of life (r=- 637 was low comparing with other symptoms. This may be due to that the cardiovascular and urinary symptoms rarely induce motor disturbance and psychological problems comparing with others. This result in consistent with Liu et al (2015) in which they emphasized that the correlation between urinary symptoms and HRQOL was low.
Neuropsychological symptoms were highly influenced the patient’s quality of life (r = 0.176). Anxiety and depression strongly correlated with quality of life (r =-381). In this study, 61.5% of patients reported anxiety and depression and they more correlated with QOL (r =-381) and it can be suggested as the most predictor of QOL. Depression is two-to three more prevalent among patient with PD as reported by Liu et al., and also suggested that NMSs are the major predictors of patient’s quality of life and can cause more disability than motor symptoms.
Conclusion
In conclusion, the present study showed that non- motor symptoms had an effect on the quality of life. So, assessment and management of NMS results in the improvement of the quality of life of patients with PD and all patients had represented at least one of NMSs.
Recommendations
1. The more assessment and management of non- motor symptoms is as important as motor symptoms and there is a need for large and well- designed community-based study on the NMS.
2. The involvement of a PD nurse specialist (PDNS) to offer education to the patients with PD, the wider community, and training of clinical and non-clinical staff. These actions help in improving quality of life of patient, the family, and the community.
Acknowledgment
I am very grateful to Allah and the patients who participated in this study in addition; I would like to thank psychiatric nursing stuff in the inpatient section for kind cooperation.
Conflict of Interest
No conflict of interest.
References
- Pederensm S, Sudemey M, Lium L, Domagkm D, Forbes A, et al. (2017) The role and structure of the multidisciplinary team in the management of advanced Parkinson's disease with of focus ou the use of levodopa carbidopa intestinal gel. J Multid Health care 10: 13-27.
- Fonticoba T, Garcia D (2018) The role of nurse specialists in the evaluation of non-motor symptoms within the overall care of patients with parkinson’s disease.
- Tibar H, El Bayad K, Bouhouche A, Haddou E, Benomar A, et al. (2018) Non-motor symptoms of Parkinson's disease and their impact on quality of life in a cohort of Moroccan patients. Font Neuro 9: 170.
- Tosin M Oliveira B (2016) The role of nurses in Parkinson's disease. Challenges in Parkinson's disease.
- Chaudhuri K, Prieto Jurcynska C, Naidu Y, Mitra T, Frades Payo B, et al. (2010) The Non declaration of Non-motor Symptoms of Parkinson’s Disease to Health Care Professionals: An International Study Using the Nonmotor Symptoms Questionnaire. Mov Dis 25(6): 704-709.
- Shalash A, Hamid E, Elrassas H, Bedair A, Abushouk A, et al. (2018) Non-motor symptoms as predictors of quality of life in Egyptian patients with Parkinson's disease: a cross-sectional study using a culturally adapted 39-item Parkinson's disease questionnaire. Front Neurl 9: 357.
- Shakthi C, Sritharaum B, Muthuveeranm M, Mani Vannanm M, Justinm C, et al. (2020) Prevalence of non-motor symptoms in Parkinson's diseases. Int J research in med Scien 7(5): 1459-1464.
- Mukhtarm S, Imranm R, Zaheerm M, Tarian H (2017) Frequency of non-motor symptoms in Parkinson's disease presenting to tertiary care center in Pakistan: A dissertational, cross-sectional study. BMJ Open 8(5): e019172.
- Violante M, Garcia N, Avila N, Fino D, Landero A, et al. (2018) Motor and non-motor wearing off and its impact on the auality of life of patients with Parkinson's disease. Arq Neuropsiquiatr 6(8): 517-521.
- Martin A, Mills J (2013) Parkinson’s disease nurse specialist and the king’s college model of care. British J Neuroscince Nursing 9(1): 22-26.
- Axelrol L, Gage H, Kaye J, Bryan K, Trend P, et al. (2010) Workload of Parkinson's specialist nurses: implication for implementing national service guidelines in England. J Clin Nurs 19(23-24): 3575-3580.
- Tosin M, Campos D, Blanco L, Santanam R, Oliverira G (2015) Mapping nursing language terms of Parkinson's disease. Rev Esc En ferm 49(3): 409-416.
- Skogarm O, Nilssonm M (2018) Distribution of non-motor symptoms in idiopathic Parkinson's disease and secondary Parkinsonism. J Multidiscip Healthc 11: 525-534.
- Ravan A, Ahmad F, Chabria S, Gadhari M, Sankhla C (2015) Non-motor symptoms in an Indian cohort of Parkinson's disease patients and correlation of progression of non-motor symptoms with motor worsening. Neurol India 63 (2): 166-174.
- Zafari A, Bagheri S, Taherian R (2017) Non-motor symptosm of parknon’s disease and health related quality of life. Amini-review Int clin.Neuroscience J 4(3): 79.
- Chaudhuri K, Martinez Martin P, Brown R, Sethi K, stocchi F, et al. (2007) The metric properties of a novel non-motor symptoms scale for Parkinson's disease: results from an international pilot study. Mov Dis 22: 1901-1911.
- Theofilou P (2013) Quality of life: definition and measurement. Eur J Psychology 9(1): 150-162.
- Boer AG, Lanschot JJ, Stalmeier JW, Van Sandick JB., Hulscher JC, et al. (2004) Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual Life Res 13: 311-320.
- El Tallawy H, Farghaly W, Shehata G, Rageh T, Hakeem N, et al. (2013) Neuro psych Dis and treatment. 1821-1826.
- Katsarou B, Karakaisis C, Peitsidou EB, Rossopoulos N (2013) Evaluation of non-motor symptoms in Parkinson's disease: An underestimated necessity. Hippokratia 17(3): 214-219.
- Liu W, Lin R, Yu R, Tai C, Lin C, et al. (2015) The impact of non-motor symptoms on quality of life in patients with Parkinson's disease in Taiwan. Neuropsychiatr Dis Treat 11: 2865-2873.
- Eereme L, Muldmaa M, Lilles S, Rosenthal M, Taba N, et al. (2016) Non motor features in Parkinson's disease: what are the most important associated factors? Park Disease.
- Martin M, Blazauez R, Kurtis M, Chaudhuri K (2011) The impact of non-motor symptoms on health-related quality of life of patients with Parkinson's disease. Mov Disord 26(3): 399-406.
- Weerkamp N, Tissingh G, Poels P, Zuidema S, Munneke M, et al. (2013) Nonmotor symptoms in nursing home residents with Parkinson's disease: prevalence and effect on auality of life. J Am Geriatr Soc 61(10): 1714-1721.
- Lee H, Koh S (2014) Many faces of Parkinson's disease: Non-motor symptoms of Parkinson's disease. J Mov Disord 8(2): 92-97.
- Gökçal E, Gür V, Selvitop R, Babacun G, Asil T (2017) Motor and non-motor symptoms in Parkinson's disease: Effects on Quality of life. Arch Neuropsychiatry 54(2): 143-148.
- Khedr E, Fawi G, Abbas M, Mohammed T, El Fetoh N et al. (2015) Prevalence of Parkinsonism and Parkinson's disease in Qena governorate/Egypt: a cross-sectional community-based survey. Neurol Res 37: 607-18.
- Spica V, Pekmezovic M, Svetel M, Kostic (2013) Prevalence of non-motor symptoms in young onset versus late onset Parkinson's disease. J Neurol 260(1): 131-137.
- Krishnan S, Sarma G, Sarma S, Kishore A (2011) Do nonmotor symptoms in Parkinson's disease differ from normal aging? Mov Disord 26(11): 2110-2113.
- Kim H, Cheons S, Seo J, Ryu H, Park K, et al. (2013) Non motor symptoms more closely related to Parkinson's disease: Comporison with normal elderly. J Neurol Sci 324 (1-2): 70-73.
- Mirdula K, Borgohain R, Jabeen S, Padmafam G, Bandaru V, et al. (2015) Comparison of frequencies of non-motor symptoms in Indian Parkinson’s disease patients on medical management versus deep brain stimulation: A case-control study. Iran J Neurol 14(2): 86-93.
- Tosin M, Campos D, Andrade L Oliveira G, Santana R (2016) Nursing interventions for rehabilitation in Parkinson's disease. Cross mapping of terms. Rev Lat Am Enfermagem 24: e2728.
- Duncan G, Khoo T, Yornall A (2014) Health-related quality of life in early Parkinson's disease: the impact of non-motor symptoms. Mov Disord 29(2): 195-202.
-
Lamiaa Hassnin Eita. Non-Motor Symptoms among Patients with Parkinson’s Disease: The Prevalence and its Effect on Quality of Life. Iris J of Nur & Car. 2(4): 2020. IJNC.MS.ID.000541.
-
Parkinson’s Disease, Non-Motor Symptoms, Quality of Life, Neurodegenerative Movement Disorders, Alzheimer Disease, Bradykinesia, Tremor, Nursing Care, Bio-Psychosocial Approach, Sexual Dysfunction, Urinary Complaints, Sleep Disorders, Neuropsychiatric Problems, Depression, Anxiety, Psychosis, Gastrointestinal
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






