 Mini Review
Mini Review
Management and Prevention of Fall Risk: A Literature Review
Sciandrone Gaetano Giuseppe*
Nurse at the Pulmonology Unit, IRCCS San Matteo Foundation Pavia 27100 (PV), Italy
Sciandrone Gaetano Giuseppe, Nurse at the Pulmonology Unit, IRCCS San Matteo Foundation Pavia 27100 (PV), Italy
Received Date: July 19, 2025; Published Date: July 23, 2025
Abstract
Falls are a global problem. Each year, approximately 600,000 falls worldwide result in death, making them a leading cause of traumatic death (World Health Organization, 2018). Due to biological changes, older adults are at increased risk of falling. Approximately half of nursing home residents experience a fall at least once a year (Rapp et al., 2012). Nearly 10% of older patients admitted to hospital units experience falls (Castellini et al., 2017), with more than a quarter suffering physical injuries (Anderson et al., 2012; Basic & Hartwell, 2015). In addition to physical consequences, falls also have psychological and social consequences. Fear of falling, the most common psychological consequence, leads to a reduction in physical and social activities (Lavedan et al., 2018).
Objectives: Identify suitable tools to prevent the risk of falling.
Materials and Methods: A literature review of quantitative studies was performed using the PIO methodology.
P: (Population and Problem) Human Population over 65
I: (Intervention) Interventions implemented to reduce the risk of falling
O: (Outcomes or themes) Prevent the risk of falling
The following filter was used to search for articles:
• Publication Last 5 years
• Systematic Reviews and Meta-Analyses
• Free full test
Conclusions: Motion sensors placed in rooms, chairs, or the patient’s bed do not reduce the patient’s risk of falling, while good physical activity with targeted strength exercises and, above all, training the patient’s balance reduces the risk of falling.
Keywords: Nurse-fall Risk-prevention
Introduction
The World Health Organization (WHO) defines the term fall as the consequence of any event that hurls an individual to the ground against their will. Accidents are the sixth leading cause of death in people over 65 years of age, and falls are the leading cause of accidental death, especially in older adults, whether preventable or not. Falls are a global problem. Every year, approximately 600,000 falls worldwide result in death, making them a leading cause of traumatic death (World Health Organization, 2018). Falls account for 38% of adverse hospital events, and approximately 30% of in-hos pital falls result in injury, with approximately 4% to 6% resulting in serious injuries, such as fractures, subdural hematoma, bleeding, and death. In addition to the physical consequences, falls also have psychological and social consequences. Fear of falling, the most common psychological consequence, leads to a reduction in physical and social activities (Lavedan et al., 2018). Falls prevention education (FPE) is one strategy to reduce falls (Kamei et al., 2015; Ott, 2018). Providing FPE also improves positive healthcare outcomes in older people (Chaudhry, 2020; Chidume, 2021), as they become more independent in their perceived quality of life to perform daily activities and live in a safer environment (Minnier et al., 2019). Al though falls can occur throughout life, people aged 65 and over are at the highest risk of falling in hospital. The resulting consequences of a fall can significantly impact a person’s overall quality of life or more likely lead to a life-threatening event (Australian Commission on Safety and Quality in Health Care [ACSQHC] 2018b). Falls occur in hospital and community settings and are a major concern in nursing. Although falls can occur at any time throughout a person’s lifespan, risks vary based on age, gender, and other factors. Some risk factors are intrinsic (e.g., visual impairment and mobility) and others are extrinsic (e.g., medications; Xu et al., 2017). Falls are a well-known quality indicator sensitive to nursing care and a patient care outcome reported in the National Nursing Quality Indicators Database (Madaris, 2023). Although the risk of falling is often associated with older adults (Appeadu & Bordoni, 2023; World Health Organization, 2021a), women during pregnancy, labor, and the postpartum period may also be at increased risk. Postural stability decreases as pregnancy progresses (El- Shamy et al., 2016; Opala- Berdzik et al., 2015; Shingala et al., 2019) and remains impaired during the postpartum period (Opala-Berdzik et al., 2015), placing women at high risk for falls. After childbirth, women have different risk factors for falls compared to other patients, such as postpartum haemorrhage and no food intake after birth for more than 6 hours (Xu et al., 2017).
Nurses can focus on identifying patients at particular risk of falling, and population stratification for this purpose is possible using assessment tools to quantify risk. For example, the Morse Fall Scale is a classic tool used to assess fall risk in the general patient population (Morse et al., 1989).
Methods
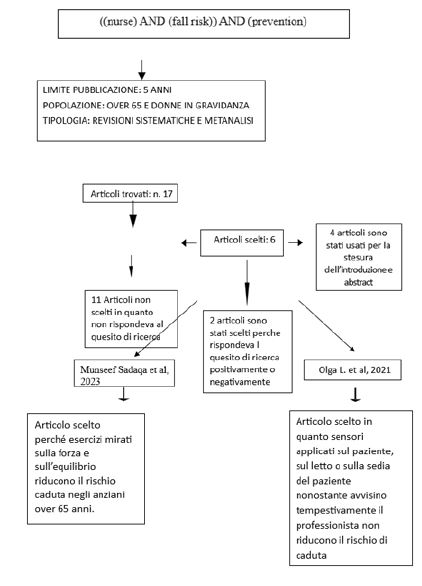
The research was conducted using the research question that I posed as the starting point of my research: Which prevention interventions on patients reduce the risk of falling?
I conducted the research using the PIO methodology which allowed me to identify the keywords and subsequently the articles related to the chosen topic:
• P (Population and Problem): The skills of the healthcare professional
• THE (Intervention): strategies harvest in act from the professional
• (Outcomes or themes): Reduction of fall episodes during hospital stay
Their research of the articles and was conduct on Bank Data PubMed, Where I have used the following keywords: Nurse- fall Risk- prevention by combining and/or including them together through the use of Boolean operators AND OR, obtaining results that contain the related terms at the same time or both.
MeSH (Medical Subject) terms. Headings).
S Strings of Research and Tables
The strings of research with the results obtained and the criteria adopted I am the following:
Discussion
Motion Sensors
Most falls occur in patient rooms, accounting for more than half of all falls. Other common locations include the hallway outside the room and the bathroom inside the room.
The installation of bells and alarms in hospitalized patient rooms alerts caregivers to the need for movement of patients who require assistance. However, the use of this patient-activated light or bell alarm system is questionable in preventing falls, especially when the patient doesn’t communicate movement due to health problems; therefore, changes in position and the initiation of walking aren’t detected by the nurse in time before the fall occurs.
The use of motion sensors with alarms has been studied as predictive devices for hospital-level falls. These are offered to caregivers as devices installed on beds and chairs (pressure sensors), or less frequently attached to patients (portable accelerometers-gyroscopes), with the ability to predict falls in hospitalized patients. Is there an impact on falls among adult patients receiving preventive care with sensor-based devices placed on hospital-use or portable items during hospitalization?
The primary objective was to conduct a systematic review of the available scientific literature exploring the impact of the use of sensor-based devices to prevent falls in adults and older adults in hospital settings. Furthermore, this study describes the technical development aspects of the sensors and the implementation characteristics identified in each of the studies.
The study by Olga et al. included randomized controlled trials (RCTs) in which hospitalized patients were assigned to wearable sensors (portable or attached to the bed, chair, or other items) diagnosed with any medical or surgical condition. The intervention under consideration was defined as the use of sensors that tracked changes in movement during hospitalization (such as from lying to sitting; from sitting to standing and walking), monitored throughout the patient’s hospitalization, and implemented with the goal of preventing patient falls.
Of the four studies found, three used sensors fixed to the bed, bedside chair, or chair in the room. Only one study evaluated the impact of sensors (accelerometers) attached to the patient’s body (thigh with Velcro). The sensors attached to the bed or bedside chair were pressure sensors that produced an alarm when the patient stood up and broke contact with the sensor.
The sensors identified in the studies included in this meta-analysis failed to predict falls in real time. Because the sensors, which are placed on beds or chairs, are static and activated by patients’ hand pressure on the devices, they do not provide a reliable and predictive alert if the patient moves away from the sensor. On the other hand, once the alarm stops, it can be interpreted as if an atrisk patient has stopped moving, thus potentially causing a mobility- related fall. If the sensors are not adequately programmed to identify changes in broad-spectrum movement, possibly before atrisk patients stand, they are unable to capture true and false positives, thus reducing their predictive power (positive or negative).
This study highlights the increase in falls in hospitalized older adults using motion sensors placed on the bed or chair in their rooms.
Physical Activity as Fall Prevention
Physical inactivity and deficits in functional ability (e.g., reduced lower limb muscle strength and impaired balance) have been identified as independent contributors to falls and fall-related injuries (e.g., head injuries and hip fractures) among older adults. Although they are critical risk factors for older adults, they are modifiable and preventable through exercise. Physical training is widely recognized as an appropriate intervention strategy for improving functional performance in older adults by reducing these risk factors and consequently minimizing the risk of falling. Furthermore, reducing physical inactivity has been shown to have positive economic impacts at the national, societal, and individual levels. Cognitive decline also occurs during normal aging, which is considered a significant factor in increasing functional dependence and decreasing activities of daily living among older adults. Consequently, the WHO recommends that older adults over 65 adopt an active lifestyle that includes a minimum of 150 minutes of moderate- intensity physical activity per week, in addition to engaging in fall prevention exercises. This moderate amount of physical activity has been shown to reduce risk factors associated with falls by up to 50%, reducing functional limitation in older people and ultimately reducing the risk of falls.
The included studies involved 4,330 participants, of whom 4,121 participated at the end of the studies and were analysed for outcome measures. The mean age of participants ranged from 66.4 to 82.4 years, and all were older adults living in the community. The interventions were conducted primarily in gyms, exercise studios, community facilities, combined gyms, home-based settings, and laboratories.
A variety of training equipment was used: resistance training machines, recumbent trainer, stationary seated cycle ergometer, treadmill, stair climber, recumbent bike, weighted equipment such as cuff and vest weights, resistance bands/tubing, free weights, body weights, balls, steps, chairs, equipment used for balance training such as non-slip tiles, balance foams, soft wedge mat, soft pads, non-inverted BOSU® balls, BOSU® balls, balance cushions, balance beams, semi-circular blocks, Posturomed , wobble boards, and inflatable discs.
The duration of exercise interventions ranged from 15 minutes to 90 minutes per session, the frequency of interventions ranged from once per day to five times per week, and the duration of exercise programs ranged from 1 week to 2 years.
Although poor muscle strength is an established risk factor for falls, strength training has been found to have no significant effect on falls when a person has sufficient strength to avoid falling. Furthermore, strength training as a single intervention has shown no evidence of being effective in preventing falls. However, strength training is likely to offer long-term fall prevention and other health benefits for older adults. To be effective, strength training should provide a certain amount of resistance in an exercise, and a maximum of 10–15 repetitions should be completed before reaching muscle fatigue. Similarly to strength training, balance training as a single intervention has shown no evidence of being effective in reducing the rate and risk of falls, yet including balance training in exercise programs appeared to be a crucial factor in reducing falls. Furthermore, it is recommended that exercises provide a moderate or high balance challenge to prevent falls. Thus, this explained that different exercise programs that included balance training were equally effective in reducing falls.
Therefore, practicing regular physical activity is essential for reducing and preventing chronic diseases, maintaining a healthy musculoskeletal system and balance, and reducing the risk of falls.
In conclusion, our review included numerous RCTs of physical exercise interventions, including strengthening and balance interventions, on physical function and the risk of falls in community- dwelling older adults. This review confirms previous findings that exercise improves the components of functional ability, namely, strength, balance, and lower limb mobility. Furthermore, exercise reduces falls and minimizes their serious consequences.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Hamm J, Money A, Atwal A, Paraskevopoulos I (2016) Fall prevention intervention technologies: A conceptual framework and survey of the state of the art. J Biomed Inform 59: 319-45.
- Cameron ID, Dyer SM, Panagoda CE, et al. (2018) Interventions for prevention falls in older people incare facilities and hospitals. Cochrane Database of Systematic Reviews (9): CD005465.
- Montesinos L, Castaldo R, Pecchia L (2018) Wearable inertial sensors for fall risk assessment and prediction in older adults: a systematic review and meta-analysis. IEEE Trans Neural Syst Rehabil English 26: 573-582.
- Sun R, Sosnoff J (2018) Novel sensing technology in fall risk assessment in older adults: A systematic review. BMC Geriatr 18(14).
- Liua L, Strouliab E, Nikolaidisc I, Cruz AM, Rios A (2016) Smart homes and home health monitoring technologies for older adults: a systematic review. Int J Med Inform 91: 44-59.
- Higgins JPT, Green S (Eds) (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration.
- Wolf KH, Hetzer K, Zu Schwabedissen HM, et al. (2013) Development and Pilot study of a bed-exit alarm based on a body-worn accelerometer [Entwicklung und Pilotstudie eines Bettenausstiegsalarms middle kör - perbezogener Beschleunigungssensoren]. Zeitschrift for Gerontologie und Geriatrie 8: 727-33.
- Kwok T, Mok F, Chien WT, Tam E (2006) Does access to bed-chair pressure sensors reduce physical restraint use in the rehabilitative care setting? J Clin Nurs 15: 581-7.
- Shorr RI, Chandler AM, Mion LC, et al. (2012) Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients in a cluster randomized trial. American College of Physicians 157: 692-9.
- Bet P, Castro P, Ponti MA (2019) Fall detection and fall risk assessment in older persons using wearable sensors: A systematic review. Int J Med Inform 30.
- Uusi-Rasi K, Patil R, Karinkanta S, Kannus P, Tokola K, et al. (2017) A 2-year follow-up after a 2-year RCT with vitamin D and exercise: effects on falls, injured falls and physical functioning among older women. J Gerontol Ser A 72: 1239-45.
- Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, et al. (2010) Risk factors for falls in community-dwelling older people: a systematic review and Meta-analysis. Epidemiology 21: 658-68.
- Karinkanta S, Piirtola M, Sievänen H, Uusi- Rasi K, Kannus P (2010) Physical therapy approaches to reduce fall and fracture risk among older adults. Nat Rev Endocrinol 6: 396-407.
- Lee TW, Ko IS, Lee KJ (2006) Health promotion behaviours and quality of life among community-dwelling elderly in Korea: a cross-sectional survey. Int J Nurs Stud 43: 293-300.
- Benichou O, Lord SR (2016) Rationale for strengthening muscle to prevent falls and fractures: A review of the evidence. Calcif Tissue Int 98: 531-45.
- Toraman A, Yıldırım NÜ (2010) The falling risk and physical fitness in older people. Arch Gerontol Geriatr 51: 222-6.
- Franco MR, Pereira LS, Ferreira PH (2014) Exercise interventions for preventing falls in older people living in the community. Br J Sports Med 48: 867-8.
- Paterson DH, Warburton DE (2010) Physical activity and functional limitations in older adults: a systematic review related to Canada's physical activity guidelines. Int J Behav Nutr Phys Act 7: 38.
- Wang RY, Wang YL, Cheng FY, Chao YH, Chen CL, et al. (2015) Effects of combined exercise on gait variability in community-dwelling older adults. Age 37: 9780.
- Ács P, Stocker M, Füge K, Paár D, Oláh A, et al. (2016) Economic and public health benefits: the result of increased regular physical activity. Eur J Integr Med 8: 8-12.
- Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, et al. (1999) Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 56: 303-8.
- Lara E, Koyanagi A, Caballero F, Domènech-Abella J, Miret M, et al. (2017) Cognitive reserve is associated with quality of life: a population-based study. Exp Gerontol 87: 67-73.
- Boente Antela B, Leirós-Rodríguez R, García-Soidán JL (2020) Compliance with the recommendations of the World Health Organization on the practice of physical activity in people over 65 years in Spain. J Hum Sport Exerc 17: 29-38.
- World Health Organization (2010) Global recommendations on physical activity for health.
- World Health Organization (2008) WHO global report on falls prevention in older age.
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, et al. (2012) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2021: CD007146.
- Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, et al. (2019) Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019: CD012424.
- LaStayo P, Marcus R, Dibble L, Wong B, Pepper G (2017) Eccentric versus traditional resistance exercise for older adult fallers in the community: a randomized trial within a multi-component falls reduction program. BMC Geriatr 17: 149.
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, et al. (2008) Effective exercise for the prevention of falls: a systematic review and Meta-analysis. J Am Geriatr Soc 56: 2234-43.
- Sherrington C, Tiedemann A, Fairhall N, Close JCT, Lord SR (2011) Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. NSW Public Health Bull 22: 78-83.
- Arnold C, Lanovaz J, Oates A, Craven B, Butcher S (2015) The effect of adding core stability training to a standard balance exercise program on sit to stand performance in older adults: A pilot study. J Aging Phys Act 23: 95-102.
- Li F, Harmer P, Eckstrom E, Fitzgerald K, Chou LS, et al. (2019) Effectiveness of tai ji quan vs multimodal and stretching exercise interventions for reducing injurious falls in older adults at high risk of falling: Follow-up analysis of a randomized clinical trial. JAMA Netw Open 2: e188280.
- El-Khoury F, Cassou B, Latouche A, Aegerter P, Charles MA, et al. (2015) Effectiveness of two-year balance training program on prevention of fall induced injuries in at risk women aged 75-85 living in community: Ossébo randomized controlled trial. BMJ 351: h3830.
- Hirase T, Inokuchi S, Matsusaka N, Okita M (2015) Effects of a balance training program using a foam rubber pad in community-based older adults: A randomized controlled trial. J Geriatr Phys Ther 38: 62-70.
- Lacroix A, Kressig RW, Muehlbauer T, Gschwind YJ, Pfenninger B, et al. (2016) Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: A randomized controlled trial. Gerontology 62: 275-88.
- Patil R, Uusi- Rasi K, Tokola K, Karinkanta S, Kannus P, et al. (2015) Effects of a multimodal exercise program on physical function, falls, and injuries in older women: A 2-year community-based, randomized controlled trial. J Am Geriatr Soc 63: 1306-13.
- Johnson SL, Stevens SL, Fuller DK, Caputo JL (2019) Effect of lower-extremity eccentric training on physical function in community-dwelling older adults. Phys Occup Ther Geriatr 37: 298-312.
- Rieger MM, Papegaaij S, Pijnappels M, Steenbrink F, van Dieën JH (2020) Transfer and retention effects of gait training with anterior-posterior perturbations to postural responses after medio-lateral gait perturbations in older adults. Clin Biomech 75: 104988.
- Kocaman AA, Kırdı N, Aksoy S, Elmas Ö, Dogu BB (2021) The effect of different exercise training types on functionality in older fallers: A pilot randomized controlled trial. Top Geriatrician Rehabil 37: 114-27.
- Ansai JH, Aurichio TR, Gonçalves R, Rebelatto JR (2016) Effects of two physical exercise protocols on physical performance related to falls in the oldest old: a randomized controlled trial: Exercises protocols in oldest old. Geriatrician Gerontol Int 16: 492-9.
- Arghavani H, Zolaktaf V, Lenjannejadian S (2020) Comparing the effects of anticipatory postural adjustments focused training and balance training on postural preparation, balance confidence and quality of life in elderly people with history of a fall. Aging Clin Exp Res 32: 1757-65.
- Chittrakul J, Siviroj P, Sungkarat S, Sapbamrer R (2020) Multi-system physical exercise intervention for fall prevention and quality of life in pre-frail older adults: a randomized controlled trial. Int J Environ Res Public Health 17: 3102.
- Eckardt N (2016) Lower-extremity resistance training on unstable surfaces improves proxies of muscle strength, power and balance in healthy older adults: A randomized control trial. BMC Geriatr 16: 191.
- Hamed A, Bohm S, Mersmann F, Arampatzis A (2018) Exercises of dynamic stability under unstable conditions increase muscle strength and balance ability in the elderly. Scand J Med Sci Sports 28: 961-971.
- Karinkanta S, Kannus P, Uusi- Rasi K, Heinonen A, Sievänen H (2015) Combined resistance and balance-jumping exercise reduces older women's injured falls and fractures: 5-year follow-up study. Age Aging 44: 784-789.
- Lee SH, Lee DY (2019) Effects of open and closed kinetic chain exercises on the balance using elastic bands for the health Care of the Elderly Females. Medical- Leg Update 19: 728.
- Okubo Y, Sturnieks DL, Brodie MA, Duran L, Lord SR (2019) Effect of reactive balance training involving repeated slips and trips on balance recovery among older adults: A blinded randomized controlled trial. J Gerontol Ser A 16(74): 1489-1496.
- Park J, Lee J, Yang J, Lee B, Han D (2015) Effects of combined exercise on changes of lower extremity muscle activation during walking in older women. J Phys Ther Sci 27: 1515-1518.
- Pourtaghi F, Moghadam ZE, Ramezani M, Vashani HB, Mohajer S (2017) The effect of resistance training using Thera-band on muscular strength and quality of life among the elderly in the City of Mashhad. Evid Based Care 7: 7-16.
- Sannicandro I (2018) Effects of strength and core stability training versus strength and aerobic training in subjects aged over 65. Med Sport 70: 410-418.
- Song HS, Kim JY (2015) The effects of complex exercise on walking ability during direction change and falls efficacy in the elderly. J Phys Ther Sci 27: 1365-1367.
- Zhao Y, Chung PK, Tong TK (2016) Effectiveness of a community-based exercise program on balanced performance and fear of falling in older nonfallers at risk for falling: a randomized study. Control Study J Aging Phys Act 24: 516-24.
- Zhao Y, Chung PK, Tong TK (2017) Effectiveness of a balance-focused exercise program for enhancing functional fitness of older adults at risk of falling: A randomized controlled trial. Geriatr Nur 38: 491-7.
- Moreland JD, Richardson JA, Goldsmith CH, Clase CM (2004) Muscle weakness and falls in older adults: A systematic review and meta-analysis. J Am Geriatr Soc 52: 1121-9.
- Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, et al. (2009) American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 41: 1510-1530.
- Singh NA, Stavrinos TM, Scarbek Y, Galambos G, Liber C, et al. (2005) A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J Gerontol a Biol Sci Med Sci 60: 768-776.
- Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, et al. (2005) Tai chi and fall reductions in older adults: A randomized controlled trial. J Gerontol a Biol Sci Med Sci 60: 187-194.
- Robertson MC, Campbell AJ, Gardner MM, Devlin N (2002) Preventing injuries in older people by preventing falls: A meta-analysis of individual-level data. J Am Geriatr Soc 50: 905-911.
-
Sciandrone Gaetano Giuseppe*. Management and Prevention of Fall Risk: A Literature Review. Iris J of Nur & Car. 5(4): 2025. IJNC.MS.ID.000618.
-
Nurse-fall, Risk-prevention, World Health Organization, Traumatic death, Falls prevention education (FPE)
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






