 Short Communication
Short Communication
Using the Electronic Medical Record to Identify At-Risk Older Adults in the Emergency Department Saves Valuable Nursing Time and Aids Evaluations and Referrals
Stephen Meldon1*, Renee Tyska2, Ashley Hawkins1 and Saket Saxena3
1Emergency Services, Cleveland Clinic, Cleveland, OH, USA
2West Health Institute, La Jolla, CA, USA
3Center for Geriatric Medicine, Cleveland Clinic, Cleveland, OH, USA
Stephen Meldon MD, Emergency Services, Cleveland Clinic, USA
Received Date:March 26, 2024; Published Date:April 04, 20243
Abstract
Older adults have the highest emergency department (ED) use and are vulnerable to poor outcomes, such as repeat ED visits, hospitalization, mental status and functional decline, and nursing home placement.
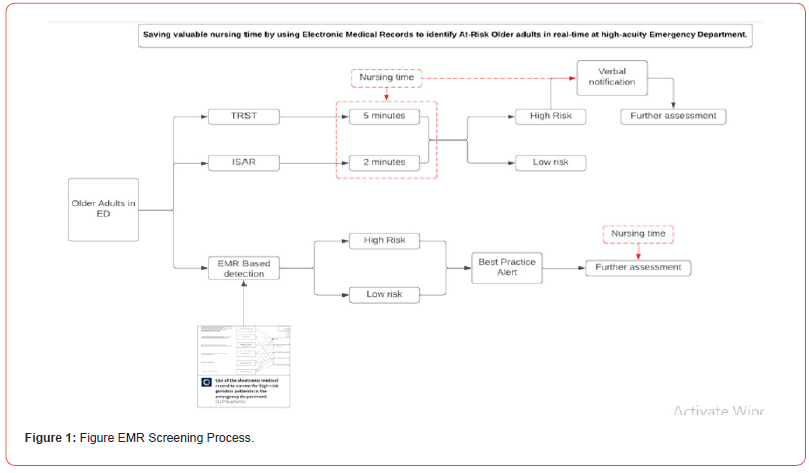
Identifying high risk older patients, followed by a more comprehensive geriatric assessment with interventions directed at improving outcomes, is a priority for Geriatric ED (GED) programs nationwide. However, identifying patients most at risk for these outcomes in a high-volume ED is difficult. Commonly used risk-screening tools, require manual administration and scoring by trained nurses or other caregivers. While geriatric risk screening is considered best practice, the current nurse triage workflow is overburdened, which makes including additional screenings a barrier.
We developed a novel, automated Electronic Medical Record (EMR) risk screen to identify these high-risk older patients and notify their ED caregivers, thus freeing up valuable nursing triage and evaluation time.
Given current and projected workforce shortages, utilizing technology to improve efficiency in workflow allows ED nurses to provide safe, quality care without bearing the brunt of additional work. Allowing the EMR to automatically screen for high-risk geriatric patients can save nursing time and effort and allow nurses to focus on other care priorities.
Keywords: Geriatric screening; Electronic medical record; Emergency department
Abbreviations: ED, ISAR, TRST, EMR
Introduction
Older adults have the highest emergency department (ED) use and are most vulnerable to poor outcomes, such as repeat ED visits, prolonged hospitalization, worsening mental status, functional decline, and nursing home placement. Identifying older patients at risk for these poor outcomes in a high-acuity, high-volume ED is difficult. We developed an automated Electronic Medical Record (EMR) risk screen to identify these patients and notify their ED caregivers, thus freeing up valuable nursing triage and evaluation time.
The Problem
The commonly used risk-screening tools, ISAR (Identification of Seniors at Risk) [1] and TRST (Triage Risk Screening Tool) [2] require manual administration and scoring by trained nurses or other caregivers, followed by communication to the treating team members to address previously unidentified medical/ social issues (cognition, mobility, polypharmacy, social determinants of health).
There are multiple inherent challenges to this approach.
Availability and Access- Having the availability of trained nurses or other ancillary personnel in the ED to perform such assessments in the ED on all older adults.
Amount of time – the ISAR screening tool, which is the most widely adopted, takes two to five minutes to perform and document findings [3].
Aggregate score – The above tests result in an aggregate score – patients are categorized as high/low risk for poor outcomes- which does not inform treating team members about which aspect of care delivery to focus on.
Identifying such patients to allow for a more comprehensive geriatric assessment and to improve outcomes, is a priority for the Geriatric ED (GED) program at Cleveland Clinic and similar GED programs nationwide.
A Solution
EMRs, which have wide-spread adoption in EDs nationally, can automatically screen for high-risk geriatric patient characteristics saving nursing time and effort and allowing nursing to focus on other care priorities. This screening can also drive geriatric assessments and referrals. Importantly, use of the EMR may also limit implicit caregiver bias and improve equity in health care evaluations and referrals.
We cross-walked the high-risk characteristics from these commonly used screening tools and developed a similar list of discrete elements commonly documented in the EMR [4]. Availability and use of content experts and consensus were critical to this process. Polypharmacy, dementia, fall history and frequent ED visits were included. Early involvement and buy-in from the Cleveland Clinic Clinical Systems Operations (EMR ITD) team who would be tasked with developing the logic for the EMR data search and the automated provider banner notification build was a key early step.
Key barriers included prioritization amongst several other EMR projects. Of note, since EMR updates occur in-house, there were no additional charge backs to the GED. Additional barriers included nursing and provider education reviewing the clinical importance of the high-risk geriatric criteria chosen, and review of the EMR high-risk banner and use of its imbedded geriatric consult link.
Results
Since this process went live in 2019, 74,198 older adults (age 65yr+) have been screened in the Cleveland Clinic Main Campus Geriatric ED. At the minimum of two-minutes per manual ISAR screen, automated EMR screening has saved 148,396 nursing minutes or almost 2,500 nursing hours, with an estimated equivalent cost savings of $87,500.
EMR-based identification of at-risk older adults in the ED has resulted in an increase in increased mobility and functional assessments and improved care coordination by the multidisciplinary geriatric ED team at Cleveland Clinic.
EMR-related identification, provider notification, and subsequent consult for assessment by the Geriatric ED team have resulted in 2,903 Comprehensive Geriatric Assessments; approximately 60% of these evaluations occurred in the Geriatric Care Unit.
Our initial evaluation shows that targeted comprehensive geriatric assessments initiated by the EMR screen have reduced potentially avoidable hospital admissions by 42% in older ED patients and 73% in the ED-based observation geriatric care unit [5].
In addition, EMR notification to ED providers of high-risk status is now being used to drive referrals of discharged patients to Cleveland Clinic Successful Aging Clinics (geriatric outpatient follow-up visits). Over a recent six-month period, this has resulted in 153 appointments or 26 per month.
Caregiver satisfaction, anecdotally, has been uniformly positive.
Discussion
Use of the EMR to automate previously manual screening for high-risk geriatric ED patients is feasible. Importantly, it is scalable and can be implemented across large healthcare systems.
It is also easily updatable and can be iterated to utilize other patient characteristics of interest (such as social determinants of health). As an example, we adjusted the number of criteria for highrisk designation to try and improve specificity and limit banner alert fatigue. Future development could include use of natural language processing (NLP) and AI to search for unstructured EMR data.
With current and projected healthcare workforce shortages [6], tech solutions, such as this, can optimize healthcare resources and reduce staff workloads in a way that can improve the patient and staff experience, and work within the existing infrastructure and workflow of the healthcare professionals using these technologies. Importantly, such healthcare digital technologies need to provide insights that are actionable (such as better allocation of resources), reduce workload pressures and deliver the best possible care [7].
Use of the EMR may also limit implicit bias by eliminating the subjective determination as to which patients receive these screenings and may improve equity in health care evaluations and referrals.
Conclusion
Cleveland Clinic Geriatric ED program has taken a unique approach to address the problems of triage screening by using the Electronic Medical Record (EMR) to screen for high-risk older patients. This time saving has allowed our ED nurses to focus instead on triage screening for delirium. EMR screening notification is also used to direct additional targeted comprehensive geriatric assessments by the geriatric ED team, resulting in improved outcomes, better care coordination and increased appropriate outpatient clinic referrals.
Acknowledgement
West Health Institute has provided funding to collaborate with the Cleveland Clinic on improving care for older adults and examining Geriatric ED outcomes. We also thank McKinsey Muir and Molly Gourash for their assistance with this program.
Conflict of Interest
None.
References
- Identification of Seniors At Risk (ISAR): An Emergency Department Screening Tool to Identify Older Adults at Risk of Adverse Functional Outcomes. The ISAR Screening Tool Manual V2. McCusker J.
- Meldon SW, Mion LC, Palmer RM, Drew BL, Connor JT, et al. (2003) A Brief Risk Stratification Tool to Predict Repeat ED Visits and Hospitalizations in Older Patients Discharged from the Emergency Department. Acad Emerg Med 10: 224-232.
- Salvi F, Morichi V, Grilli A, Spazzafumo L, Giorgi R, et al. (2009) Predictive validity of the Identification of Seniors At Risk (ISAR) screening tool in elderly patients presenting to two Italian Emergency Departments. Aging Clin. Exp. Res 21: 69–75.
- Saxena S, Meldon S, Hashmi AZ, Muir M, Ruwe J (2023) Use of the Electronic Medical Record to screen for high-risk geriatric patients in the Emergency Department. JAMIA Open 6(2).
- Meldon S, Saxena S, Hashmi A, Masciarelli McFarland A, Muir M, et al. (2024) The Impact of Geriatric Evaluations on Hospital Admission Rates for Older Emergency Department and Emergency Department Observation Unit Patients. WestJEM 25(1): 86-93.
- AHA Data Brief: Health Care Workforce Challenges Threaten Hospitals Ability to Care for Patients. https://www.aha.org/system/files/media/file/2021/11/data-brief-health-care-workforce-challenges-threaten-hospitals-ability-to-care-for-patients.pdf (accessed Dec 8, 2023)
- Jakobs R. How tech can tackle workloads and staff shortages to optimize healthcare. World Economic Forum Davos 2023. https://www.weforum.org/agenda/2023/01/healthcare-workloads-and-staff-shortages-davos23/ (accessed Dec 8, 2023)
-
Stephen Meldon*, Renee Tyska, Ashley Hawkins and Saket Saxena. Using the Electronic Medical Record to Identify At-Risk Older Adults in the Emergency Department Saves Valuable Nursing Time and Aids Evaluations and Referrals. Iris J of Nur & Car. 4(6): 2024. IJNC.MS.ID.000599.
-
Geriatric screening, Electronic medical record, Emergency department
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






