 Review Article
Review Article
Traumatic Spinal Cord Injuries: The Nature of the Beast and Principles of its Management
WS El Masri*
Hon. Professor of Spinal Cord Injury, Keele University, UK Emeritus Consultant Surgeon in Spinal Injuries Midland Centre for Spinal Injuries RJAH Orthopedic Hospital, Oswesty Past President International Spinal Cord Society 2008-2010
WS El Masri, Hon. Professor of Spinal Cord Injury, Keele University, UK
Received Date:April 22, 2023; Published Date:May 12, 2023
Introduction
Traumatic spinal cord injuries (TSCI) are life threatening and life changing events. Fortunately, the incidence of Spinal Cord Injuries is one of the smallest of all medical conditions ranging between 10 to 50 patients/ million population /year. Prior to the second world war the majority of the patients died from complications that developed in the systemic effects of cord damage. With expert simultaneous management of the injured spine together with all the medical and non-medical effects of cord damage from the early hours of injury the impact of a spinal cord injury can be minimized and a significant number of patients with incomplete spinal cord injuries recover motor power to walk again without surgical intervention on the injured spine. The majority of patients with complete cord damage do not recover the ability to walk irrespective of the method of management of the injured spine. With expert care of the inured spine and all the effects of cord damage however, all complications of cord damage can be prevented or diagnosed and treated early to prevent morbidity and mortality as well as prevent further neurological deterioration by mechanical and non-mechanical factors [1-5].
An injury to the spinal cord results in a multi-system physiological impairment and malfunction that includes the spinal cord. An injured, physiologically impaired, and unstable spinal cord is vulnerable to a variety of non-mechanical complications that can easily develop in these patients. Significant hypotension, hypertension, hypoxia, hypothermia, generalized sepsis, electrolytes imbalance have been observed to further destabilize the injured cord causing manifest neurological deterioration, prevent recovery or delay neurological recovery.
Delays in the diagnoses of complications due to the lack or impairment of sensation and inability of the patient to present the expected symptoms and signs to clinicians are not uncommon. This is due to the rarity of the condition and the little exposure of the majority of clinicians to the management of these patients without training in dedicated Services to the management of spinal cord injuries [6-10].
Currently, unfortunately the resources to manage the medical and non-medical effects of the majority of patients with spinal cord injuries are inadequate and diminishing. Consequently, the devastating wide range of medical, psychological, social, emotional, financial, vocational, environmental, and economic consequences are often poorly managed. The poor management of the medical effects result in the development of a wide range of avoidable complications that affect the patients health and precipitate a vicious circle of added psycho-social and economic burden to patients and all those related to them [11-15].
Successful management of patients with Spinal Cord Injuries requires: an understanding of the patho-physiological changes that occur in the various systems of the body and an infra structure of a knowledgeable, well trained, experienced and well-coordinated multidisciplinary team of health care professionals who treat the patient in an environment that facilitates the complex management of the condition and reduce the impact of the effects of cord damage on patients and those who care for them.
With expert initial management and ongoing surveillance, care and support, patients with spinal cord injuries can lead healthy, fulfilling, productive, dignified, and enjoyable lives and contribute to their community and society at large [16-20].
Effects and Special Characteristics of Spinal Cord Injury (SCI)
SCI causes a generalized physiological impairment and multi system malfunctions as well as psychological, social, emotional, matrimonial, financial, vocational, environmental, and economic problems to the individual. Those individuals related to the patient are at least similarly affected by the non-medical effects of the injury. Due to the loss of autoregulatory mechanisms, loss of blood brain barrier and due to several cell membrane cellular and metabolic disturbance, the Injured Spinal Cord (SC) is Physiologically impaired and Unstable. Unlike the undamaged spinal cord, the injured SC is vulnerable to complications outside of the spinal canal. Hypoxia, hypotension, sepsis can easily occur and can result in further neurological deterioration, delay or lack of recovery.
The function of the various systems of the body depends on the reflex activity of the spinal cord segments distal to the lesion as well as the intrinsic property of the individual body system. Changes in level of reflex activity of the injured SC is likely to occur during the patient’s life and affect the functioning of the various systems of the body. During the first six to twelve weeks from injury i.e., the transitional phase between the absence and the gradual return of the sympathetic and spinal reflexes the functioning of the almost all systems of the body affected by the neurological impairment/ loss undergo changes that necessitate close monitoring and recalibration of management of the various systems of the body to prevent complications, mitigate further impairment and minimize disability [21-25].
The reflex activity of the isolated spinal cord continues to vary throughout a patient’s life with effect on the reflex functioning of the different systems of the body. A cold environment for example can increase reflex activity causing excess spasticity. Any pathology below the level of injury is likely to increase the afferent stimuli the spinal cord and result in excess reflex activity spasticity with implications on function of the various systems of the body. The sensory impairment or loss below the injury presents diagnostic challenges to the clinician. Conventional symptoms and signs of pathology are absent. This can result in delay of diagnosis with unpleasant consequences. Each system malfunction caused by spinal cord injury is a source of multiple disabilities and a potential source of a wide variety and range of complications. For example, impairment of bladder functions can result in urinary incontinence and urinary infections, calculi, renal damage, and renal failure.
Considering the number of disabilities and potential complications from the various system impairments, one can easily appreciate the magnitude of the burden to the patient, partner carers, and the team responsible for the treatment, rehabilitation, and education of the patient.
When a complication develops, the interruption of the higher coordinating and moderating functions of the brain at the site of the spinal cord injury usually results in multiple and/or cascading intersystem effects that are rarely seen in other conditions. These are seldom easy to manage. For example, an anal fissure, while painless in a tetraplegic or high paraplegic patient can nevertheless cause excess spasticity which in turn may cause a fall and fracture of a long bone. Alternatively excess spasticity involving the pelvic floor muscles can result in urinary retention, autonomic dysreflexia and possibly some cerebra-vascular accident [26-30].
Unfortunately, Complications will invariably develop in Spinal Cord Injury patients if management is less than adequate. Pressure sores, respiratory infections, contractures of muscles are some such examples. Death and complications can also easily occur because of poor understanding of the physiology of the spinal man/ woman. Death from respiratory failure in patients with injuries below C5, death from over hydration pulmonary embolism or from hypothermia during the stage of spinal shock, are examples of preventable complications which can lead to death.
Almost all complications following SCI are preventable or can be minimized. The non-medical effects of spinal cord injuries are equally devastating to patients and family members. It must be appreciated that the psychological, social, and medical effects of a spinal cord injury can easily affect each other’s directly and/or indirectly.
For example, if a patient who is psychologically depressed or in a depressive mood to neglect pressure relief, this is likely to result in the development of one or more pressure sores, which may due to poor sight and smell cause social and matrimonial problems.
Fortunately, the incidence of traumatic spinal cord injury is the lowest of all major trauma. The incidence varies between countries ranging between 10-50 per million head of population per year. A general hospital serving a population of 250,000 is likely to receive three to twelve newly injured patients per year. With such relatively small numbers of patients it is rather difficult to develop the expertise of a multi-disciplinary team of health care professionals to manage such complex conditions in general hospitals. The management of SCI patients is therefore easier, safer and more cost effective to conduct in Spinal Injury Centres equipped with the infrastructure and expertise of adequately trained knowledgeable and competent health care professionals [31-35].
Furthermore, supervised peer support is easier to offer in Spinal injury centres where a large number of patients are treated. This is of incalculable value in the facilitation of management, psychological support and not infrequently vocational re engagement of the patient.
Principles of Active Physiological Conservative Management (APCM) of TSCI
It becomes readily evident to those who have been involved with the management of a SCI patient that the wide range of effects and the complexity of the condition require a team of clinicians from the medical and allied professions. It is essential that the members of such a team be knowledgeable about the condition, well trained, well-coordinated and prepared to provide a “Patient Centered Service” perhaps sacrificing in the process some of their own “Professional & Personal Ambitions” [36-40].
The aims of Holistic Simultaneous APCM of all the effects of
acute traumatic cord damage in Specialized Centres are to:
• Prevent death
• Mitigate the need for admission to Intensive Care and
Ventilation of patients with a cord injury below C5 with no
previous history of chronic respiratory problems and no life
threatening associated injuries
• Contain the Biomechanical Instability of the injured spine
until bony healing to ensure the shortest natural fusion that
results in a painless full range of movement of the spine which
is necessary for the patient to achieve maximum independence
in and outside a wheelchair.
• Prevent and/or minimize complications to mitigate
or minimize further impairment of body systems, minimize
disability, and achieve maximum neurological recovery. This is
achieved by constantly reviewing, monitoring, and recalibrating
the management of the various systems of the body affected by
the paralysis according to level of reflex activity and functioning
until reflex activity returns and stabilizes.
• Frequently Monitor Neurology, Vital Capacity, Blood
Pressure, Oximetry throughout the acute and subacute stages.
• Ensure by close monitoring that when patients are
mobilized the is no neurological loss associated with a drop
of Blood pressure, Vital Capacity or Low levels of Oxygen
saturation.
• Manage to treat and retrain all the systems of the body to
function safely and conveniently to patients and/or carers.
• Ensure a locomotor program of rehabilitation that
maximizes independence within the level and density of cord
damage and the disability.
• Equip the patient with adequate information about the
condition, self-care, self-confidence, and skills to re-engage
socially.
• Assessing the patient’s cognitive functions helps in the
setting of goals of treatment, according to his/her capability
in engaging in a demanding rehabilitation program as well as
determine the extra need for care support or supervision.
• Assess the ability of the patient to resume previous
employment.
• If necessary, ensure retraining the patient vocationally if
unable to resume previous employment.
• Educate the patient in the condition as well as in the
of prevention of complications prior to discharge to ensure
maintenance of health and minimize need for re-hospitalization.
• Advise and assist in “Soft Landing” a healthy patient in
own adapted environment.
• If your assessment determines that following discharge
from hospital carers will be required by the patient, ensure
they are well aware of the potential long-term complications
and trained in the methods of their prevention.
• Maintain the health and independence of the patient
following discharge by offering regular follow up reviews to
detect and treat complications at an early stage and prior to the
development of morbidity or mortality.
• Provide timely support during crises.
Such comprehensive management enables patients to live
healthy, reasonably happy, productive lives as well as re engage and
compete in many spheres of life.
Because of the impaired physiology and/or sensory impairment/loss the principles of management of most conditions in TSCI patients differ from the principles of management of the same condition in neurologically intact individuals [41-45].
Conclusion
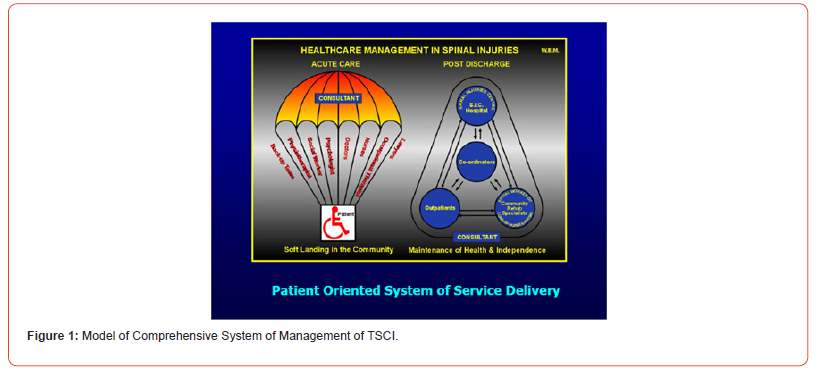
A Comprehensive, Patient Centered, Goal Oriented, Well Coordinated Service in the acute, subacute and rehabilitation stages together with an Ongoing Surveillance Service by the team that has provided the initial management and is familiar to the patient is paramount to enable individuals with TSCI to readjust, cope, regain self-confidence and control, engage, participate, contribute and compete in many spheres of life as well as remain healthy and out of hospitals for most of their remaining lives (Figure 1).
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Guttmann L (1976) Spinal cord injuries: comprehensive management and research, 1st ed. Oxford, UK: Blackwell, vol 1 1973 2nd ed. Oxford, UK: Blackwell vol 2.
- Wagih El Masri(y), Michael Barnes (2020) Spinal cord injury and its management - Oxford Textbook of Medicine (6edn), Chapter 24.13.2 Published in print and online.
- Frankel HL, Hancock DO, Hyslop G, Melzack J, Michaelis LS, et al. The value of postural reduction in Initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969-70; 7: 179-192.
- S Katoh, W S El Masry (1994) Neurological recovery after conservative treatment of the cervical spine. JBJS 76(2): 225-8.
- El Masri(y) WS, Jaffray DJ (1992) Recent developments in the management of injuries of the cervical spine. In: Frankel HL, ed. Spinal cord trauma. Amsterdam: Elsevier 55-73
- FolmanY, El Masri(y) WS (1989) Spinal cord injury: prognostic indicators. Injury 20: 92-93.
- Poynton AR, O Farrell DA, Shannon F, Murray P, McManus F, et al. (1997) Sparing of sensation to pin prick predicts recovery of a motor segment after injury to the spinal cord. J Bone Joint Surg Br 79: 952-54.
- S Katoh, W S El Masry (1995) Motor Recovery of Patients Presenting with Motor Paralysis & Sensory Sparing following Cervical Spinal Cord Injuries. Praplegia 33: 506-509.
- El Masry (1993) WS Editorial - physiological instability of the injured spinal cord. Paraplegia 31: 273-5.
- Carvel JE, Grundy DJ (1994) Complications of spinal surgery in acute spinal cord injury. Paraplegia 32: Illis389-395.
- El Masry WS (2006) Traumatic spinal cord injury: the relationship between pathology and clinical implications. Trauma 8: 29-46.
- Wagih El Masri (2010) Management of Traumatic Spinal Cord Injuries: current standard of care revisited. ACNR 10(1): 37- 40.
- W El Masri, Naveen Kumar (2017) Active physiological conservative management in traumatic spinal cord injuries an evidence-based approach.
- WS El MASRY. Clinical and Radiological assessment of patients with spinal cord and cauda equina injuries: Advances in Rehabilitation (aggiornamenti in Medicina Riabilitativa): Views and Perspectives, Chapter 4, 16: p79 -105.
- (2004) Editors: Barat, M, Franchignoni F Maugeri Foundation Books, Pavia, Italy.
- El Masry WS, Osman AE (2006) Clinical perspectives on spinal injuries. In: Cassar-Pullicino V, Imhof H. Spinal trauma: an imaging approach. New York, Thieme Medical Chapter 1, p. 1-14.
- Tator CH, Duncan EG, Edmonds VE, Lapczac LI, Andrews DF (1987) Comparison of surgical and conservative management of 208 patients with acute spinal cord injury. Can J Neurol Sci 14(1): 60-9.
- El Masri(y) WS, Meerkotter DV (1992) Early decompression of the spinal cord following injury: arguments for and against. In: Illis LS, ed. Spinal cord dysfunction vol II intervention and treatment. Oxford: Oxford University Press.
- J Mumford, JN Weinstein, KF Spratt, VK Goel (1993) Thoracolumbar burst fractures. The clinical efficacy and outcome of non-operative management. Spine (Phila Pa 1976) 18(8): 955-70.
- El Masri(y) WS, Katoh S, Khan A (1993) Reflections on the neurological significance of bony canal encroachment following traumatic injury of the spine in patients with Frankel C D and E presentation. J Neurotrauma 10: 70.
- S Katoh, W S el Masry, D Jaffray, I W McCall, SM Eisenstein, et al. (1996) Neurological outcome in conservatively treated patients with incomplete closed traumatic cervical spinal cord injuries. Spine 21(20): 2345-51.
- Rosenberg N, Lenger R, Weisz I, Stein H (1997) Neurological deficit in a consecutive series of vertebral fractures patients with bony fragments within the spinal canal. Spinal Cord 35: 92-95.
- De Klerk LW, Fontijne WP, Stijnen T, Braakman R, Tanghe HL, et al. (1998) Spontaneous remodelling of the spinal canal after conservative management of thoracolumbar burst fractures. Spine (Phila Pa 1976) 23(9): 1057-60.
- Boerger TO, Limb D, Dickson RA (2000) Does canal clearance affect neurological outcome after thoracolumbar burst fractures. J Bone Joint Surg Br 82(5): 629-35.
- Eberl R, Kaminski A, Müller EJ, Muhr G (2003) Importance of the cross-sectional area of the spinal canal in thoracolumbar and lumbar fractures. Is there any correlation between the degree of stenosis and neurological deficit? Orthopade 32(10): 859-64.
- Dai LY, Wang XY, Jiang LS (2007) Neurologic recovery from thoracolumbar burst fractures: is it predicted by the amount of initial canal encroachment and kyphotic deformity? Surg Neurol 67(3): 232-7; discussion 238.
- Bedrook GM, T Sakai (1982) A review of cervical spine injuries with neurological dysfunction. Para-plegia 20: 321-333.
- Wilmot CB, Hall KM (1986) Evaluation of the acute management of tetraplegia: conservative versus surgical treatment. Paraplegia 24: 148-153.
- JS Keene, SP Fischer, R Vanderby Jr, DS Drummond, PA Turski (1989) Significance of acute posttraumatic bony encroachment of the neural canal. Spine (Phila Pa 1976) 14(8): 799-802.
- Braakman R, Fontijne WP, Zeegers R, Steenbeek JR, Tanghe HL (1991) Neurological deficit in injuries of the thoracic and lumbar spine. A consecutive series of 70 patients. Acta Neurochir (Wien) 111(1-2): 11-7.
- Murphy KP, Opitz JL et al. (1990) Cervical fractures and spinal cord injury: Outcome of surgical and non-surgical management. Mayo Clin Proc 65: 949-959.
- Fidler MW (1988) Re-modelling of the spinal canal after burst fracture: A prospective study of two cases. J Bone Joint Surg 70B: 730-32.
- MG Fehlings, RG Perrin (2005) The role and timing of early decompression for cervical spinal cord injury: update with a review of recent clinical evidence. Injury 36 Suppl 2: B13-26.
- Fehlings MG, Vaccaro A, Wilson JR (2012) Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS ONE 7(2): e32037.
- Van Middendorp JJ, Hosman AJ, Doi SA (2013) The effects of the timing of spinal surgery after traumatic spinal cord injury: a systematic review and meta-analysis. J Neurotrauma 30: 1781-1794.
- Brennan P (2012) STASCIS results on timing in spinal injury. Surgeons’ news, The Royal College of Surgeons of Edinburgh. p.6.
- Kwon BK, Curt A, Belanger LM (2009) Intrathecal pressure monitoring and cerebrospinal fluid drainage in acute spinal cord injury: a prospective randomized trial. J Neurosurg Spine 10: 181-193.
- Mathias CJ, Bannister R (2002) Investigation of autonomic disorders. In: Mathias CJ, Bannister R (eds) Autonomic Failure. A Textbook of Clinical Disorders of the Autonomic Nervous System, 4th edn. Oxford: Oxford Univ. Press pp. 169 – 95.
- ML Marcus, DD Heistad, JC Ehrhardt, FM Abboud (1977) Circulation Research Regulation of total and regional spinal cord blood flow. Circulation Research 41: 128-134.
- Tator, J Neurosurg (1991) Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 75(1): 15-26
- P Cariga, S Ahmed, CJ Mathias, BP Gardner (2002) The prevalence and association of neck (coat-hanger) pain and orthostatic (postural) hypotension in human spinal cord injury Spinal Cord. 40: 77-82.
- Morgan MDL, Silver JR and Williams SJ. The respiratory system of the spinal cord patient. 12 Trauma 0(0) In: Bloch RF, Basbaum M (eds) Management of spinal cord injury. Baltimore, MD: Williams and Wilkins. pp. 78-117
- Cameron GS, Scott JW, Jousse AT, et al. (1955) Diaphragmatic respiration in the quadriplegic patient and the effect of position on his vital capacity. Ann Surg 141: 451-456.
- Baydur A1, Adkins RH, Milic Emili J (2001) Lung mechanics in individuals with spinal cord injury: effects of injury level and posture. J Appl Physiol 90: 405-411.
- Valentina Alvisi, Elisabetta Marangoni, Silvia Zannoli, Mariella Uneddu, Riccardo Uggento, et al. (2012) Pulmonary function and expiratory flow limitation in acute cervical spinal cord injury. Arch Phys Med Rehabil 93: 1950-1956.
-
WS El Masri*. Traumatic Spinal Cord Injuries: The Nature of the Beast and Principles of its Management. Iris J of Nur & Car. 4(3): 2023. IJNC.MS.ID.000587.
-
Spinal cord, Injuries, Spinal injuries, Traumatic spinal cord injuries, Spine, Neurological deterioration, Significant hypotension, Hypoxia
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






