 Mini Review
Mini Review
The Effectiveness of the Repositioning and from the Assessment of the State Nutritional in Prevention and in the Treatment from the Injuries from Pressure
Sciandrone Gaetano Giuseppe*
Nurse at the Pulmonology Unit, IRCCS San Matteo Foundation Pavia 27100 (PV), Italy
Sciandrone Gaetano Giuseppe, Nurse at the Pulmonology Unit, IRCCS San Matteo Foundation Pavia 27100 (PV), Italy
Received Date:July 15, 2025; Published Date:July 18, 2025
Abstract
The prevalence of pressure ulcers in the population represents a significant health problem. Prevention and treatment of pressure ulcers are among the most challenging issues facing healthcare professionals.
Objective: Identify whether the techniques of repositioning and assessment of the patient’s nutritional status are effective in the prevention and treatment of pressure injuries.
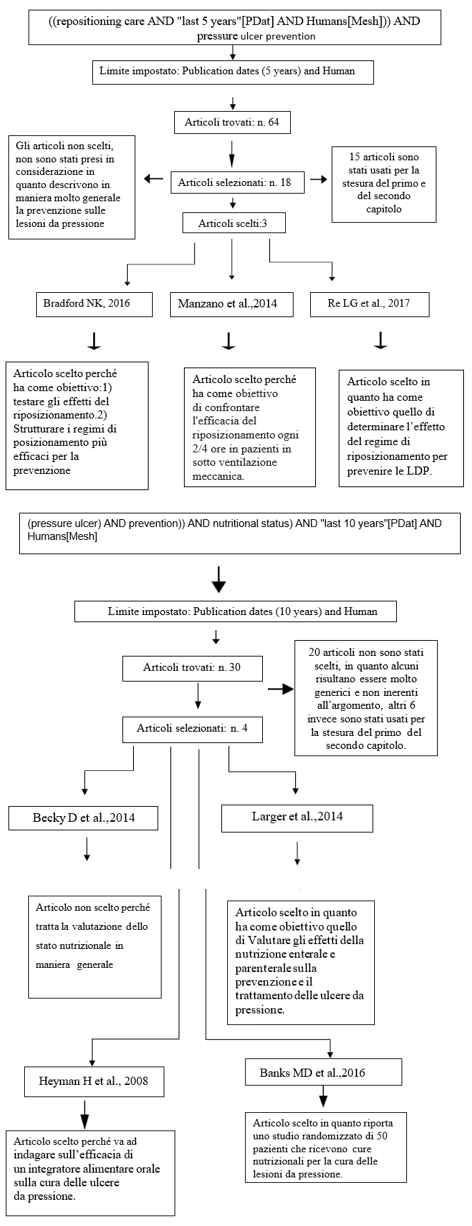
Method: It was conducted using the PIO methodology. The following filter was used to search for articles:
• Humans (Adults with age of majority to 65 years)
• Research Of articles on repositioning.
• Nutritional status assessment
I am were found:
• For the assessment of nutritional status, 30 articles were selected, of which 4 were selected. I subsequently excluded one because it deals with
the assessment of nutritional status in a general manner.
• For patient repositioning, 64 articles were selected, 18 of which were then chosen because 3 articles answered the research question.
Conclusions: From the analysis of the articles, it is highlighted that to prevent/reduce and treat the onset of pressure ulcers it is important to:
• Structuring alternative and effective repositioning regimens, in particular respecting the 2/3-hour times, significantly reduces the risk of
pressure ulcers developing.
• There is no clear evidence for nutritional interventions for prevention or treatment of benefit, but their consideration from the assessment
For Everything is fine individual at high risk of developing a pressure ulcer is essential.
Keywords:Pressure ulcer prevention; Nutritional status; Repositioning dear
Introduction
In the current healthcare context, one of the most challenging challenges facing professionals. The main challenge healthcare workers constantly face is the prevention of one of the recurring and most feared consequences of aging and bed rest: pressure ulcers. A pressure ulcer is a lesion localized on a bony prominence, caused by pressure combined with shear forces (EPUAP et al, 2016). The presence of pressure ulcers is a health problem of considerable importance: its spread is demonstrated by a constantly growing prevalence due to of aging and the health problem that forces people
to remain immobile. The prevention and treatment of pressure ulcers is a major challenge both in hospitals and outpatient settings, requiring the management of human and material resources.
Definition And Classification
“A pressure ulcer is a localized injury to the skin and/or underlying tissue usually located over a bony prominence, as a result of pressure or pressure in combination with shear forces” (EPUAP et al, 2016).
Staging of pressure ulcers is based on their depth and the possible involvement of specific structures. The most recent and accepted staging approach, proposed by the American and European groups (NPUAP/EPUAP), is now also supported by the Pan-Asian group (PPPIA), and involves subdivision into four stages.
Stage I: Erythema Not bleachable
Skin intact with redness on a prominence bone. The area can to be painful, solid, soft, warmer or colder.
Stage II: Loss Cutaneous to Thickness Partial
There is partial loss of dermis that appears as a reddish-pink ulcer. It may also be an intact or open/ruptured serum-filled blister. This Stage should not be used to describe skin lacerations, burns, perineal dermatitis, maceration, or excoriations.
Stadium III: Loss Cutaneous to Total Thickness
Full-thickness tissue loss. Subcutaneous fat may be visible, but bones, tendons, or muscles are not visible. The depth of Stage III pressure ulcers varies depending on the anatomical location.
Stadium IV: Loss Of Tissue to Total Thickness
Loss of tissue Total with exposed bone, tendon, or muscle. Eschar and devitalized tissue may be present in some parts of the wound bed. The depth of Stage IV pressure ulcers varies depending on the anatomical location.
Stage V or unclassifiable:
When the exact stage cannot be determined due to eschar or slough covering the lesion or when deep tissue damage is suspected but is not visible.
The body parts more prone to the risk of formation of injuries from pressure They vary depending on whether the individual is lying down or sitting. In the case of a bedridden individual, the areas most affected are: sacrum, heels, elbows, and shoulder.
If the person is frequently in an armchair or wheelchair, the area’s most at risk are: buttocks, heels and back. Early identification from the people to risk of develop LdP and their timely mass in act Of Interventions is essential for prevention. Prevention and treatment of pressure ulcers require the necessary knowledge and culture to guide the operator in choosing and using appropriate methods and tools.
Risk factors that increase the chance of developing a pressure
injury are:
• Lodging
• Immobility
• Incontinence urinary and faecal
• Malnutrition
• Reduced mental clarity
• Reduced/altered sensory perception
One of the first objectives that the professional must follow
when taking charge of the person and their assessment clinic.
This assessment and focused at the identification of the factors of
risk for the development of injuries from pressure: Yes, defines to
I risk it person who, due to a pathology, presents general factors,
such as hypomobility or reduced motor capacity, or local factors,
which expose them to a greater risk of developing pressure ulcers.
Particular attention must be paid to identifying the main local risk
factors, such as friction, slippage, humidity, blood hypoperfusion,
edema, etc., and to the following pathologies that can promote the
onset and/or slow their progression. healing such as:
• Illnesses cardiovascular
• Diabetes
• Pathologies oncological
• Malnutrition
• Immunodeficiencies
• Peripheral vascular disease
• Fever
• Infections concomitants
At the time of taking charge of the subject, it is also necessary to have a previous medical history to understand whether the patient is at risk of developing pressure ulcers or not. The clinical history must understand nutritional status assessment.
Instruments
Assessment scales are tools that allow you to objectively identify the risk index of developing pressure ulcers.
The use of a structured tool that has been tested for validity and reliability, such as the Braden Scale for Predicting Pressure Sore Risk, the Norton Pressure Sore Risk Assessment Scale, and the Water low Pressure Ulcer Risk Assessment Tool, is recommended (Level of evidence III: RNAO 2011 supplement).
The main lines Guide international I am agreeing in the
recommend to this I aim for the Braden scale. In some clinical
situations, risk assessment scales may present limitations; in fact,
a subject apparently not at risk could develop pressure ulcers if
wearing orthopaedic supports (casts, splints, etc.), or if wearing
medical devices (NGS, bladder catheter, collar, etc.). Braden In the
2001 describes a protocol of treatment structured for levels of risk,
based on the results of the Braden Scale for Predicting Pressure
Sore Risk:
• For low-risk individuals (15-18), the prevention plan includes
a mobilization program, for adequate protection of the heels,
management of moisture, nutrition, friction and shear forces
and the use of support surfaces to reduce pressure when the
patient is confined to a bed or chair.
• For individuals at moderate risk (13-14), interventions
adopted in case of mild risk should be continuous, with the
addition of a 30° lateral rotation program.
• For high-risk individuals (10-12), rotation frequency and the
use of memory foam cushions to facilitate 30° lateral rotations
should be supplemented with small weight transfers.
• For individuals at very high risk (<9), the plan includes
continuation of previous prophylactic interventions plus the
use of an air mattress overlay.
Materials and Methods
After have duct preliminary research in literature tertiary with the scope Of To outline the problem of pressure ulcers in patients with hypokinetic syndrome and its prevention, I tried to understand the effectiveness of the two procedures.
I have constructed the following research question: “Are patient repositioning and nutritional status assessment effective methods for prevention?” and for the treatment of pressure ulcers?”
I used the PIO methodology which allowed me to identify the
keywords and subsequently the articles related to the chosen topic:
• P (Population and Problem): Elderly people at risk of
developing injury from pressure
• I (Intervention): Repositioning and balanced diet to prevent
the onset of pressure ulcers;
• O (Outcomes or themes): Effectiveness of the repositioning
and diet balanced for the prevention and treatment of pressure
ulcers.
PubMed database, through three search strings and use of operators Booleans AND OR Like this from combine and/or include in I can combine multiple concepts in the same search, obtaining results that contain related terms at the same time or both. Furthermore, to narrow and target the search, I used MeSH (Medical Subject Headings).
The keywords used were: pressure ulcer prevention; nutritional status, repositioning care.
I have conducted two Search types:
• Studies randomized That confirm or less the effectiveness of
the repositioning of the patient in the prevention of pressure
ulcers.
• Studies randomized trials that confirm or deny the
effectiveness of nutritional status assessment in the prevention
and treatment of pressure ulcers.
Strings of Research and Tables
The strings of research with the results obtained and the criteria adopted I am the following:
Discussions And Conclusion
Posture changes should be performed every 2-3 hours, taking into account the patient’s comfort, skin condition, and general health. (Bellingeri A., The handbook for the management of skin lesions, 2017.)
In addition to these two aspects, certain areas of the body must be taken into account to ensure they are not subjected to continuous pressure for a long time, such as the heel area which, despite the change in posture, can remain in contact with the surface for long periods and can develop pressure sores.
is recommended if the patient is uncooperative to avoid creating friction or slipping forces.
During their movement and necessary check That Not There are devices doctors, as pipes or drainage, which interfere and cause skin damage.
Foam or air mattresses are useful for repositioning, but their cost and effectiveness vary depending on the type.
The repositioning to 30° inclined it turns out more effective respect to the repositioning of 90° lateral.
When using the lateral position, pillows should be placed between the lower limbs to avoid contact between the knees and ankles (Bellingeri A., The handbook for the management of skin lesions, 2017).
If the person is bedridden, in the supine position, pillows should be placed under the legs, from the calf to the ankle, to keep the heels raised.
Nutrition should be understood as both an assessment of nutritional status and a nutritional intervention; it can prevent the onset or treat pressure ulcers. Specifically, in the study by (Banks MD et al., 2016) and the study by (Heyman et al., 2008), we can see improvements in patients with pressure ulcers. In the first article, using the graphs we saw earlier, we can see how, through the assessment of nutritional status and nutritional intervention itself, the area of the ulcer was significantly reduced, while in the second article, we can see how adequate nutritional intervention even led to the closure of the ulcer itself.
To the moment from the socket in load of the patient:
Considering a nutritional assessment is essential for any
individual at high risk of developing or suffering from a pressure
ulcer:
• To the moment of access to any context clinical- assistance;
• To every change from the conditions of health;
• When Not Yes observe a progression from the healing.
Send a consultation to a dietitian for any person at nutritional
risk, at risk of Ldp or carrier by Ldp And if necessary, also at a team
nutritional multidisciplinary for a more in-depth evaluation.
• Weigh the patient and investigate on body weight trends
• Evaluate the capacity of the individual of to feed oneself
independently
• Evaluate the adequacy of the income total of nutrients
• Develop an individualized nutritional plan for all
individuals with or at risk for pressure ulcers
Introit Caloric
• Supply a contribution caloric individualized
• Supply 30-35 kcal/kg/day a everyone the individuals’
carriers by Ldp or at risk
• Consider a correction of estimated caloric needs based on
to weight loss or gain or to the presence of obesity.
• Offer fortified foods and/or administer high-calorie, highprotein
nutritional supplements between meals when nutritional
needs cannot be met through the normal diet.
• Consider nutritional support (enteral or parenteral) when
intake oral caloric intake is insufficient.
Introit Protein
• Provide adequate protein intake to achieve positive
nitrogen balance in every patient at risk of developing pressure
ulcers.
• Supply 1.25-1.5 grams of proteins/kg/day a everyone the
patients to risk and carriers Of Ldp
• Assess the patient’s renal function to ensure that protein
intake is appropriate
• Consider supplementation with high protein and proteincontaining
formulas arginine and micronutrients in individuals
with Ldp Of third or fourth stage or with multiple Ldp.
Hydration
• Supply And encourage an adequate contribution daily of
liquids for their correct hydration of every individual at risk or
suffering from pressure ulcers
• Monitor individuals for signs and symptoms of dehydration
including changes in weight, skin turgor and diuresis
• Supply a major contribution of liquids to the individuals
with dehydration, fever, vomiting, diaphoresis, diarrhea, or a
lesion with abundant exudates
Vitamins And Minerals
• Provide and encourage individuals at risk of developing a
pressure ulcer to consume a balanced diet that includes a good
supply of vitamins and minerals
• Provide and encourage individuals at risk for and with
pressure ulcers to take vitamin and mineral supplements when
dietary intakes are poor or when a deficiency is confirmed or
suspected.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Andrea Bellingeri (2017) The handbook for their management from the injuries skin.
- Banks MD, Ross LJ, Webster J, Mudge A, Stankiewicz M, et al. (2016) Pressure ulcer healing with an intensive nutrition intervention in an acute setting: A pilot randomized controlled trial. Journal of wound care 25: 384-439.
- Kerry H Cheever, Janice L Hinkle (2017) Brunner- Suddarth, Medical- Surgical Nursing. Vol. 2.
- European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel (EPUAP /NPUAP, 2016).
- Francisco Manzano (2014) Comparison of two repositioning schedules for the prevention of pressure ulcers in patients on mechanical ventilation with alternating pressure air mattresses. Intensive Care Med 40: 1679–1687
- Heyman H, Van of Looverbosch FROM, Meijer EP, Schols JM (2008) Benefits of an oral nutritional supplement on pressure ulcer healing in long -term care residents. Journal Wound Care 17: 476, 480.
- Langer G, Fink A (2014) Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database of Systematic Reviews Issue 6.
- Natalie K Bradford (2016) Repositioning for pressure ulcer prevention in adults- TO Cochrane review. International Journal of Nursing Practice 22: 108-109
- National Institute for Clinical Excellence (2001) Pressure ulcer risk assessment and prevention.
- (2009) Prevention and treatment of pressure ulcers: Quick reference guides. Washington AD.
- Re LG, Fusetti V, Lusignani M (2017) Is repositioning regimen effective to prevent pressure injuries? Synopsis of systematic reviews. Nursing Professions 3: 150-160
- (2008) Risk assessment for prevention of morbidity and mortality: lessons for pressure ulcer prevention. Reynolds TM. J Tissue Viability 17(4): 115-120.
- Luisa Saiani, Anna Brugnoli (2010) Treaty Of care nursing. Vol 1-2.
- Wanderwee K, Clark M, Dealey C, Gunningberg L, Defoor T (2007) Pressure ulcer prevalence in Europe: a pilot study. J Eval Clin Pract 13: 227-235
- Kottner J, Halfens R, Dassen T (2009) An interrater reliability study of the assessment of pressure ulcer risk using the Braden scale and the classification of pressure ulcers in a home care setting. Int J Nurs Stud.
-
Sciandrone Gaetano Giuseppe*. The Effectiveness of the Repositioning and from the Assessment of the State Nutritional in Prevention and in the Treatment from the Injuries from Pressure. Iris J of Nur & Car. 5(4): 2025. IJNC.MS.ID.000617.
-
Pressure ulcer prevention, Nutritional status, Repositioning dear
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






