 Review Article
Review Article
Nursing Contributions to Smoking Cessation: Evidence-Based Strategies and Emerging Trends
Coello-Canedo E*
Pontifical University of Salamanca, Salamanca, II University of Salamanca, Salamanca, Spain
Coello-Canedo E, Professor, PhD St, MSc, RN, University of Salamanca, Salamanca, Spain.
Received Date:May 02, 2025; Published Date:May 21, 2025
Background: Tobacco use remains a major public health concern, contributing to millions of preventable deaths each year. Nurses play a critical
role in smoking cessation programmes by providing education, motivation, and treatment. However, gaps in knowledge regarding the most effective
strategies still persist, highlighting the need for continued research and innovation in this field.
Aim: This review aims to identify and analyse evidence-based nursing interventions in smoking cessation, considering strategies, pharmacological treatments and relapse factors.
Methods: A review was conducted in October 2024 in evidence published from 2019 to 2024. The search methodology was guided by the PCC
model and conducted in CINAHL Complete. Articles in English and Spanish, were included.
Results: Eleven studies were included, those present different theoretical perspectives that underpin nursing interventions aimed at smoking
cessation. Including group and individual education, the 5As’ model, personalized coaching and digital technologies such as mobile apps. The most
effective pharmacological treatments indicated are varenicline and bupropion.
Conclusion: Factors such as stress, social support and psychological dependence influence relapse. Nursing interventions in smoking cessation
are effective, combining education, pharmacological treatments and emotional support. Further research is recommended to optimize their impact
in various contexts and to improve cessation rates and their maintenance over time.
Keywords:Interventions; Nursing; Risk Factors; Smoking Cessation
Introduction
Tobacco use represents one of the foremost public health challenges in developed countries, with significant implications for preventable morbidity and mortality, as well as being one of the leading causes of disability [1,2]. According to the World Health Organization (WHO), tobacco is currently associated with over 8 million deaths annually, of which approximately [1,3] million are attributed to exposure to second-hand smoke. The WHO defines tobacco as “a product derived from the Nicotiana tabacum plant that contains nicotine as its primary addictive component, alongside other substances harmful to human health.” Any individual who consumes at least one cigarette per day over the past month is considered a smoker [1].
Despite global efforts to reduce prevalence, smoking continues to be a major public health concern, requiring comprehensive and multidimensional approaches. Within this context, nurses play a pivotal role in tobacco cessation programmes, including educating individuals on the risks associated with smoking, treating nicotine dependence, and advocating for stricter public health policies [2].
Various studies have investigated specific interventions such as wellness coaching, a therapeutic resource combining emotional support and practical tools, which have shown promising results in reducing nicotine dependence and daily cigarette consumption [3]. Furthermore, pharmacological management plays a critical role in smoking cessation by alleviating withdrawal symptoms and improving long-term quit rates. Medications such as varenicline (partial agonist of nicotinic receptors) and bupropion (dopamine and norepinephrine reuptake inhibitor) have been shown to enhance cessation outcomes, with evidence suggesting a superior efficacy of varenicline. Pharmacological treatment should be tailored to the individual, considering their specific characteristics and needs [4].
Nevertheless, nicotine dependence and psychosocial factors, as
negative emotional states, anxiety, depression, lack of support, and
low motivation, are significant predictors of relapse, as evidenced
by multiple studies [5,6]. Although notable progress has been
made, significant knowledge gaps remain regarding the most
effective nursing strategies to address smoking cessation across
diverse populations and contexts. Therefore, the primary aim of
this study is to explore and provide relevant insights into nursing
interventions within tobacco cessation programmes, addressing
the following research questions:
• What are the nurse strategies that can support smoking
cessation and prevent relapse?
• What are the main pharmacological treatments available
for smoking cessation?
• What individual and contextual factors influence smoking
relapse?
Methods
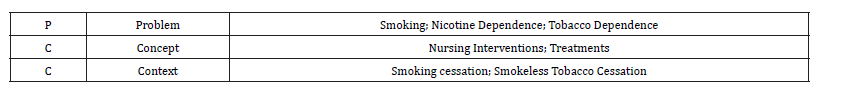
This review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) [7]. The MeSH terms identified can be appreciated in Table 1 Participants, Concept, and Context (PCC) framework, to improve clarity and reproductivity.
Table 1:PCC Framework.
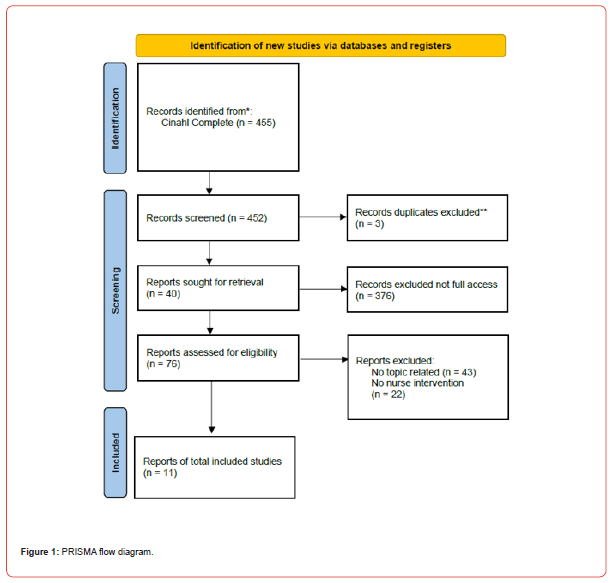
The search was conducted in CINAHL Complete, between October and November of 2024. Only evidence published in Spanish and Inglish was included. The temporal limitation ranged between 2019 and 2024. A total of 455 were found. The identified references were compiled, and duplicates were removed. Findings were assessed independently by each author following a three-step process: title, abstract, and revision of the full text, as proposed by PRISMA-ScR guidelines [7]. The study inclusion process founded eleven relevant articles. The selection process can be appraised in the PRISMA flow diagram (Figure 1).
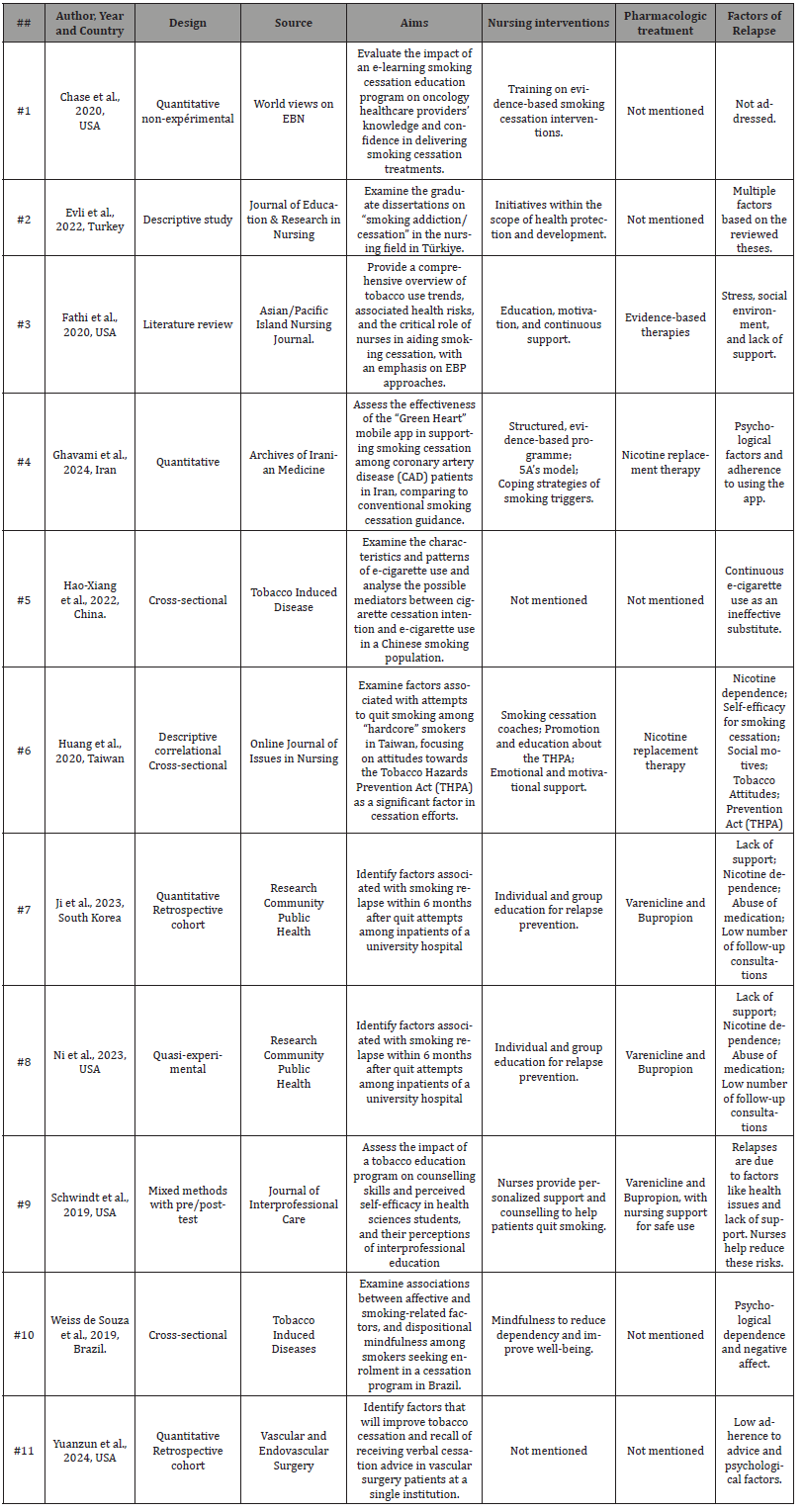
The literature found was assessed, and all data were evaluated by authors independently. Disagreements and transcription errors were avoided, and the study characteristics were summarized and presented in Table 2.
Table 2:Nursing interventions in smoking cessation.
Results
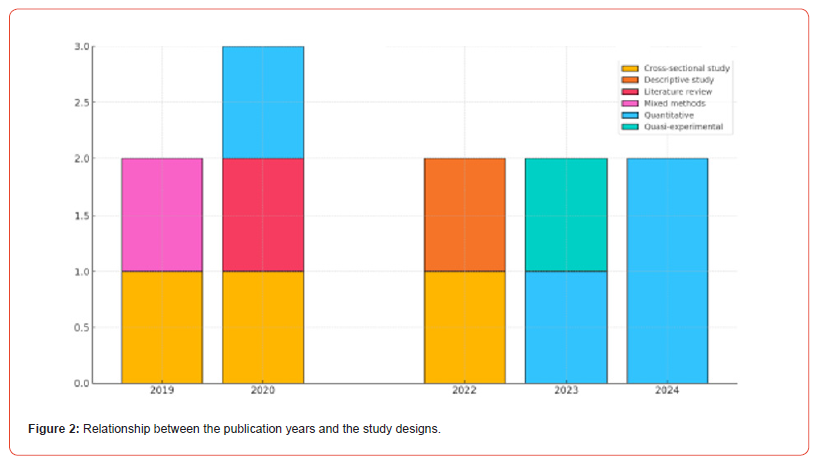
A total of eleven relevant articles were identified for analysis. The majority were published between 2019 and 2024, with a peak in 2020, which emerged as the year with the highest number of publications. The studies covered seven countries, with the United States being the most frequently represented. The relationship between the publication years and the study designs is illustrated in Figure 2.
In general, the studies focused on interventions for smoking cessation, emphasising the critical role of nursing interventions. These included individual and group-based education, personalised coaching, and evidence-based programmes such as the 5A’s model. These strategies were often complemented by pharmacological treatments, primarily nicotine replacement therapies and medications such as varenicline and bupropion.
The most common factors contributing to relapse included psychological dependence, stress, lack of social support, and challenges related to treatment adherence. Furthermore, the implementation of technology, such as mobile applications, was also explored as a tool to enhance cessation outcomes.
The analysis of the selected articles highlights key concepts essential to the smoking cessation process. Some are directly associated with nursing interventions, while others more broadly reflect the importance of holistic support for individuals attempting to quit smoking. Central themes identified across nearly all studies include evidence-based education, patient motivation, and continuous follow-up. Although the use of digital technology, particularly mobile apps, also emerged as an important intervention, this was more closely related to patient self-management. According to the authors’, such technologies appear to be particularly linked to promoting adherence and enabling personalised monitoring.
Specific Nursing Interventions
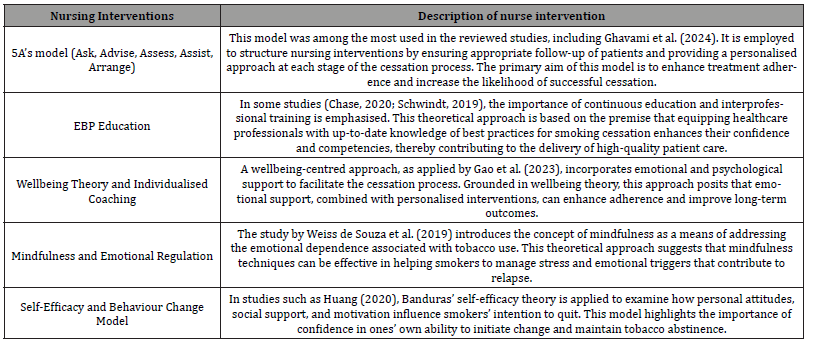
The analysed studies reflect a range of theoretical approaches underpinning nursing interventions in smoking cessation, which are detailed in Table 3.
Table 3:Study Characteristics.
Discussion
Smoking cessation is a complex process that requires biological, psychological, and behavioural addressing factors. Nicotine dependence remains one of the greatest challenges to sustained abstinence. For this reason, interventions that integrate pharmacological, emotional, and evidence-based educational approaches are crucial to effectively tackle smoking-related issues and their impact on public health [8-11].
Among pharmacological tools, treatments such as varenicline and bupropion have proven effective in increasing long-term cessation success rates. Notably, varenicline has demonstrated superior outcomes, making it particularly effective in supporting individuals to remain tobacco-free. These pharmacological options offer additional support by directly targeting physical dependence, thereby facilitating the quitting process [4].
Beyond pharmacological interventions, innovative strategies such as personalised wellbeing coaching have shown significant effectiveness in reducing nicotine dependence and daily cigarette consumption. These approaches humanise the process, blending emotional support with behavioural change, and offer a more holistic path to cessation [3].
Technology, particularly through mobile apps and digital tools, has emerged as a key ally in smoking cessation. These platforms enable personalised plans, educational content, and automated follow-up, thereby improving accessibility and offering continuous patient support [8]. Evidence suggests that digital solutions enhance cessation success rates by enabling patients to adhere more efficiently to their quitting process.9 However, not all individuals are willing or able to engage with such technologies, highlighting the importance of combining digital tools with traditional resources, such as printed educational materials, which can be equally effective in reinforcing intervention outcomes [12].
Nevertheless, not all strategies are equally supported by robust evidence. For instance, while the use of electronic cigarettes has gained popularity as a cessation aid, particularly among younger populations and individuals with greater purchasing power. More rigorous studies are still needed to determine their efficacy as a smoking cessation intervention [13].
Cessation not only involves quitting smoking but also maintaining this change in the long term, an outcome frequently compromised by relapse. Key factors associated with relapse include nicotine dependence, lack of support, and infrequent engagement in preventive consultations [4].
Emotional factors also play a critical role. The presence of negative affect, along with conditions such as depression and anxiety, significantly increases the risk of relapse. Conversely, positive affect and emotional wellbeing are strongly associated with successful cessation attempts. This underscores the need for interventions to go beyond, addressing physical dependence and also target underlying psychological factors [5].
Another essential factor in preventing relapse is self-efficacy, or the individuals’ confidence in their ability to quit smoking. Higher levels of self-efficacy have been associated with greater success in cessation attempts, whereas a low perception of personal capability increases the likelihood of relapse. Therefore, support strategies must actively promote self-efficacy by providing both practical tools and emotional reinforcement to strengthen the patients’ confidence in remaining smoke-free [6,10].
Nurses play a pivotal role in health education, informing patients about the risks associated with smoking and the benefits of cessation. Their responsibilities also extend to advocating for policy changes that support stricter regulations and preventive programmes, thereby fostering environments more conducive to a tobacco-free life [2].
Conclusion
The analysis conducted confirms the effectiveness of nursing interventions within smoking cessation programmes. Key strategies such as evidence-based education, the 5A’s model, and personalised coaching emerged as fundamental in enhancing patient motivation and adherence throughout the cessation process. In addition, pharmacological treatments, particularly varenicline and bupropion, proved to be effective tools in managing physical nicotine dependence, offering valuable support alongside behavioural strategies.
Patient satisfaction with nursing support was also a notable outcome, especially when care included ongoing accompaniment, emotional support, tailored interventions, and close follow-up. This comprehensive approach reinforces the essential role of nurses in health promotion, not only from an educational and clinical standpoint but also as a crucial source of emotional support during the quitting journey.
Despite the positive results observed, further research is recommended to identify and refine best practices, particularly in adapting interventions to diverse contexts and populations. A multidimensional, evidence-based approach will not only improve cessation rates but also support long-term maintenance of smoking abstinence, contributing significantly to the reduction of tobacco use as a major public health challenge.
Acknowledgment
The present revision work has been carried out by the students of the Nursing Degree of the Pontifical University of Salamanca MAL, LAS, IBC, IBG, NBM and YGM who preferred remaining anonymous once the designed final version. This publication aims to thank and reward the work done by this nurse students.
References
- World Health Organization (2023) Tobacco [Internet]. Geneva: WHO.
- Fathi J (2020) Tobacco use: The current state of affairs and how nurses can help patients quit. Online J Issues Nurs [Internet], 25(3).
- Gao N, Solomon P, Clay Z, Swarbrick P (2023) A pilot study of wellness coaching for smoking cessation among individuals with mental illnesses. J Ment Health [Internet] 32(1): 183-189.
- Bae JE, Kim C-W, Lee SE, Jang M (2023) Factors related to smoking relapse within six-months of smoking cessation among inpatients. J Korean Acad Community Health Nurs [Internet] 34: 307.
- De Souza I, Kozasa E, Rabello L, Mattozo B, Bowen S, Richter K, et al. (2019) Dispositional mindfulness, affect and tobacco dependence among treatment naive cigarette smokers in Brazil. Tob Induc Dis [Internet].
- Huang HW, Yang YH, Huang CL (2021) Factors associated with attempt for smoking cessation among hardcore smokers in Taiwan. Asian Pac Isl Nurs J [Internet] 5(4): 251-258.
- Tricco AC, Lillie E, Zarin W, O Brien KK, Colquhoun H, et al. (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine 169(7): 467-473.
- Ghavami M, Abdshah A, Ahmadi A, Akbarzadeh D, Mofidi A, et al. (2024) Effectiveness of applying Green Heart, a smartphone-based self-management intervention to control smoking: A randomized clinical trial. Arch Iran Med [Internet] 27(5): 255-264.
- Chase W, Zurmehly J, Amaya M, Browning KK [2020] Implementation of a smoking cessation e‐learning education program for oncology clinic healthcare providers: Evaluation with implications for evidence‐based practice. Worldviews Evid Based Nurs [Internet] 17(6): 476-482.
- Schwindt R, McNelis AM, Agley J, Hudmon KS, Lay K, et al. (2019) Training future clinicians: An interprofessional approach to treating tobacco use and dependence. J Interprof Care [Internet] 33(2): 200-208.
- Evli M (2022) Evaluation of graduate dissertations in the nursing field on smoking addiction/cessation in turkiye. J Educ Res Nurs [Internet] 19(3): 334-341.
- Peng Y, Rossi R, Falkenhain A, Bose S, Williams M, et al. (2024) Factors associated with tobacco cessation advice recall and quit rates in vascular surgery patients. A single center study. Vasc Endovascular Surg [Internet] 58(7): 714-722.
- Lin HX, Zhang Y, Chen MJ, Zheng YT, Yun QP, et al. (2022) The characteristics and patterns of e-cigarette use and its association with cigarette cessation intention in a Chinese smoking population: A mediation analysis. Tob Induc Dis [Internet] 20(February) p. 1-9.
-
Coello-Canedo E*. Nursing Contributions to Smoking Cessation: Evidence-Based Strategies and Emerging Trends. Iris J of Nur & Car. 5(3): 2025. IJNC.MS.ID.000614.
-
Interventions, Nursing, Risk Factors, Smoking Cessation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






