 Research Article
Research Article
Integrative Medicine for Cancer Pain: A Systematic Review
Wenhsing Yang* and Chieh Lin Yang
Department of Nursing, New York City College of Technology, USA
Wenhsing Yang, Department of Nursing, New York City College of Technology, USA
Received Date:March 05, 2024; Published Date:April 05, 2024
Abstract
Keywords:Pain management; Cancer pain; Holistic care approach; Adult cancer pain; Integrative cancer pain management
Introduction
Pain management is a branch of medicine that focuses on easing suffering and managing chronic pain to improve quality of life for an individual. Methods of pain management vary throughout history and differ among cultures. Many adult patients with cancer who experience chronic pain undergo palliative treatment. Currently, Western pain management differs greatly from integrative medicine. Our research explores whether integrative medicine in conjunction with Western medicine would provide more adequate pain relief and whether or not it provided an overall benefit to the patient. Previous research provided evidence that a more holistic, comprehensive pain management approach can help improve outcomes and increase cultural awareness [1]. We examined previous research which provided evidence to support this claim. While pain management in cancer patients has been a hot topic of many research studies, some researchers concluded using alternative methods of pain management in addition to the conservative treatment. Music therapy, massage therapy, herbal medications and even aromatherapy are all parts of integrative medicine that proved to have a significant benefit in pain management in cancer patients.
Methods: Electronic Search, Medline, PubMed, Google Scholar.
Populations
The populations selected for this paper shared the common characteristic of chronic pain related to cancer. There were no exclusion criteria for the type of cancer or staging. However, pain after the immediate period after oncologic surgery was excluded. No specific geographic locales or language were excluded. All participants had to be adults; no pediatric populations were included. The clinical setting chosen was primarily ambulatory and palliative care units. Inclusion criteria also consisted of studies implementing an allopathic intervention either as a single variable versus a placebo for cancer pain, or a controlled trial of allopathic medicine versus conventional western medicine. The five types of allopathic medicine selected for this review are: acupuncture, massage, music therapy, aromatherapy massage, holisticinterdisciplinary approach to cancer pain and traditional herbal medicine.
The systematic review and meta-analysis study on acupuncture for pain management in cancer had an inclusion criterion for RCTS investigating acupuncture for cancer pain. The participants were all adults, diagnosed with any type of cancer and no exclusion for staging. Acupuncture was used as the sole variable, but in studies that compared with conventional western medications, the analgesic drug had to be unchanged during the study period and finally the outcome had to be validated by a standardized pain measurement tool to ensure consistency [2]. Exclusion criteria were animal studies, case reports, qualitative studies, descriptive surveys, abstracts only and studies with inconsistent interventions [2]. Of the 1748 records identified via database search, 20 studies were included in the meta-analysis [2].
In the pilot study on the effects of full body massage on pain relief in metastatic bone pain, patients were selected from five inpatient oncology units in a Taiwanese teaching medical center. The study was a quasi-experimental, pretest-posttest design with repeated measures [3]. Inclusion criteria was the following: 1) patients had to be at least 18 years of age, 2) diagnosed with metastatic bone cancer, 3) experiencing at least moderate cancer pain, and 4) admitted to the unit at least 48 hours prior to the study [3]. Exclusion criteria were 1) if a patient was undergoing any major surgeries, 2) having any physical or psychological impairments, and 3) experiencing any physical condition that is contraindicated with massage [3]. During the six-month period, 36 patients met the study criteria but only 30 consented [3].
The McGill University health center retrospective analysis of an interdisciplinary approach to cancer pain targeted pharmacological versus nonpharmacological pain management interventions. The study was a retrospective chart review of the center’s established patients seen in the clinic between April 2013 and March 2014 [1]. Inclusion criteria consisted of a) patients had to be established in the practice and have had at least two follow-ups, b) patients that answered all questionnaires provided by clinic, and c) the medical chart contained all pertinent information needed for the study [1]. Of the 186 Canadian patients selected, 71 met the inclusion criteria [1]. All patients were adults.
A mixed methods pilot study on the effects of music therapy on cancer pain was designed to have a blended format between a randomized control trial and an exit interview fulfilling the qualitative requirement for a more holistic approach to research [4]. Thirty-one adult cancer patients met the inclusion criteria of a) currently receiving cancer treatment, b) spoke proficient English, and c) lacked any cognitive, psychotic, or hearing impairments [4].
The systematic and meta-analysis review on traditional herbal medicine (THM) selected articles only involving RCTs and utilizing oral forms of THM only [5]. Concomitant conventional treatment was accepted while placebo, conventional treatment, or no treatments were selected for control group [5]. A total of 24 RCTs were selected, all patients were Chinese or Korean adults currently being treated for cancer [5].
The meta-analysis on the effects of aromatherapy massage on cancer patients had inclusion criteria consisting of the following: “(1) the study design was randomized controlled trial, (2) the subjects were human, (3) the experimental group received massage with essential oil and the control group received usual care only, and (4) mean difference and standard deviation were reported in the article [6].” Study participants were all cancer patients from UK and USA, but no demographics such as age or gender were presented, nor the type or stage of cancer [6].
Interventions
In the study by Lee et al. [5] the effectiveness of traditional herbal medicine in combination with conventional therapy was examined. Botanicals such as Corydalis Rhizoma, Ligusticum Rhizoma, Libanotus; processed animal products such as Venenum Bufonis, Scorpion, Lumbricus; and processed minerals such as Borneolum Syntheticum and Realgar were all used to relieve pain by promoting blood flow and circulation. This systematic review concluded that the addition of traditional herbal medicine could significantly reduce the levels of pain experienced by cancer patients. Although herbal medicine uses in pain relief are still in the early stages of research, this particular study shows promising effects of utilization of botanicals, processed animal products, and processed minerals as traditional herbal medicine for pain relief [5].
In the article by Pérez et al. [1] the McGill University health center cancer pain clinic interdisciplinary approach to pain management was evaluated and discussed. The cancer pain clinic was established in 2011 to offer various approaches to access and management of cancer pain. The clinical team is composed of physicians, nurse clinicians and anesthesiologists all of whom specialize in oncology and palliative care. The patients receive care in person and follow-up phone calls. The patient’s case is reviewed by all the specialists involved and then the patient is assessed with all the specialists present in the room. Pain management treatments such as physiotherapy, occupational therapy, and psychosocial support are offered to the patient. Patients return to the clinic at regular intervals for follow-up on the pain management care and updated status of cancer status. According to this study, this type of multidisciplinary approach to pain management in cancer patients results in decreased pain and improved function [1].
The intervention of music therapy and music medicine in cancer patients to alleviate pain and assess the psychological outcomes was studied by Bradt et al. [4]. In this mixed methods intervention study, interactive music making with a music therapist and sessions where the patients listened to pre-recorded music without the presence of therapy, both showed improved pain symptom management. The use of music therapy in cancer patients helped them connect with their pre-illness self and bring out their playful and creative side [4]. This type of intervention allowed patients to express their emotions and benefit pain reduction in addition to traditional pharmacological therapy [4].
Massage therapy is another type of alternative medicine that is safe and beneficial to cancer patients. Jane et al. conducted a quasiexperimental study on the effects of massage therapy intervention on pain intensity, levels of anxiety and physiological measures in cancer patients [3]. A massage lasting between 40 to 50 minutes and that targeted head, neck, back, limbs and feet were performed by an oncology nurse trained in massage therapy [3]. The longterm effect of massage therapy on pain management and anxiety was found to be a very efficient form of pain management in cancer patients [3]. Aromatherapy massage is also a type of alternative treatment to improve the pain of cancer patients [6]. Aromatherapy is the use of essential oils that are derived from different kinds of plants. These oils can be applied to the skin or inhaled through the use of special diffusers. In the meta-analysis study, the effects of massage with aromatherapy oils on different symptoms of pain and anxiety were reviewed [6]. According to Chen et al. [6] the use of aromatherapy was initially practiced in Egypt and India thousands of years ago and relieved stress, depression, and alleviated pain.
The effectiveness of acupuncture for pain in cancer patients was evaluated in a study by Hu et al. [2]. Most of the time manual acupuncture is used based on the Traditional Chinese Medicine theory. There are different types of other acupuncture methods such as electro acupuncture, wrist-ankle, ear, and fire needle acupuncture that are all used in pain management. A particular set of acupoints that correspond to anatomical Zang-Fu organs were used for acupoint selection. The number of acupuncture sessions varies among different patients. The overall effect of acupuncture in cancer patients showed that acupuncture in addition to conventional drug therapy is more effective than drug therapy alone [2].
Discussion
The articles selected for this review span a variety of interventions in the pursuit of reducing pain among cancer patients. Methods, results, and testing were as varied as the individual interventions.
McGill University Health Center Cancer Pain Clinic used a holistic approach to pain management. While this research did not use RCTs and there was no control group, treatments included uses of opioids and analgesics as well as additional therapies. While this approach seems all-inclusive, “patients with severe pain at baseline and with recurrent or progressive cancer disease were less likely to experience pain improvement” [1].
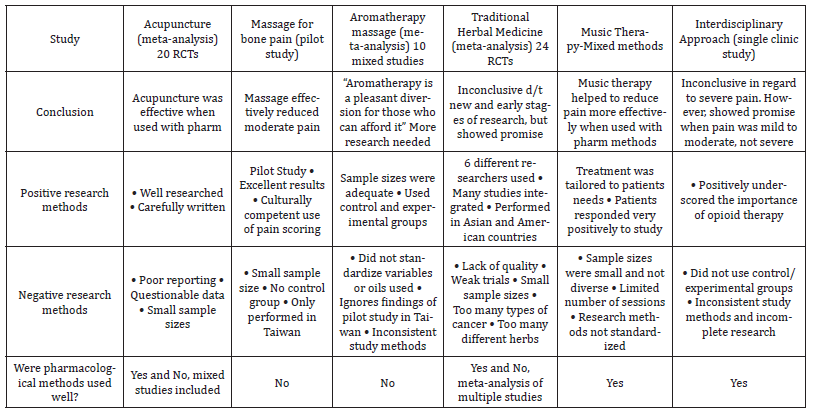
Despite the fact that some of the research was not completed due to participant dropout, the researchers were still able to conclude that an interdisciplinary approach and the use of opioids did effectively manage mild to moderate pain, however severe pain became much more difficult to manage. This conclusion leads the way for another alternative therapy such as integrative medicine to possibly fill the gaps identified in this study (Table 1).
Table 1:Table of Research Evidence.
Acupuncture for pain management in Cancer: A Systematic Review and Meta-Analysis. Eight authors contributed to this review article that compares acupuncture with pharmacological interventions or in conjunction [2]. Although many articles were deleted through the selection process, those that were chosen for inclusion were deemed limited by incomplete reporting, small sample sizes, inconsistent methods and somewhat inconclusive results. While acupuncture with pharmacology was seen as having better results than acupuncture alone, better quality testing is needed overall for this question. However, the significance of this study is the indication that pharmacological therapy is more effective when used in conjunction with acupuncture [2]. While well researched and carefully written, this review concludes with the need for further studies.
In the effects of full body massage on pain intensity, anxiety, physiological relaxation in Taiwanese patients with metastatic bone pain, this extremely limited (n=30) pilot study of full body massage executed by a single massage practitioner on patients with only a moderate amount of pain showed promising results of cutting pain and anxiety almost in half for an entire 18-hour period [3]. While no control group was used, descriptions by the patients were for the most part positive. Using a vertical coding system for the Chinese (whose language is vertical) patients helped them toward better reporting, this remains a single country experiment; cultural conditions can explain some of it but may not be replicated in countries where massage is not part of the culture Jane et al. [3]. This study needs a wider population and patients with a more diverse set of pain parameters. Also, the time of day seemed to be an important consideration as was the use of a single massage practitioner. There are many different types of massage available worldwide and just as many different types of massage practitioners. Some standardization would need to be included for wider studies.
In contrast to the latter article, 3 RCTs focused on aromatherapy (use of certain, unspecified, fragrant oils) massage but found no positive effect on pain relief [6]. Obviously, the authors recommend more research, but in comparing their results to the study of full body massage, there should be more of a consistent approach. This was a study between “usual care” (control group) and those receiving “aromatherapy massage” (experimental group). A better focus would have been to compare a “non-aromatherapy massage” (control group) and those receiving “aromatherapy massage” (experimental group). Then the single variable would be aromatherapy (oil), which also needs to be standardized across the research field. The authors conclude that the aromatherapy massage is “a pleasant diversion for those who can afford it” [6]. This ignores the positive results obtained in the previous pilot study.
The Chinese history of traditional herbal medicine is long and rooted in trial and error but is widely used and is spreading. Twenty-four RCT studies received a systematic review from six different researchers [5]. While fifteen were written in Chinese and nine were written in English, there were common flaws in all: lack of quality, weak trials, and small sample sizes. While the results so far show promise in the treatment of different kinds of cancer pain, the quality assessment chart was inconsistent, and it was sometimes challenging trying to figure out which herbal substance was the control, and which herbal substance was experimental. Too many kinds of cancer pains were included so that it was not focused on one problem. But that simply points to the need for more focused, simplified kind of testing. The herbals have been in use for centuries, but the testing has not. Future research should resolve some of these issues.
Music therapy, on the other hand, has a relatively short history and an even shorter testing period, but does show some promise. Originally, just listening to music was the approach used, but recently, a mixed methods study included two approaches to the use of music in therapy, music making (MM) and music therapy (MT) [4]. This was a very small sample (less than 40), a very limited number of sessions (2) and a limited variety of patients (mostly female and black) [4]. While the results showed positive results, further study would require a standardized approach to this with wider sample sizes and a variety of patients. The sessions explained a free form approach and some tailoring to individual needs, but ultimately, the method of using music therapy is akin to distraction from pain, which has been known the be effective, and likely can be replicated using others means of distraction, such as playful creativity or mood-altering relaxation. Similar studies could be done with activities like watching television, doing crafts (knitting), playing games, sensory deprivation tanks, group therapy, prayer, or meditation, or even visits from family members or therapy pets.
In looking at these approaches to pain reduction (tested drugs, traditional herbals, music, massage, and aromatherapy), and the additional ones proposed above (watching television, doing crafts (knitting), sensory deprivation tasks, group therapy, prayer, or meditation, or even having visiting pets), culture and experience, personality and sensitivity can play large parts in seeing which therapies can actually help. Patients with sensitivities toward odor would not do well with aromatherapy just as patients who do not like to be touched would not do well with massage. There can be many approaches to this pain problem even if they may merely be pleasant diversions. With minor pain, the patient can be helped with these additional therapies, but with acute pain, the patient will most probably need serious tested medications to provide relief.
Outcomes
As a whole, the majority of research supports that certain integrative approaches can manage pain effectively physically, while others need further research. However, there is a clear benefit that integrative medicine improves a patient’s experience psychologically. From a physical perspective, patients consistently reported decreases in their pain levels when integrative medicine such as massage and acupuncture were implemented, although the same case cannot be made in regard to aromatherapy and herbal therapy, which will be discussed in further detail below. The successes of the integrative studies do not diminish the importance of traditional Western methods, such as opioids, but only serve to make the argument that the addition of integrative measures with Western medications can be more effective than using either approach singularly. Treatments such as massage, acupuncture, and music therapy in conjunction with typical Western methods ultimately should provide the best outcomes for patients in regard to pain management.
The McGill University for Cancer Pain Management effectively underscores the positive and undeniable fact that Western medicine is indeed sufficient for managing pain, however that the inclusion of non-pharmacological methods improves outcomes. In the health care community, the goal is not only to manage pain sufficiently, but instead to manage pain optimally. By utilizing the nonpharmacological measures in conjunction with the pharmacological approaches, it was determined that 53% of patients responded with a pain reduction greater than 30%, thus proving the success of this method for managing pain [1]. A similar outcome was found in the article “Acupuncture for Pain Management in Cancer: A Systematic Review and Meta-Analysis” by Hu et al. [2], which determined that acupuncture alone is not as effective as opioids for managing pain, but when used in conjunction with opioids can be significantly more effective for managing pain in cancer patients than just using opioids.
In order to prove that this effect was not only due to the use of Western medication, but studies were also performed using only non-pharmacological interventions. In a pilot study [3], full body massages alone were shown to be very effective in managing pain in patients with bone cancer. The massages were shown to be effective for relieving symptoms of pain and anxiety both short term and long term, with the most significant benefit occurring 15 minutes after the massage, which is practically on par with short acting pain medication such as morphine, which was not utilized in this study.
In the study performed by Bradt et al. [4] on the impact of music therapy on psychological outcomes and pain in cancer patients, the data indicated that music therapy not only decreased pain scores, but also improved mood and psychological perspective of patient’s illness. As health care providers, we are aware that when patients have cancer, their pain is not solely physical, but also psychological. The study by Bradt et al. [4] underscores the importance of not only managing physical pain, as the music therapy was shown to help patients tap into inner resources such as playfulness and creativity, as well as provide for emotional expression, which opioids could never do.
This is not to say that all integrative therapies have been shown to be effective on their own. The examples of aromatherapy in the article “The Clinical Effects of Aromatherapy Massage on Reducing Pain for the Cancer Patients” by Chen et al. [6] and herbal medicine in the article “Traditional herbal medicine for cancer pain: A systematic review and meta-analysis” were not conclusive. In the meta-analysis by Chen et al. [6], aromatherapy did not yield any positive results, but the researchers acknowledge that further research is needed. In the meta-analysis by Lee et al. [5], the outcome showed that in some cases, traditional herbal therapy was effective for significantly diminishing pain, whereas in other studies, the same could not be concluded (site the “other studies” that did not conclude that). Ultimately, the conclusion can be drawn that further research is certainly needed in these areas.
Especially in cultures that do not necessarily believe in or trust traditional Western medication, the effort to include integrative medicine into the regiment for cancer patients can serve as a comfort that efforts are being made to understand and work collaboratively for optimal outcomes. The inclusion of multicultural integrative approaches may also help patients trust the process and the health care team by showing that an effort is being made to manage not only their physical pain, but also their psychological and emotional pain that comes with the cancer diagnosis. In turn, this may make patients who are otherwise not open to Western medications consider it more carefully. Ultimately, the culturally competent approach would be expected to decrease pain for patients with cancer, increase adherence to pain management regimes, and work to make patients feel more included in their care. This should prove to be particularly effective for patients who believe in integrative medicine more than traditional Western medicine.
Conclusion
The use of Alternative Medicine for Cancer pain management in conjunction with Western medicine is the best approach. The studies represented in this review all but two were a conglomeration of randomized control trials and excluded quasi-experimental and qualitative studies. There was statistical significance that massage, music therapy, acupuncture, traditional and herbal medicine had an effect on treating cancer pain. Aromatherapy massage did not show any significant difference. The pilot study on integrative medicine comparing pharmacologic versus nonpharmacologic pain management was successful but needs further randomized trials.
Given that this review showed statistically pertinent results, the introduction of integrative medicine should make its way across palliative care and oncology units. Often the reason for not implementing a proven strategy is lack of education and access. If hospitals and providers make it accessible to their patients, the results can be significant. Furthermore, if implemented, integrative medicine has the potential for influencing improved patient outcomes, more culturally competent care, improved satisfaction, decreased dependence on opioids, improved quality of life due to low to no side effects and possibly significant cost savings.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Perez J, Olivier S, Rampakakis E, Borod M, Shir Y (2016) The McGill University health center cancer pain clinic: A retrospective analysis of an interdisciplinary Approach to cancer pain management. Pain Research and Management pp.1-7.
- Hu C, Zhang H, Wu W, Yu W, Li Y, et al. (2016) Acupuncture for pain management in cancer: a systematic review and meta-analysis. Evidence-based Complementary and Alternative Medicine pp.1-13.
- Jane SW, Wilkie DJ, Gallucci BB, Beaton RD, Huang HY (2009) Effect of a Full-body massage on pain intensity, anxiety, and physiological relaxation in Taiwanese patients with metastatic bone pain: a pilot study. Journal of Pain and Symptom Management 37(4): 754-763.
- Bradt J, Potvin Kesslick A, Shim M, Radl D, Schriver E, et al. (2015) The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: a mixed methods study. Support Care Cancer 23: 1261-1271.
- Lee JW, Kee WB, Kim W, Min BL, Lee H, et al. (2015) Traditional herbal medicine for cancer pain: a systematic review and meta-analysis. Complementary Therapies in Medicine 23: 265-274.
- Chen TH, Tung TH, Chen PS, Wang ShH, Chao CM, et al. (2016) The clinical effects of aromatherapy massage on reducing pain for the cancer patients: meta-analysis of randomized controlled trials. Evidence-Based Complementary and Alternative Medicine pp.1-6.
-
Wenhsing Yang* and Chieh Lin Yang. Integrative Medicine for Cancer Pain: A Systematic Review. Iris J of Nur & Car. 4(5): 2024. IJNC.MS.ID.000600.
-
Pain management, Cancer pain, Holistic care approach, Adult cancer pain, Integrative cancer pain management
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






