 Research Article
Research Article
Effects of Body Repositioning in Immobilized Patients to Prevent Pressure Ulcer in Intensive Care Units at Public Hospital, Pakistan
Nasira Hassan1*, Muhammad Afzal2, Sana Sehar3 and Syed Amir Gilani4
1Lahore School of Nursing, University of Lahore, Pakistan
2Associate Professor, The University of Lahore, Pakistan
3Assistant Professor, The University of Lahore, Pakistan
4Faculty of Allied Health Sciences, The University of Lahore, Pakistan
Nasira Hassan, Lahore School of Nursing, University of Lahore, Pakistan.
Received Date: November 18, 2019; Published Date: February 06, 2020
Abstract
Background: A communal health problem amongst immobilized patients is pressure ulcer that extend their period of hospitalization.
Objective: The objective of this study was to assess the effect of body repositioning in immobilized patients to prevent pressure ulcer in intensive care units at public hospital, Pakistan.
Research Methodology: A quasi experimental with non-equivalent control group design was used to assess the effect of body repositioning among immobilized patients to prevent pressure ulcer.
Results: A major difference between the interventional (1.35±.520) and control group (1.73±.790) mean of body repositioning to reduce the pressure ulcer among immobilized patients. P value is 0.000 which was less than .001 shows an important difference in mean of interventional and control group.
Keywords: Intensive care units (ICU); Pressure ulcer (PU)
Introduction
A communal health problem amongst immobilized patients is pressure ulcer that extend their period of hospitalization [1]. Pressure ulcer is confined impairment to the underlying tissues or skin above bony notorieties resulting from continued pressure [2]. Pressure ulcer start from mild reddening of skin to the damage of tissues and infection spread to muscles and bone [3]. Elbow, hip, back of head, heels, toes, shoulders, knees and thighs are body areas which are commonly predispose to pressure ulcer [4].
Pressure ulcer is a common community health problem. High mortality rate among immobilized patients is because of pressure ulcer [5]. It was one of the health care harm which lengthen the hospital stay and increase twenty percent of the total cost for the health care treatment [6]. In intensive care units more than 6000000 patients suffered from pressure ulcer, cost of 6 million patients treatment was 2.17 billion dollars. Moreover, pressure ulcer can harm to patients like pain, expensive treatment, Elongated hospitalization [7], physical and emotional problem, adverse social and psychosomatic impression lead to premature mortality [8].
The incidence of pressure ulcer among immobilized patients is not clear to determine because there are several epidemiological studies with different methodologies which present different prevalence and incidence rate [9]. However, international rate of PU in UK is 4.5%-25.2%, in Spain is 2.9%- 8.34%, in England is 14.8% and in USA is 19.1% [10]. Repositioning has long been vital constituent of pressure ulcer prevention (PUP). Repositioning (supine, lateral position) is one approach used along other protective strategies to release pressure and so preclude pressure ulcer. Repositioning schedules are used to dispense the pressure amongst the body and support surfaces [11]. Two hourly repositioning schedules is a standard care to the immobilized patients that must be applied, but in practice these standards were not regularly implemented [12].
Furthermore, 80% to 95% pressure ulcer are preventable from severe harm or even death [13]. It is the vital part of nursing care because all nurses are remaining forefront in the care of atrisk patients and subsequent provision of preventive measure to minimize the bedsore among immobilized patients [14]. To reduce the rate of bedsore among immobilized patients, there is need of special care and need to be educated [15]. Repositioning, skin care, nutrition and education of health care workers are preventive interventions of pressure ulcer among immobilized patients.
A prospective randomized control trial was conducted at western Ontario university, includes all physician of medicine on evaluation of a particular repositioning maneuver web-based teaching module consist of small group particular repositioning maneuver (PRM), standard classroom instruction and web-based module. The results were web-based module is very effective than SG and CI [16]. Another study was conducted to reduce the HAPU among bedridden patients by implementing novel care-based guidelines and preventive intervention (2 hourly repositioning, balanced and planned nutrition, pressure reducing beds, timely surgical interventions, education to care givers and wound/ skin checked by specialist nurse). Sample size was 9,755 patients. A paired sample t-test was used. Chi-square analysis was done. Only 89 patients were developed PU. Incidence rate of PU was reduced from 1.36% to 0.39% (p=0.002) in three years [17].
Study Objective
The objective of this study was to assess the effect of body repositioning in immobilized patients to prevent pressure ulcer in intensive care units at public hospital, Pakistan.
Methods
Research design
A quasi experimental with non-equivalent control group design was used to assess the effect of body repositioning among immobilized patients to prevent pressure ulcer.
Study Settin
Intensive care units of Neurosurgery department at public hospital, Pakistan.
Population
Study population was all immobilized patients who were admitted in intensive care unit.
Sampling
All immobilized patients were recruited through convenient sampling. Here two groups were formed. Intervention group is the one group on whom the nurses were performed repositioning preventive measure. Control group was for comparison purpose. The data collection procedure for patients was such that on day three of admission patients was assessed and 10 patients each group was followed for ten days. Then at day ten prevalence of pressure was observed in both groups and compared. Similarly, in this way 100 intervention group patients and 100 control group patients were followed over a period of 100 days in 10 10 groups for 10 days period each subgroup. After completing 100 patient’s assessment in intervention group and in control group the mean prevalence pressure ulcer score was assessed.
Research Instrument
The research instrument was consisting of following segments:
Socio-Demographic Data
It was utilized for collecting relevant data characteristics such as patients’ age 18-50 years, both genders; degree of pressure ulcer at 3rd and 10th day of assessment, abdominal circumference (inches) and co-morbidities.
Braden risk assessment scale
Braden risk assessment scale was used to evaluate the risk of pressure ulcer among ICUs patients by nurses
Repositioning of immobilized patients
Repositioning practices were done by nurses to minimize the risk of pressure ulcer among ICUs patients. Repositioned the immobilized patients 2 hours in supine position, 2 hours in a right lateral position 30° and 2hours in a left lateral position and continue the repositioning cycle in 24hour.
Data Collection Procedure
After taking endorsement to conduct this study from head of department.
Braden risk assessment scale
The first assessment of the patients was Braden risk assessment scale. The patients who are at high risk for developing pressure ulcer were received prevention intervention (repositioning). Braden risk assessment form was filled by nurses with help of researcher at morning time. Braden risk assessment form was kept in the nursing file.
Minimize the pressure
The patients who are at high risk for developing pressure ulcer was repositioned 2 hourly. Repositioning schedule was attached at the bed side of patient. The staff nurse was responsible to comply the scheduled position and was mark the assigned position in her flow sheet. The researcher certified the patient’s position according to schedule position in morning, evening and night shift on daily basis.
Results
In the above (Table 1) findings state that in the interventional group there were total 72(72%) males and 28(28%) females while in the group where no intervention was performed males were 77(77%) and females were 23(23%). The age demographics of the patients, age 18-25 years were 40 (40%) in interventional group while 36(36%) in no intervention group. In interventional group 12(12%) were 26-30 years whereas 10(10%) were age 26-30 in no intervention group. 7(7%) and 9(9%) participants were age 31 to 35 years in intervention and no intervention group simultaneously. Similarly, 5(5%) and 10(10%) were age 36-40 years respectively in two groups. In the age group 41-45 years 11(11%) were in intervention group whereas 5(5%) in no intervention group. 25(25%) in the intervention group were age 46 to 50 years while 30(30%) participants were in no intervention group in the same age.
Table 1: Table 1
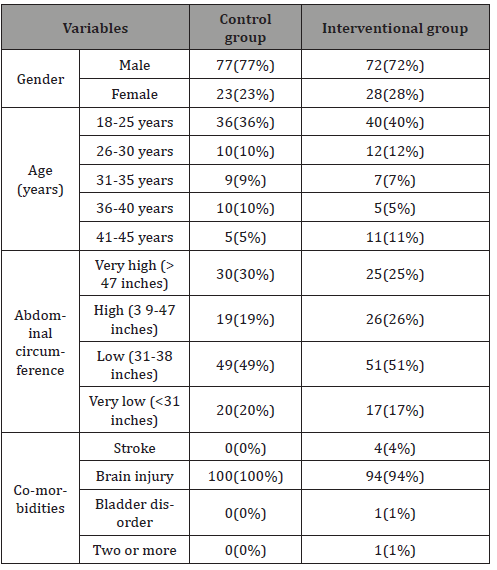
Table findings suggest that abdomen circumference was very high >47 inches 6(6%) in interventional group and 12(12%) in non- interventional group. High abdomen circumference 39-47 inches was 26(26%) in intervention group while 19(19%) in no intervention group. 51(51%) in intervention group had low abdomen circumference while in no intervention group 49(49%) had low abdomen circumference. 17(17%) and 20(20%) were having very low abdomen circumference in intervention and no intervention group respectively.
The above table findings reveal that in the intervention group the major comorbidity was brain injury 94(94%), followed by stroke 4(4%) and bladder disorder 1(1%). On the other hand, in the no interventional group all the participants were having brain injury as a major comorbidity. (Table 2) shows the statistics of patients’ pressure ulcer on initial assessment where in the interventional group 80(80%) of the participants had no pressure ulcer at all and 20(20%) had 1st degree of pressure ulcer whereas in the no intervention group 69(69%) of the patients had no pressure ulcer initially while 31(31%) had 1st degree pressure on initial assessment. Above table shows the statistics of patients’ pressure ulcer on day 10 assessment where in the interventional group 72(72%) of the participants had no pressure ulcer at all and 27(27%) had 1st degree of pressure ulcer and 1(1%) had 2nd degree pressure ulcer. On the other hand in the no intervention group 47(47%) of the patients had no pressure ulcer on day 10,34(34%) had 1st degree pressure on day 10 assessment, 18(18%) had 2nd degree of pressure on that assessment and 1(1%) had 3rd degree of pressure ulcer.
Table 2: Table 2
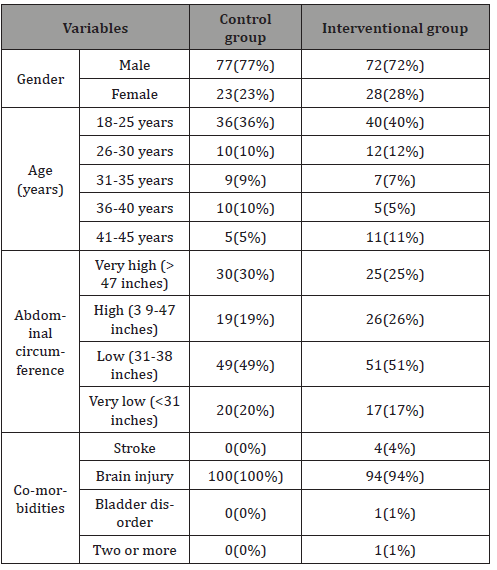
Table 3: Pressure Ulcer Difference between Intervention and no intervention group at day 10.
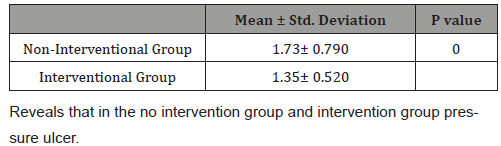
(Table 3) Reveals that in the no intervention group and intervention group pressure ulcer scores on day 10 was found significantly different. The no intervention average pressure ulcer score on day 10 was 1.73+0.790 while the intervention group pressure ulcer score was less 1.35+0.520. There was significant difference in both intervention and no intervention pressure ulcer score which reveals the effect of pressure ulcer preventive measures on patients where p- value was 0.000, less than 0.05 shows the significant effects of the pressure ulcer preventive measures on the prevalence of pressure ulcer in the long term bed ridden patients in the Intensive care units.
Discussion
A common health problem amongst immobilized patients is pressure ulcer that extends their period of hospitalization. In ICUs, there are 6000000 patients which suffered from PU and cost of treatment of those patients were 2.17 billion dollars [1]. Due to PU, there is high mortality rate among bedridden patients in intensive care units (Jiang et al., 2014). In the current study incidence rate of PU was 25% according to hospital statistics which was very high. Incidence rate of PU among immobilized patients is not clear due to different methodologies [9]. International PU rate was 4.5%-25.2% in United Kingdom, 2.9%-8.34% in Spain, 14.8% in England and 19.1% in USA [10].
Furthermore, the current study tested the pressure ulcer rate among immobilize patients by applying 2 hourly repositioning schedules. Pressure ulcer difference among non-intervention (1.73±0.790) and intervention group (1.35± 0.520), p-value was 0.000 showed significant effect of repositioning to reduce the bedsore.
Limitations
The sample proportion is small and from a particular confined group therefore the results cannot be comprehensive to the larger population.
Acknowledgement
I would like to special thanks to my supervisor, co-supervisor and my colleagues for help. Secondly, I would like to thank a lot to my gratitude parents, husband as well as my children who help me in finishing the study.
Conflict of interest
No Conflict of interest.
References
- El saidy TMK, Aboshehata OK (2019) Effect of Skin Care and Bony Prominence Protectors on Pressure Ulcers among Hospitalized Bedridden Patients. American Journal of Nursing 7(6): 912-921.
- Fletcher J, Hall J (2018) New guidance on how to define and measure pressure ulcers. Nursing Times 114(10): 41-44.
- Kaitani T, Tokunaga K, Matsui N, Sanada H (2010) Risk factors related to the development of pressure ulcers in the critical care setting. J Clin Nurs 19(3‐4): 414-421.
- Gunningberg L, Stotts NA, Idvall E (2011) Hospital‐acquired pressure ulcers in two Swedish County Councils: cross‐sectional data as the foundation for future quality improvement. Int Wound J 8(5): 465-473.
- Jiang Q, Li X, Qu X, Liu Y, Zhang L, et al. (2014) The incidence, risk factors and characteristics of pressure ulcers in hospitalized patients in China. Int J Clin Exp Pathol 7(5): 2587-2594.
- Gunningberg L, Hommel A, Bååth C, Idvall E (2013) The first national pressure ulcer prevalence survey in county council and municipality settings in Sweden. J Eval Clin Pract 19(5): 862-867.
- Schumacher C (2018) Hospital Acquired Pressure Injury Prevention on an Inpatient Unit.
- Moraes JT, Borges EL, Lisboa CR, Cordeiro DCO, Rosa EG, et al. (2016) Conceito e classificação de lesão por pressão: atualização do National Pressure Ulcer Advisory Panel. Revista de Enfermagem do Centro Oeste Mineiro 6(2).
- Guest JF, Ayoub N, McIlwraith T, Uchegbu I, Gerrish A, et al. (2017) Health economic burden that different wound types impose on the UK's National Health Service. Int Wound J 14(2): 322-330.
- Smith IL, Brown S, McGinnis E, Briggs M, Coleman S, et al. (2017) Exploring the role of pain as an early predictor of category 2 pressure ulcers: a prospective cohort study. BMJ open 7(1): e013623.
- Gillespie BM, Chaboyer WP, McInnes E, Kent B, Whitty JA, et al. (2014) Repositioning for pressure ulcer prevention in adults. Cochrane Database Syst Rev (4): CD009958.
- Coyer F, Lewis P, Tayyib N (2013) A prospective observational study of patient positioning in a Saudi intensive care unit. Middle East Journal of Nursing 101(449): 1-9.
- Tingle J (2016) Protecting patients: pressure ulcer prevention. Br J Nurs 25(20): 1146-1147.
- Kaur S, Singh A, Tewari MK, Kaur T (2018) Comparison of two intervention strategies on prevention of bedsores among the bedridden patients: A quasi experimental community-based trial. Indian J Palliat Care 24(1): 28-34.
- Jaul E, Barron J, Rosenzweig JP, Menczel J (2018) An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr 18(1): 305.
- Tabanfar R, Chan HH, Lin V, Le T, Irish JC (2018) Development and face validation of a Virtual Reality Epley Maneuver System (VREMS) for home Epley treatment of benign paroxysmal positional vertigo: A randomized, controlled trial. Am J Otolaryngol 39(2): 184-191.
- Lam C, Elkbuli A, Benson B, Young E, Morejon O, et al. (2018) Implementing a Novel Guideline to Prevent Hospital-Acquired Pressure Ulcers in a Trauma Population: A Patient-Safety Approach. J Am Coll Surg 226(6): 1122-1127.
-
Nasira H, Muhammad A, Sana S, Syed A G. Effects of Body Repositioning in Immobilized Patients to Prevent Pressure Ulcer in Intensive Care Units at Public Hospital, Pakistan. Iris J of Nur & Car. 2(4): 2020. IJNC.MS.ID.000543.
-
Immobilized Patients, Ulcer, Intensive Care, Pressure Ulcer, Health Problem, Hospitalization, Muscles and Bone, Health Care, Epidemiological, Skin Care, Particular Repositioning Maneuver, Physician, Surgical Interventions, Abdominal Circumference, Nursing
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






