 Research Article
Research Article
The Orthopedic Features in Children - Hockey Players
Koryukov YA, SKA Medical Center, St. Petersburg, Russia.
Received Date: April 21, 2021; Published Date: May 24, 2021
Abstract
Hockey as a power and quite injury and dangerous sport, presents the children’s body with high requirements for general physical training and accompanying orthopedic pathology. These are the issues of providing high-quality specialized medical care in cases of injuries of young hockey players, orthopedic examinations and deciding on the admission to training and competitions of healthy and injured children and adolescents, along with adult professional hockey players, that are within the competence of doctors of orthopedic doctors of the SKA medical center.
Keywords:Young hockey players; Injuries; Orthopedic examinations; Medical care
Introduction
The desire to be strong, to find a place in sports leads many boys to hockey. Increased involvement of children and adolescents in sports is accompanied by increased levels of musculoskeletal injuries [1-3]. At the same time, damage from overload accounts for about 50% of all children’s sports injuries [4,5]. Against the background of a sharp rejuvenation of sports, injuries from overload of the musculoskeletal system (ODA) are increasingly found in young athletes [6].
The role of the pediatric orthopedic surgeon, who is involved in the medical support of children hockey players, is undeniable, since, in addition to providing rehabilitation assistance for injuries to the musculoskeletal system and their consequences, he conducts a medical examination of the athlete and is able to determine the accompanying functional disorders of the musculoskeletal system, which due to lack of time may be inaccessible to the sports doctor of the professional hockey team. We are talking primarily about the presence of such concomitant orthopedic disorders as connective tissue dysplasia (DST) and osteochondropathy. Professional sports not only provoke their development or exacerbate them but are also an obstacle to demonstrating their higher capabilities and achieving high personal and team results [1]. Physiologically, changes in morphological profile related to the athlete’s anaerobic activity, his total body weight, loss of a certain proportion of muscle volumes lead to the expected decrease in performance [3,7]. Rational planning of training loads is important to combine with adequate nutrition in order to achieve good sports form by the time the competition begins [7-9].
Of considerable importance is the so-called labor protection of a young athlete, which consists in the admission to training and competitions of an absolutely healthy child who did not have a history of traumatic injuries or was injured, treated and ready to return to the ice [10].
Material and Methods
68 children hockey players of age from 16 to 17 years were examined, who were professional players of the youth composition of the SKA hockey club, sent to the medical center by team doctors this season. Of these, 35 (51.5%) people underwent a general medical examination in order to prevent the pathology of the musculoskeletal system at the stages of preparation for sports competitions and received admission to them. Another group - 33 (48.5%) children, was examined and treated for various injuries suffered [11].
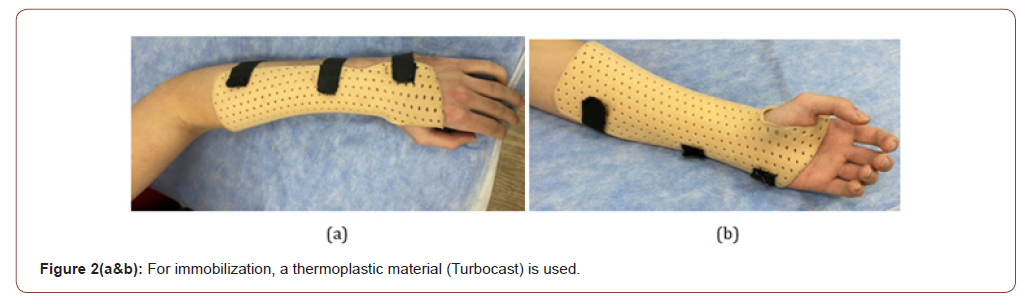
Upper limb injuries were detected in 8 (11.8%) people: damage to the capsule-ligament apparatus of the acromial-clavicular joint (S43.5) - 2 cases, the shoulder joint (S43.4) -1, at the level of the finger (S63.6) -2 (Figure 1&2).

There were also more severe injuries-dislocation of the shoulder joint (S43.0) in one child, a broken finger (S62.6) -1, an injury to the tendon of the rotational cuff of the shoulder (S46.0) -1. In one case, a hand contusion occurred (S69.8).
In most cases, 25 (36.8%) children had a lower limb injury (Figure 3). We noted the dislocation of the sacroiliac joint (S33.2) - 1 case, the contusions of the hip (S70.1) was revealed in 2 children, the tibia (S80.1) -1, the foot (S90.3) -2; there was also an injury to the leading thigh muscle and its tendon (S76.2).

4 young hockey players received severe knee injuries with ligament damage, of which 2 had damaged lateral ligaments (S83.4) and 2 had cruciform (S83.5). Ligament rupture at ankle level (S93.2) found in 3 patients. 2 children suffered fractures of the lower limbs: multiple fractures of the shin (S82.7) -1 and a fracture of the metatarsal bones (S92.2) -1.
As methods of diagnostic examination of patients, our center used: anthropometric, suboscopy, somatoscopy, as well as instrumental methods (radiography, MRI, ultrasound, CT).
Among children hockey players, the cardiorespiratory system is subjected to high loads. Therefore, in preparation for training, careful pediatric and functional diagnostics were required: ultrasound, EkoKG, ergo spirometry, cycling ergometry, Wingate test.
Methods of rehabilitation of childhood athletes included physiotherapy (shock wave therapy, magneto and laser therapy, cryotherapy), blood clot-enriched plasma cites injections, massage, manual therapy, LFC, kinesiotherapy, and type orthosis from the turbocast and upper/lower extremity official orthoses.
Results and Discussion
A sport such as hockey is characterized by damage to the lower limbs, which was statistically confirmed in our studies, and damage of the ligaments of large joints was also found in most cases of injuries - in 11 athletes. It drew attention to the presence of very severe injuries of 5 young hockey players in the form of dislocations and fractures. They for a long time turned off children from active sports life.
The vast majority of injuries were sustained by hockey players during games, and not in the training process. The higher motivation of the competitive period, overdue our dedication, a larger number of martial arts caused high injuries. This was especially manifested during the playoff period against the background of increased body fatigue, even higher intensity of loads and lack of time for full recovery. The causes of injuries were also: a rotational mechanism (damage to the ligaments of the ankle and knee joints), high-energy blows with a club and a washer.
A number of hockey players (35%) during the examination showed signs of connective tissue dysplasia (DST), which could serve as factors provoking and aggravating game damage. It is well known that DST suggests a genetically determined disorder in its development in the form of defects in its fibers and base material. As a result of such disorders, numerous disorders of tissues, parts of the body and the body as a whole are known. The main predictor of DST is hypermobility syndrome in the joints. It was simply determined by tests aimed at flexion/unbending in the elbow and knee joints, joints of the fingers of the hand and foot. Exceeding the physiological amplitude of movements leading to recurvation in large joints (extension of more than 5 degrees in the elbow, more than 0 degrees, in the knee), the ability to get the inner surface of the forearm with a flexion of the hand with a thumb, and when the fingers of the hand in the metacarpophalangeal joints are extended up to 90 degrees or more, lead the foot to shin up to 45 degrees, determined.
Some dysmorphies were also found among children with DST: a deformed auricle, curved minuscules, incomplete syndactyly of the toes of the feet. As methods for preventing subsequent injuries against the background of CST, we recommended additional exercises with physical training instructors in order to strengthen the muscle-ligament apparatus of the limbs (for example, the use of unstable platforms).
Methods of restorative treatment after injuries of the upper and lower limbs in quantitative terms were presented as follows: 1. Shock wave therapy 3-5 procedures, 1-2 times a week; 2. Barocamera 10 procedures for 60-90 minutes, daily; 3. Myostimulation 2 times a day for 30-60 minutes, 10-15 procedures; 4. Oscillator therapy 10 procedures daily; 5. Magneto-vacuum therapy on Vakumed sport apparatus 10-15 procedures, daily; 6. Electrophoresis and phonophoresis 10-15 procedures; 7. Laser therapy 5-7; 8. Highintensity magnetotherapy 7-10. All procedures were prescribed in accordance with the identified pathology, but no more than 3 varieties of procedures per treatment course. Procedures were also assigned depending on the stage and timing of the restoration.
PRP therapy was performed in 4 patients after damage to the rotating cuff of the shoulder, a bruised tibia, which provoked an exacerbation of Osgood-Schlatter disease, leading the thigh muscle, the lateral ligament of the knee joint. The course of treatment consisted of 2-3 injections into the injury zone with an interval of 5-7 days. Against the background of treatment, patients noted a decrease in tissue swelling and a decrease in pain syndrome in the limb.
Conclusion
1. An important component of reducing the number and severity of injuries in children hockey players is the presence of full equipment, proportionate shoes, high-quality and full-fledged protective equipment. Attention was paid to the treatment of ordinary calluses, sweats, etc. The best completion of the gameplay was the well-built warm-up and final parts of the training of children - hockey players, cyclically repeated exercises at a calm even pace, post-training stretches.
2. Non-drug therapy included strict adherence between game modes, including nutrition, where emphasis was placed on the consumption of full-fledged proteins and products containing polyunsaturated fatty acids. In therapy, DST recommended the use of food additives containing both the above substances and hyaluronic acid, synthetic analogues of vitamins K and D3, ascorbic acid, Omega 3, correctors for disrupting the synthesis and catabolism of glycosaminoglycan - chondroitin sulfate and succinic acid, corrector of bioenergy processes carnitine chloride.
3. The correct attitude to recovery procedures, both specialists and young athletes themselves, is a key to minimizing injuries.
4. Timely and additional examinations by doctors of a specialized medical center and adequate treatment tactics not only facilitated children’s sports, but also affected the quality of sports results.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Berkus MD, Langer O, Samuelloff A, Zenakis EM, Field NT, et al. (1994) Meconium stained amniotic fluid: Increased risk for adverse neonatal outcome. Obstet Gynecol 84: 115-120.
- Nathan L, Lenevo KJ, Camody TJ, Kelly MA, Sherman ML (1994) Meconium: a 1990s perspective on an obstetric hazard. Obstet Gynecol 83: 329-332.
- Ahanya SN, Lakshmanan J, Morgan BL, Ross MG (2005) Meconium passage in utero: mechanisms, consequences, and management. Obstet Gynecol Surv 60: 45-56.
- Wiswell TE (2001) Handling the meconium stained infant. Semin Neonatol 6(3): 225-231.
- Wiswell TE, Henley MA (1992) Intratracheal suctioning, systemic infection and the meconium aspiration syndrome. Pediatrics 89: 203-206.
- Cleary GM, Wiswell TE (1998) Meconium-stained amniotic fluid and the meconium aspiration syndrome - An update. Pediatr Clin North Am 45: 511-529.
- Maymon E, Chaim W, Furman B, Ghezzi F, ShohamVardi I, et al. (1998) Meconium stained amniotic fluid in very low risk pregnancies at term gestation. Eur J Obstet Gynecol Reprod Biol 80: 169-173.
- Wiswell TE, Bent RC (1993) Meconium staining and the meconium aspiration syndrome. Unresolved issues. Pediatr Clin North Am 40: 955-981.
- Kligner MC, Kruse J (1999) Meconium aspiration syndrome: Pathophysiology and prevention. J Am Board Fam Pract 12: 450-466.
- Romero R, Hanaoka S, Mazor M, Athanassiadis AP, Callahan R, et al. (1991) Meconium-stained amniotic fluid: a risk factor for microbial invasion of the amniotic cavity. Am J of Obstet Gynecol 164(3): 859-862.
- Shukla OS, Swapna ST (2019) Study of risk factors, clinical profile, and outcome in meconium-stained deliveries. Indian J Child Health 6(5): 213-216.
- Divia A (2018) Study on Risk Factors and Perinatal Outcome in Meconium Stained Liquor, Dissertation pp. 64-70.
- Gupta V, Bhatia BD, Mishra OP (1996) Meconium stained amniotic fluid: antenatal, intrapartum and neonatal attributes. Indian Pediatrics 33(4): 293-297
- Patil KP, Swamy MK, Samatha K (2006) A one year cross sectional study of management practices of meconium stained amniotic fluid and perinatal outcome. Obstet Gynecol India 56: 128-130.
- Bhatia BD, Gupta V, Dey PK (1996) Meconium aspiration syndrome: current concepts. Indian J Matern Child Health 7(1): 1-7.
- Khatun M (2005) Meconium Staining liquor and its correlative with fetal outcome within seven days of birth in Dhaka Medical College. Dissertation. Bangladesh College of Physicians and Surgeons pp. 39-43.
-
Koryukov YA, Nikulina AV. The Orthopedic Features in Children - Hockey Players. Glob J of Ped & Neonatol Car. 3(4): 2021. GJPNC. MS.ID.000568.
Computed Tomography, Head trauma, Emergency department, Children, Vomiting, Glaxo coma scale, Risk, CT imaging, Patients, Disorder
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






