 Research article
Research article
The Difference in Patterns of Dyslipidemia in The U.S. Hispanic and Asian Indian Adolescents
Naveen Mehrotra1 and Anna Petrova2*
1Board Certified in Pediatrics, Adjunct Assistant Professor, Division of Epidemiology, Rutgers School of Public Health
2Professor of Pediatrics, Department of Pediatrics, Rutgers Robert Wood Johnson Medical School, USA
Anna Petrova, Professor of Pediatrics, Department of Pediatrics, Rutgers Robert Wood Johnson Medical School, USA.
Received Date: July 17, 2024; Published Date: September 10, 2024
Abstract
Introduction
Despite compelling evidence showing variations in the prevalence of dyslipidemia and cardiovascular morbidity among different racial and ethnic groups, the impact of cultural diversity on the development of dyslipidemia in children and adolescents remains uncertain. In this study, we investigated whether there is a difference in diagnosing lipid abnormalities in pediatric patients of Hispanic and Asian Indian ethnicity, regardless of their age, gender, and overweight/obesity.
Methods
In this study, pediatric patients of Asian Indian and Hispanic backgrounds who underwent universal lipid screening at primary care settings were included. We collected data on their lipid profiles (total cholesterol, low-density lipoprotein, triglycerides, and high-density lipoprotein), glucose levels, age, gender, health insurance coverage, and weight categories (normal, overweight, and obese). The statistical analysis included descriptive statistics and stepwise logistic regression analysis. Statistically significant difference was defined at P level of <0.05.
Results
This study included 244 Asian Indian and 184 Hispanic adolescents. Among those, 30.8% and 32.1% had acceptable levels of lipid parameters (P=0.74), 30.7% and 35.9% had high dyslipidemia (P=0.71), and 26.6% and 18.3% had borderline dyslipidemia (P=0.09). Multifactorial dyslipidemia was recorded in 7.0% of Asian Indian and 3.3% Hispanic adolescents (P=0.09). The rate of combined dyslipidemia was higher in Hispanic adolescents compared to Asian adolescents (21.2% vs. 12.9%, P<0.03). Regardless of gender and age, overweight/obese Asian Indian and Hispanic adolescents were found to be at increased risk for developing any dyslipidemia.
Conclusion
The results of universal screening in pediatric patients showed that only one-third of the Asian Indian and Hispanic children studied had acceptable lipid levels. The study found that Asian Indian adolescents are at a higher risk for multifactorial dyslipidemia, while Hispanics are more likely to develop combined dyslipidemia, which is strongly associated with being overweight or obese. Further research is needed to fully understand how cultural diversity influences the risk of unhealthy lipid levels in young people.
Keywords:Adolescents; Dyslipidemia type; Asian Indian American; Hispanic; Ethnicity
Introduction
The existing evidence indicates that the development of atherosclerosis can begin during childhood [1-3]. According to the Health and Nutrition Examination Surveys (NHNES), one out of ten children have abnormal levels of low-density lipoprotein (LDL-C) or total cholesterol (TC), [4] and one out of five have abnormal levels of high-density lipoprotein (HDL-C) or other non-HDL-C proteins [5]. The U.S. Preventive Services Task Force (USPSTF) has emphasized the importance of examining whether race and ethnicity affect lipid profile abnormalities in the pediatric population [6]. This focus is likely due to strong evidence indicating racial and ethnic disparities in the prevalence of dyslipidemia and cardiovascular issues among adults in the United States [7-9]. However, the role of racial and ethnic background on the development of dyslipidemia in the general pediatric population remains unclear. Data from NHANES spanning from 1999 to 2016 shows no significant changes in LDL-C and HDL-C levels across different racial and ethnic groups, reduced average TC levels in white but not in black and Mexican children [10]. A study examining lipid screening in pediatric patients from 2007 to 2010 in community practice found a higher prevalence of elevated TC and reduced HDL-C in Hispanic adolescents compared to their white counterparts [11]. Our previous study focused on analyzing the rate and factors associated with different types of dyslipidemia in Asian Indian adolescents who underwent universal lipid screening in the primary care pediatric setting [12]. The current study continues our work to characterize the lipid profile abnormality in culturally diverse pediatric populations, such as Hispanic origin, representing the most significant ethnic minorities in the U.S [13]. The study aimed to compare the occurrence of different types of dyslipidemias in Hispanic to those in Asian Indian adolescents to determine if there is an ethnicity-based difference in the diagnosis of lipid abnormalities, regardless of essential health factors such as age, gender, and childhood overweight/obesity [14- 16]. To the best of our knowledge, such a study is the first to provide new insight into ethnicity-associated risk for the development of dyslipidemia in the U.S. pediatric population of Hispanic and Asian Indian descent. Notably, adults from these ethnic groups have a high prevalence of dyslipidemia and a disproportionately high incidence of cardiovascular morbidity and mortality. [8,9] We hypothesized that there is a difference in the type of dyslipidemias recorded in Asian Indians compared to Hispanic adolescents because of dissimilarities in certain food practices [17] and risk for metabolic syndrome due to differences in socioeconomic status [18] that were predicted by the income eligibility criteria for public health insurance [19]. In the present study, public health insurance covered all Hispanic adolescents. In contrast, private health insurance covers all studied Asian Indian adolescents.
Methods
The precise methods outlined in the previous study [12] were implemented to select Hispanic adolescents and extract relevant data from their medical records. The primary care pediatric setting used to select Asian Indian and Hispanic children were presented in two pediatric offices located in two areas of New Jersey with high concentration of Hispanic and Asian Indian populations. Such two settings have the same electronic system, ensuring consistency in data collection. Medical records of Hispanic patients aged from 10 to 20 years old were selected by the Current Procedural Terminology (CPT) for preventive care office visits (99393, 99394, 99395, 99383, 99384, and 99385). Medical records of selected subjects were verified to obtain demographic (age, gender, health insurance coverage), lipid measurements (TC, LDL-C, TG, and HDL-C), blood sugar, and anthropometric parameters at the time of lipid screening. All collected measurements were added to the existing database of Asian Indian children and adolescents. The same classification of dyslipidemia was used to identify acceptable, borderline, or high levels of dyslipidemia [2,3] by analyzing TC, LDL-C, TG, and HDL-C. If all lipid profile measures were at acceptable levels, adolescents were identified as having normal lipid profiles. Borderline dyslipidemia was classified if TC level was between 170 to 199 mg/dL, LDL-C was between 110 to 129 mg/dL, or TG was between 90 to 129 mg/dL. High dyslipidemia was classified if any single or combination of TC was above 200 mg/dL, or LDL-C was above 130 mg/dL, or TG was above 130 mg/dL, or HDL-C was below 40 mg/dL. The threshold points represented the 95th and 75th percentiles for high and borderline, respectively, and the 10th percentile for low threshold points for HDL-C. We also calculated the ratio of TG/HDL-C to classify combined dyslipidemia (CD) using the cutoff point of 3, which suggested the definition of CD in whites. [20] Additionally, patients with multifactorial dyslipidemia were identified if the TC level was above 200 mg/dL and/or the LDL-C level was above 130 mg/dL [6]. The stages of adolescence life were classified into early (10 to 13 years), middle (14 to 17 years), and late (18 to 21 years) stages. Overweight and obese adolescents were categorized based on sex-age percentile for body mass index (BMI) from 85th to below 95th and 95th and above percentile [21].
Statistical Analysis
We utilized the completed database to conduct a statistical comparison of lipid profiles and other parameters between Asian Indian (Group 1) and Hispanic (Group 2) adolescents. We analyzed lipid profiles in relation to age, gender, and BMI categories. The parameters we analyzed included average blood lipid quantities and dyslipidemia categories. We used chi-square and analysis of variance (ANOVA) to compare categorical and continuous variables, respectively. Additionally, we employed a stepwise logistic regression model to determine the independent association of different types of dyslipidemias with ethnicity (Hispanic vs. Asian Indian), while controlling for age (years), gender (male vs. female), and BMI categories (normal vs. overweight/obesity). Our results are presented as a rate percentage (%), mean with standard deviation, and odds ratios (OR) with a 95% confidence interval (95%CI). We used STATISTICA 13.3 (StatSoft Inc., Tulsa, OK, USA). All statistical tests were two-sided, with the significance level set at a P-value of less than .05.
Result
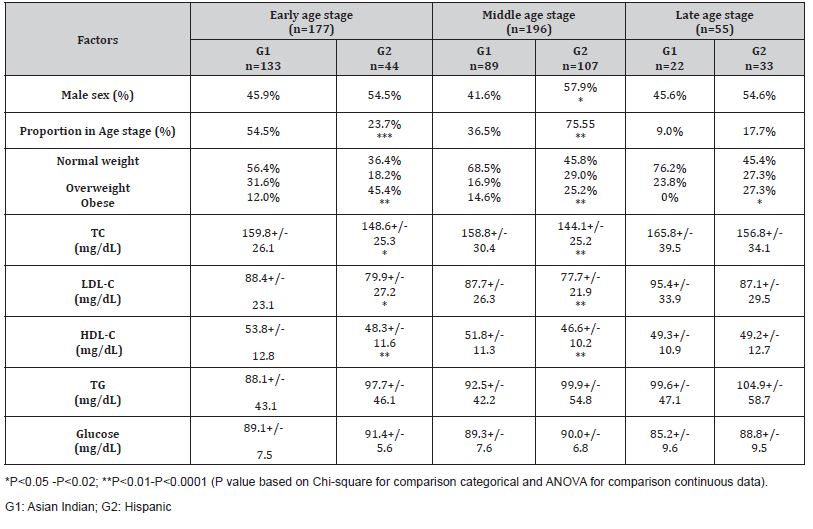
A total of 428 adolescents were studied, comprising 177 (41.4%) at the early age stage, 196 (45.8%) in the middle age stage, and 55 (12.8%) at the late age stage. The study had two groups, Group 1 with 244 Asian Indian adolescents and Group 2 with 184 Hispanic adolescents. All Asian Indian patients in the study were covered by commercial health insurance, while all Hispanic patients were covered by government health insurance. Group 1 had a higher percentage of early age stage adolescents and a lower percentage of middle age stage adolescents than Group 2, as shown in Table 1. The gender in Groups 1 and 2 was comparable in the adolescents of early and late stages, but there was an increased proportion of the middle-aged males in Group 2. A significantly higher proportion of adolescents of any age stage in Group 2 had abnormal BMI than in Group 1. The average blood lipid concentrations of TC, LDL-C, and HDL-C were higher in Group 1 than in Group 2 adolescents in early and middle age stages (Table 1). The average fasting glucose levels were normal in Groups 1 and 2 (Table 1). Only 5.5% (13/236) of adolescents in Group 1 and 7.6% (14/184) in Group 2 had glucose levels between 101 and 128 mg/dL, respectively (P=0.36).
Table 1:Ethnic groups and age stage based comparison of study participants (%, Mean+/-SD)..
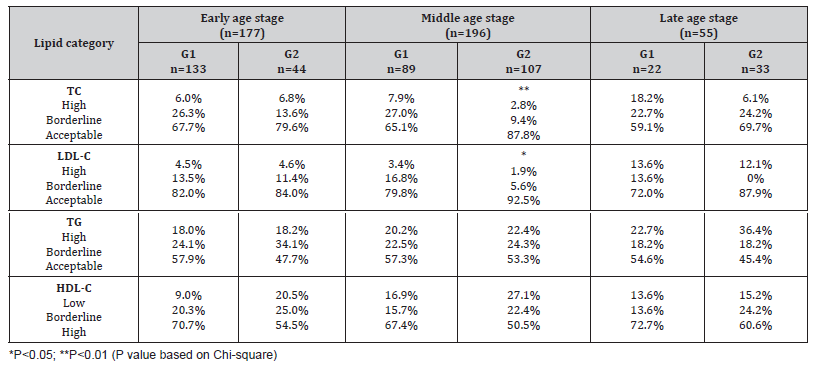
Ethnicity Group-based Comparison of Acceptable Lipid Levels
Overall, 31.6% (n=134) of the children had an acceptable concentration of parameters in their lipid profile, including TC, LDL-C, and TG, as well as HDL-C greater than 40 mg/dL. This percentage was comparable between Group 1 and Group 2 (30.8%, n=75 vs. 32.1%, n=59, P=0.74). Asian Indian adolescents (Group 1) were found to be less likely to have acceptable levels of TC (66.0% vs. 82.6%, P<0.001) and LDL-C (79.9% vs. 89.7%, P<0.01) compared to Hispanic adolescents. However, they were more likely to have HDL levels above 40 mg/dL than Hispanic adolescents (69.8% vs. 53.3%, P<0.01). The study also found a similar rate of acceptable concentration of TG between the two groups (57.4% vs. 50.5%, P=0.33). Further analysis based on age showed that Asian Indian adolescents in their middle age stage had a lower rate of acceptable TC and LDL-C levels compared to Hispanics (Table 2). As shown in Table 2, there was no statistically significant difference in the rates of acceptable TG and HDL levels between Asian Indians and Hispanics of different ages.
Table 2:Ethnic group and age stage analysis of classified lipid profile abnormalities.
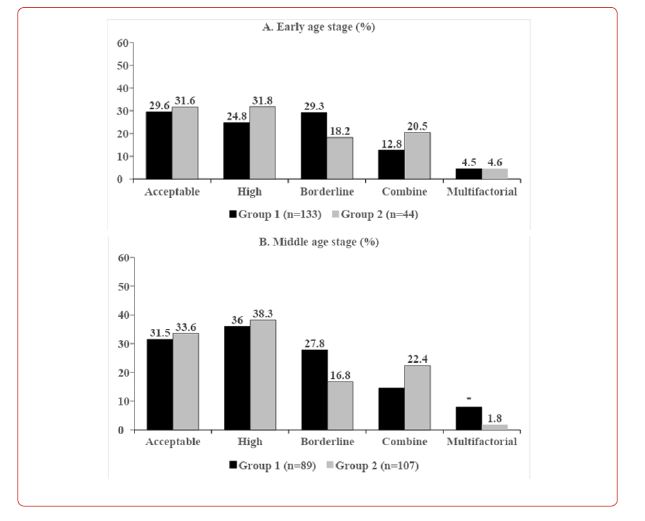
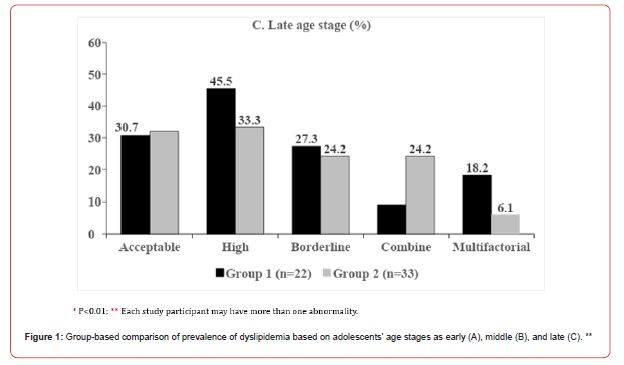
Ethnicity Group-based Comparison of Dyslipidemia Rates
The difference of dyslipidemias rates between Group 1 and Group 2, including high (30.7% vs. 35.9%, P=0.71), borderline (26.6% vs. 18.3%, P=0.09), and multifactorial (7.0% vs. 3.3%, P=0.09) did not reach statistical significance. However, the percentage of combined dyslipidemia was higher in Group 2 at 21.2% compared to 12.9% in Group 1 (P<0.03). Figure 1 (A, B, C) illustrates the comparison of acceptable, high, borderline, combined, and multifactorial dyslipidemias between the two groups across different age stages. At the early age stage, the rates of all dyslipidemias were similar (Figure 1A). Multifactorial dyslipidemia increased in middle-aged adolescents in Group 1 (Figure 1B). When combining data from middle and late age stages, it was found that Group 1 had a higher rate of multifactorial dyslipidemia than Group 2 (10.0% vs. 2.8%, P<0.02).
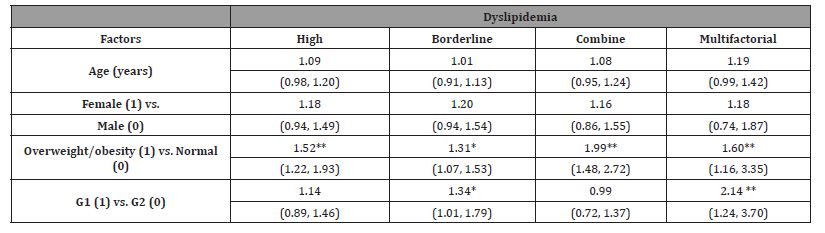
Factors Predicting High, Borderline, Combine, and Multifactorial Dyslipidemias
In our study, we used stepwise logistic regression models to investigate the relationship between various types of dyslipidemias and the ethnicity of the adolescents we studied, while also considering their age and gender as well as their weight category. Our findings, which are outlined in Table 3, revealed that Asian Indian ethnicity was an independent factor associated with a 1.5 times higher chance of developing borderline dyslipidemia and a two times higher chance of developing multifactorial dyslipidemia. Additionally, we found that being overweight or obese significantly increased the likelihood of both Asian Indian and Hispanic adolescents being diagnosed with different types of dyslipidemia. Interestingly, we did not find independent predictive relationships between adolescents’ age and gender and the development of any dyslipidemia.
Table 3:Factors associated with different types of dyslipidemias (OR, 95%CI).
Discussion
This research compares lipid profiles obtained from the universal screening of Asian Indians with those of Hispanic adolescents to determine the impact of ethnicity on the development of different types of dyslipidemia independent of age, gender, and weight categories. It revealed that up to 30% of adolescents in both ethnic groups had lipid levels within the acceptable range. However, Asian Indians were less likely to have acceptable levels of TC and LDL-C but more likely to have high levels of HDL-C compared to Hispanic adolescents. We found that, regardless of age, gender, and overweight/obesity, Asian Indian adolescents are twice as likely to have multifactorial dyslipidemia, with a rate of 10%, compared to 2.8% in Hispanic adolescents. The prevalence of multifactorial dyslipidemia in the general pediatric population is still uncertain. According to the US Preventive Services Task Force (USPSTF) review, the rates of multifactorial dyslipidemia vary widely, ranging from 4.8% to 12.3% [6]. Furthermore, the USPSTF review emphasized the significance of overweight/obesity in causing a multifactorial type of dyslipidemia in children. Our study demonstrated the independent effect of overweight/obesity on the development of not only multifactorial but also borderline, high, and combined dyslipidemias. In our study, we found that the rate of multifactorial dyslipidemia in Hispanic adolescents with and without overweight/obesity was comparable (3.9% vs. 2.5%, P=0.86), while it was elevated in Asian Indians with abnormal BMI (12.1% vs. 4.0%, P<0.02). We will need more data to explain the differences in the role of overweight/obesity in the development of multifactorial dyslipidemia. The variation in the impact of overweight/obesity on multifactorial dyslipidemia occurrence between Hispanic and Asian Indian teenagers in our study may be due to the diversity of dietary practices that limit the intake of polyunsaturated fatty acids [22].
Nevertheless, the impact of overweight/obesity on the development of combined dyslipidemia defined by the TG/HDL-C ratio at a cutoff point of 3 was similar in Hispanic and Asian Indian study participants. High levels of triglycerides (TG) and low highdensity lipoprotein cholesterol (HDL-C) were identified as key components in assessing lipid abnormalities related to overweight/ obesity [23-25]. The significance of an increased TG/HDL-C ratio as a metabolic indicator of insulin resistance has been emphasized in adults [25], including Hispanic men and women [26].
The National Heart, Lung, and Blood Institute (NHLBI) and the American Academy of Pediatrics (AAP) recommended universal lipid screening for children and adolescents, but they noted a lack of evidence for specific recommendations for racial or ethnic groups within the pediatric population [20]. Despite these recommendations, universal screening has not been widely adopted by primary care pediatricians for over a decade. It is predominantly used for obese adolescents and those with a family history of cardiovascular diseases [27]. Data from primary care settings in the Midwest revealed that only 4% of eligible pediatric patients underwent lipid screening [28]. The inadequate implementation of universal lipid screening may be a significant factor that could delay research on dyslipidemia in the culturally diverse pediatric population in the U.S. Additionally, the USPSPF identified insufficient evidence to support the direct benefits of screening for multifactorial dyslipidemia during childhood, [29] even though prevention of cardiovascular diseases should begin in childhood [30].
We acknowledge the limitations of our study, particularly regarding the generalizability of study results restricted by socialeconomic diversity of studied Asian Indian and Hispanic patients who covered by commercial and government-based health insurance, respectively. Furthermore, the varying socioeconomic status of families in these two groups could also impact the obtained findings [31]. It’s important to note that we didn’t consider the racial diversity within the Hispanic ethnicity group or the dietary intake of the participants, which could be crucial factors in dyslipidemia [32,33]. Future research should address these limitations to enhance our understanding of this important issue.
Conclusion
The study discovered that as many as one-third of pediatric patients from Asian Indian or Hispanic backgrounds who underwent universal screening had acceptable lipid levels. In Asian Indian adolescents, the likelihood of identifying multifactorial type dyslipidemia was twice as high as in Hispanic adolescents. Additionally, being overweight or obese increased the risk of developing multifactorial dyslipidemia in Asian Indian patients, but not in Hispanic patients. The study showed that the significant factor in developing combined dyslipidemia is not the patient’s ethnicity, but rather their weight. However, further research is necessary to understand the varying risk factors for dyslipidemia in culturally diverse groups of American youths.
Acknowledgment
The authors would like to acknowledge all of the adolescents who underwent lipid screening in the pediatric practice of My Whole Child Pediatrics.
Conflict of Interest
None.
References
- H C McGill Jr, C A McMahan, E E Herderick, G T Malcom, R E Tracy, et al. (2000) Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr. 72(5Suppl): 1307S-1315S.
- Lloyd-Jones DM, Yuling Hong, Darwin Labarthe, Dariush Mozaffarian, Lawrence J Appel, et al. (2010) Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 121(4): 586-613.
- Steinberger J, Stephen R Daniels, Nancy Hagberg, Carmen R Isasi, Aaron S Kelly, et al. (2016) Cardiovascular health promotion in children: challenges and opportunities for 2020 and beyond: a scientific statement from the American Heart Association. Circulation 134(12): e236-e255.
- Kit BK, Margaret D Carroll, David A Lacher, Paul D Sorlie, Janet M DeJesus, et al. (2012) Trends in serum lipids among US youths aged 6 to 19 years, 1988-2010. JAMA 308(6): 591-600.
- Kit BK, Elena Kuklina, Margaret D Carroll, Yechiam Ostchega, David S Freedman, et al. (2015) Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999-2012. JAMA Pediatr 169(3): 272-279.
- Lozano P, Nora B Henrikson, Caitlin C Morrison, John Dunn, Matt Nguyen, et al. (2016) Lipid screening in childhood and adolescence for detection of multifactorial dyslipidemia: evidence report and systematic review for the US Preventive Services Task Force. JAMA 316(6): 634-644.
- Pu J, Zhao B, Azar KM, Hastings KG, Nimbal V, et al. (2015) Dyslipidemia in special ethnic populations. Cardiol Clin 33(2): 325-333.
- Frank ATH, Beinan Zhao, Powell O Jose, Kristen M J Azar, Stephen P Fortmann, et al. (2014) Racial/ethnic differences in dyslipidemia patterns. Circulation 129(5): 570-579.
- Singh V, Deedwania P (2006) Dyslipidemia in special populations: Asian Indians, African Americans, and Hispanics. Curr Atheroscler Rep 8(1): 32-40.
- Perak AM, Hongyan Ning, Brian K Kit, Sarah D de Ferranti, Linda V Van Horn, et al. (2019) Trends in levels of lipids and Apolipoprotein B in US youths aged 6 to 19 years, 1999-2016. JAMA 321(19): 1895-1905.
- Margolis KL, Louise C Greenspan, Nicole K Trower, Matthew F Daley, Stephen R Daniels, et al. (2014) Lipid screening in children and adolescents in community practice: 2007 to 2010. Circ Cardiovasc Qual Outcomes 7(5): 718-726.
- Mehrotra N, Mehrotra N, Petrova A (2021) Prevalence and factors associated with dyslipidemia in otherwise healthy Asian Indian American Adolescents. Int J Child Adolesc Health 14(3): 253-260
- Quick Facts: United States, Population Estimates. [(accessed on 28 May, 2024)];2019 Available online: https://www.census.gov/quickfacts/fact/table/US/PST045219
- Elmaoğulları S, Tepe D, Uçaktürk SA, Karaca Kara F, Demirel F, et al. (2015) Prevalence of dyslipidemia and associated factors in obese children and adolescents. J Clin Res Pediatr Endocrinol 7(3): 228-234.
- American Academy of Pediatrics. Ages & Stages. Healthy Children. (accessed August 11, 2020).
- Centers for Disease Control and Prevention. Defining Childhood Obesity. Published July 3, 2018. (accessed August 11, 2020).
- USDA ERS- Racial and ethnic diversification will likely shape U.S. food demand and diet quality by Diansheng Dong and Hayden Stewart. April 04, 2022.
- Puolakka E, Katja Pahkala, Tomi T Laitinen, Costan G Magnussen, Nina Hutri-Kähönen, et al. (2016) Childhood socioeconomic status in predicting metabolic syndrome and glucose abnormalities in adulthood: The cardiovascular risk in young Finns study. Diabetes Care 39(12): 2311-2317.
- Barnett JC, Berchick, ER (2017) Health insurance coverage in the United States 2016: Current population reports. U.S. Government Printing Office; U.S. Department of Commerce; Washington, DC, USA: 2017. pp. 60-260.
- Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011 Dec;128 Suppl 5(Suppl 5): S213-56.
- Centers for Disease Control and Prevention. Defining Childhood Obesity. Published July 3, 2018. (accessed August 11, 2020).
- Fernandez ML, West KL (2005) Mechanisms by which dietary fatty acids modulate plasma lipids. The Journal of Nutrition 135(9): 2075-2078.
- Tabas I, Williams KJ, Boren J (2007) Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation 116(16): 1832-44.
- Berenson GS, Srinivasan SR, Bao W, Newman WP III, Tracy RE, et al. (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: the Bogalusa Heart Study. N Engl J Med 338(23): 1650-1656.
- Magnussen CG, Raitakari OT, Thomson R, Markus Juonala, Dharmendrakumar A Patel, et al. (2008) Utility of currently recommended pediatric dyslipidemia classifications in predicting dyslipidemia in adulthood: evidence from the Childhood Determinants of Adult Health (CDAH) study, Cardiovascular Risk in Young Finns Study, and Bogalusa Heart Study. Circulation 117(1): 32-42.
- Michael J Barry, Wanda K Nicholson, Michael Silverstein, David Chelmow, Tumaini Rucker Coker, et al. (2016) Screening for lipid disorders in children and adolescents: U.S. Preventive Services Task Force Recommendation Statement. JAMA 330(3): 253-260.
- de Ferranti SD, Rodday AM, Parsons SK, William L Cull, Karen G O Connor, et al. (2017) Cholesterol screening and treatment practices and preferences: a survey of United States pediatricians. J Pediatr 185: 99-105.
- Allen-Tice C, Steinberger J, Murdy K, Zierhu H (2020) Pediatric cholesterol screening practices in 9- to 11-year-olds in a large midwestern primary care setting. J Clin Lipidol 14(2): 224-230.
- Michael J Barry, Wanda K Nicholson, Michael Silverstein, David Chelmow, Tumaini Rucker Coker, et al. (2016) Screening for lipid disorders in children and adolescents: U.S. Preventive Services Task Force Recommendation Statement. JAMA 330(3): 253-260.
- Berenson GS, Srinivasan SR, Bao W, Newman WP III, Tracy RE, et al. (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: the Bogalusa Heart Study. N Engl J Med 338(23): 1650-1656.
- Hartz JC, Yellen E, Baker A, Zacariah J, Ryan H, et al. (2019) The relationship between payer type and lipid outcomes in response to clinical lifestyle interventions in youth with dyslipidemia. BMC Pediatr 19(1): 217.
- Gary D. Sandefur, Mary E. Campbell, and Jennifer Eggerling-Boeck. Racial and ethnic identification, official classifications, and health disparities. Critical perspectives on racial and ethnic differences in health in late life. Editors: Norman B Anderson, Rodolfo A Bulatao, and Barney Cohen. National Research Council (US) Panel on Race, Ethnicity, and Health in Later Life. Washington (DC): National Academies Press (US); 2004.
- Khoury M, Manlhiot C, Gibson D, Chahal N, Stearne K, et al. (2016) Universal screening for cardiovascular disease risk factors in adolescents to identify high-risk families: a population-based cross-sectional study. BMC Pediatr 16: 11.
-
Naveen Mehrotra and Anna Petrova*. The Difference in Patterns of Dyslipidemia in The U.S. Hispanic and Asian Indian Adolescents. Glob J of Ped & Neonatol Car. 5(2): 2024. GJPNC.MS.ID.000606.
Adolescents, Dyslipidemia type, Asian Indian American, Hispanic, Ethnicity, General pediatric, Dissimilarities, Overweight/obesity, Teenagers
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






