 Case Report
Case Report
Presentation of an Unsuspected Tuberculosis with Intracranial and Extracranial Manifestations in an Adolescent Female: A Case Report
Oluniyi S Afolabi1*, Moataz Elghazouly1, Ahmed Mohamed Ezzeldeen Mahmoud1 and Ayidh Saad Ayidh Alharthi2
1Department of Radiology, King Fahad Hospital, Kingdom of Saudi Arabia
2Department of Paediatrics, King Fahad Hospital, Kingdom of Saudi Arabia
Oluniyi S Afolabi, Department of Radiology, King Fahad Hospital, Al Baha, Kingdom of Saudi Arabia.
Received Date: September 06, 2022; Published Date: September 20, 2022
Abstract
Introduction: Tuberculosis is known to be endemic in Asia, Africa and Eastern Mediterranean, and it is known to be common among the paediatric population, with its subsequent potential extrapulmonary manifestations.
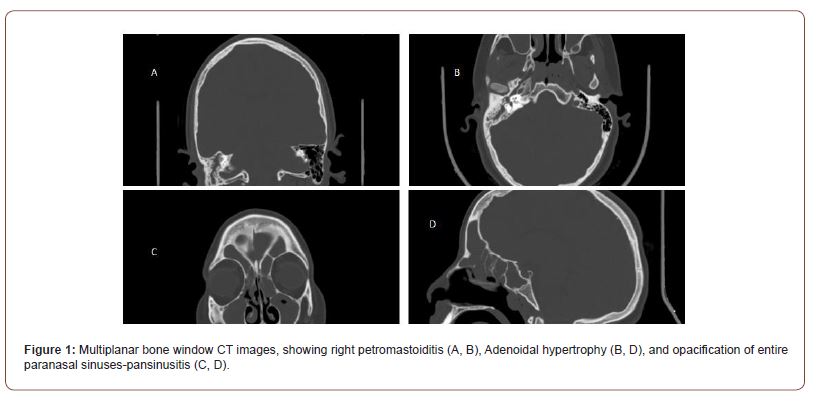
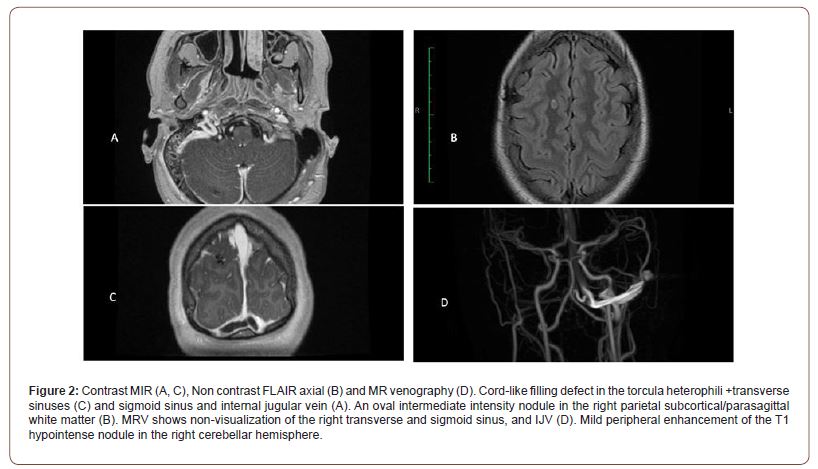
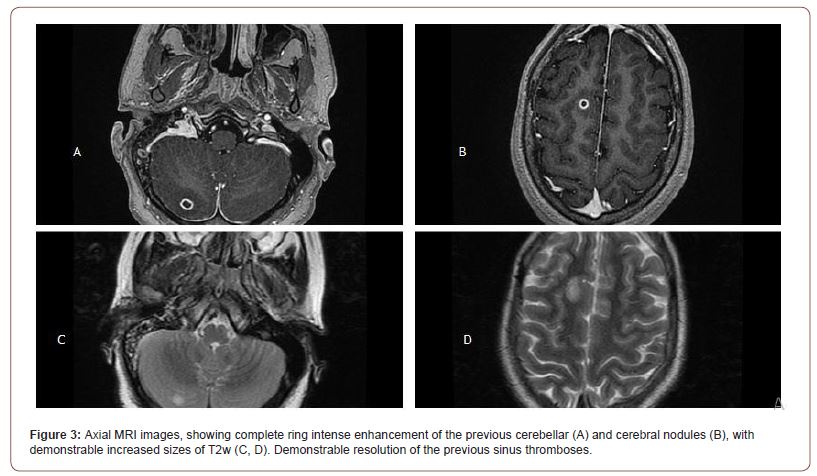
Case presentation: This is a case of a 13year year old girl with headache, eye ache, photophobia, ear pain and bilateral partial deafness. Her initial blood workup showed leucocytosis, neutrophilia and lymphocytopaenia, as well as decreased APTT and raised fibrinogen level. Initial CT showed pansinusitis, right petromastoiditis and adenoidal hypertrophy, while an initial MRI showed an additional venous sinus thrombosis, as well as right sided supratentorial and infratentorial mildly enhancement nodules. A follow-up MRI then showed an increase in size and complete ring intense enhancement of these cerebral and cerebellar nodules. An additional high-resolution CT showed a large right lung lower lobe thickwalled cavity. Thus, raising the suspicion of intracranial chronic granulomatous lesions. A positive PCR Tuberculosis screening test was eventually demonstrated and there was a significant resolution of the lesions on follow-up imaging after treatment.
Conclusion: This article was aimed at showing the need for a high index of suspicion for tuberculosis, in paediatric age group, especially when there are multiple/overwhelming septic foci, as well as other unusual presentations, such as venous sinus thrombosis.
Keywords: Adolescent; Tuberculoma; Venous thrombosis; Pansinusitis; Ring lesions
Introduction
Tuberculosis, caused by mycobacterium tuberculosis bacillus remains a highly dangerous global infection, as it is the second cause of death from infection after Human Immunodeficiency Virus (HIV) [1]. This is more prevalent in the most endemic regions, which are Asia, Africa and Eastern Mediterranean. There has been increased in the incidence of tuberculosis in children, due to the co-existence with HIV [2]. Paediatric tuberculous infection can be as high as twenty percent, and this could be more in the endemic regions. Potential life-threatening disease is commoner in infancy and early childhood [3]. Tuberculosis among adolescent usually present with adult-type disease, which usually affect the upper lobe’s apical and posterior segments and may eventually progress to cavitation and bronchial dissemination [2]. A local study has shown a higher prevalence among adolescent, when compared with younger age group, and also among foreign-born patients, in a basically non-endemic region [4]. Central nervous tuberculosis, in the form of tuberculous meningitis is the third commonest presentation of extrapulmonary disease in paediatric patients, after lymphadenopathy and pleural effusion [5]. Tuberculoma is a common presentation of central nervous system (CNS) manifestation of tuberculosis, aside tuberculous meningitis which is usually complicated by infarction [6]. Tuberculosis meningitis has thus been linked with poor prognosis [5,6].
Case Presentation
A previously healthy 13year old girl presented at the Emergency room on account of headache, eye pain, photophobia and ear pain of two weeks duration. There were also tinnitus and decreased hearing in the left ear. The ear pain was initially left sided, but later became bilateral. She was a product of an uneventful full-term pregnancy but had left Erb’s palsy since birth. No history of fever, seizures or loss of consciousness. She completed routine paediatric immunisation and had normal development. The initial physical examination revealed an acutely ill-looking girl. No fever. No pallor. No neurological deficit.
Initial Ophthalmic assessment revealed bilateral optic disc swelling with papilloedema grade 3-4. Preserved colour vision. Pure tone average (PTA) audiometry assessment revealed bilateral hearing loss- mild in the right ear and moderate in the left ear.
Her complete blood count showed leucocytosis, neutrophilia and lymphocytopaenia at presentation. Liver function test, renal function test and bone profile were all within normal ranges. Ear swab showed no growth. The initial APTT was decreased, and fibrinogen was elevated.
She had an initial non contrast CT scan which showed gross pansinusitis, right petro-mastoiditis and adenoidal hypertrophy (Figure 1). She later had a Contrast Magnetic Resonance Imaging (MRI) with Magnetic Resonance Venography (MRV) within 24hours of presentation. This showed venous thrombosis of the right transverse and sigmoid sinus, as well as the internal jugular vein (IJV). In addition, there was solitary nodule in each of right frontal subcortical white matter and right cerebellar hemisphere. Each nodule appeared hypointense on T1, intermediate to slight hyperintensity on T2, and hyperintense FLAIR images. They show faint/minimal contrast enhancement to gadolinium, with a corresponding ADC/DWI restricted diffusion. An initial assumption of supratentorial and infratentorial venous subacute infarcts, likely from right sided venous sinus thromboses was made (Figure 2), in addition to the previously noted petromastoiditis and pansinusitis. The patient had a follow up contrast MRI in about three weeks after the initial imaging. This showed increased size of the initial right cerebral and cerebellar nodules, which now revealed well-defined avid peripheral ring enhancement (Figure 3). These findings thus, raised the suspicion of possible granulomatous condition, rather than abscesses or infarcts.
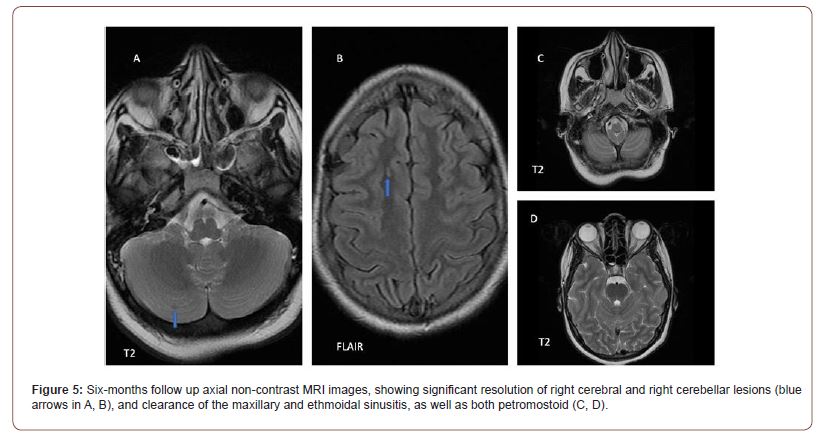
She was subsequently commenced on anti-tuberculous treatment, using Isoniazid, Rifampicin, Pyrazinamide and Levofloxacin. Other supplementary medications such as pyridoxine and Vit D3 were also added. Daily subcutaneous Clexane was commenced, for an initial 2months. Patient was to present at the follow-up clinic in four weeks, for the review of her clinical and laboratory parameters. A six-month follow up non-contrast MRI showed resolution of the right cerebellar lesion which now appears signal void on all sequences, suggestive of calcific foci. The right frontal lesion appears as a slit-like FLAIR/T2 hyperintensity, when compared with the previously large lesion with moderate perilesional oedema at initial presentation (Figure 5).
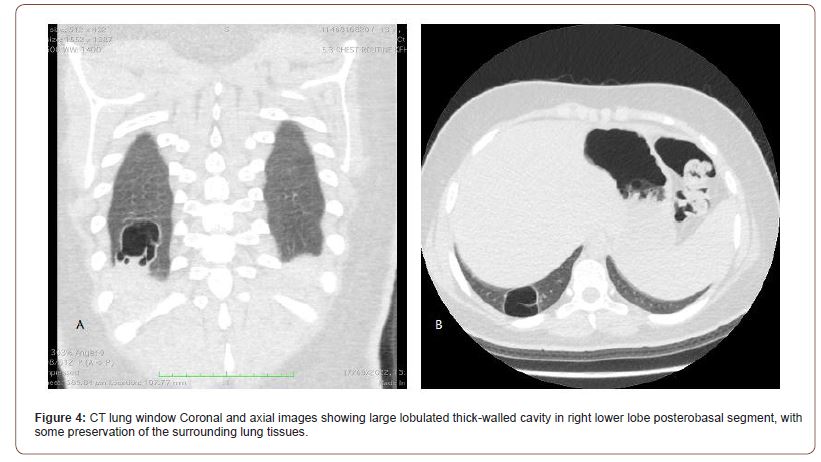
She then had cerebrospinal fluid analysis and culture, sputum Acid-fast bacilli staining, Toxoplasmosis/CMV/HIV/ Torches screening, which were all negative. She eventually had a Tuberculosis screening by PCR, which was positive. She also had a chest CT, which showed a right lower lobe thick-walled large cavity with an apparently clear/normal surrounding lung tissue, suggestive of a chronic status. (Figure 4).
Discussion
CNS tuberculosis, being a major presentation of extrathoracic infection, is fundamentally demonstrated as Tuberculous meningitis and tuberculoma, which had been reported to show 19.2% and 2.8% respectively of the paediatric extrathoracic manifestation of the disease [2]. Wasay M. et al however documented a significantly higher presentation of tuberculoma than tuberculous meningitis among adult population. This report also documented associated infarcts in 25% of the studied adult population [6], which could justify the initial consideration of supratentorial and infratentorial infarcts in the index case.
Similar to the case under review, who presented with headache and cerebellar tuberculoma, among other imaging findings, Israr et al reported a case of cerebellar tuberculoma in an 8year old with a sole complaint of headache [7]. Tuberculous sinuses had been reported in adults, which mainly affects the maxillary sinus, unlike in this particular adolescent who presented with pansinusitis and mastoiditis [8,9]. More so, cases of intracranial venous sinus thrombosis and extracranial deep vein thrombosis (DVT) had been documented in known intracranial and pulmonary tuberculosis in adult patients. Fiorot Junior et al showed intracranial venous sinus thrombosis [10], while H. Kouismi et al demonstrated extracranial DVT with laboratory confirmation of hypercoagulable states [11]. Similarly, an uncommon thrombosis of the internal jugular vein had been reported in a toddler with a disseminated tuberculosis [12].
Phaneendra Kolla had been able to report tuberculoma has the second commonest cause of ring enhancing brain lesion, after cysticercosis, as he was able to demonstrate the relevance of CT imaging in assessing brain lesions, especially in paediatric cases [13].
Conclusion
Multifocal tissue infections with co-existing multiple intracranial ring enhancing lesions should raise the suspicion of a potential granulomatous condition, especially tuberculosis in endemic areas and among the paediatric age group.
Funding
None.
Conflicts of Interest/Competing Interests:
None declared by each of the authors.
Consent to Participate
Consent obtained from the parents of the patient, having been assured of complete confidentiality.
Author’ Contributions
Each of the authors substantially contributed to the conceptualization, design, acquisition of data and analysis/ interpretation of the acquired patient’s data for the purpose of this publication. They all have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Ramachandran G, Swaminathan S (2014) Tuberculosis. Handbook of Pharmacogenomics and Stratified Medicine. Elsevier Inc, pp. 835-857.
- Marais BJ, Schaaf HS (2014) Tuberculosis in Children. Cold Spring Harb Perspect Med. Cold Spring Harbor Laboratory Press 4: 1-22.
- Esposito S, Tagliabue C, Bosis S (2013) Tuberculosis in Children. Mediterr J Hematol Infect Dis 5(1): 1-8.
- Winston CA, Menzies HJ (2012) Pediatric and Adolescent Tuberculosis in the United States, 2008-2010. Pediatrics 130(6): e1425-1432.
- Maltezou HC, Spyridis P, Kafetzis DA (2000) Extra-pulmonary tuberculosis in children. Arch Dis Child 83(4): 342-346.
- Wasay M, Farooq S, Khowaja ZA, Bawa ZA, Ali SM, et al. (2014) Cerebral infarction and tuberculoma in central nervous system tuberculosis: Frequency and prognostic implications. J Neurol Neurosurg Psychiatry 85(11): 1260-1264.
- Israr Khan D, Anas M, Khan AA, Khan S (2019) Chronic Headache: The Only Manifestation of Cerebellar Tuberculoma. Biosci Biotechnol Res Asia 16: 711-714.
- Yeon Kim K, Ho Bae J, Soo Park J, Lee SS (2014) Case Report Primary sinonasal tuberculosis confined to the unilateral maxillary sinus. Int J Clin Exp Pathol 7(2): 815-818.
- Kant S, Srivastava R, Verma A, Singh H, Singh S, et al. (2013) Maxillary Sinus Tuberculosis: Various Presentations. Indian J Chest Dis Allied Sci 55(3): 175-177.
- Fiorot Junior JA, Felício AC, Fukujima MM, Rodrigues CA, Morelli VM, et al. (2005) Tuberculosis: An uncommon cause of cerebral venous thrombosis? Arq Neuropsiquiatr 63(3B): 852-854.
- Kouismi H, Laine M, Bourkadi JE, Iraqi G (2013) Association deep veinous thrombosis with pulmonary tuberculosis. Egypt J Chest Dis Tuberc 62(3): 541-543.
- Das S, Srinivasaraghavan R, Krishnamurthy S, Mahadevan S (2014) Internal jugular vein thrombosis complicating disseminated tuberculosis in a 2-year-old child. BMJ Case Rep 1-3.
- Kolla P (2020) A study on CT evaluation of ring enhancing lesions of brain. Int j Radiol Diagn Imaging 3(1): 195-197.
-
Oluniyi S Afolabi*, Moataz Elghazouly, Ahmed Mohamed Ezzeldeen Mahmoud and Ayidh Saad Ayidh Alharthi. Presentation of an Unsuspected Tuberculosis with Intracranial and Extracranial Manifestations in an Adolescent Female: A Case Report. Glob J of Ped & Neonatol Car. 4(1): 2022. GJPNC.MS.ID.000579.
Adolescent, Tuberculoma, Venous thrombosis, Pansinusitis, Ring lesions, Tuberculosis, Cerebellar nodule, Headache, MRI, Hyperintensity, Infection, Manifestation, Adult population
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






