 Research Article
Research Article
PICC Line in Neonates: Indications and Complications. A Single Level 3 NICU Experience in the UAE and Review of Literature
Nisha Viji Varghese*, Dr. Omar Abu Sa’ada, Uzma Afzal, Nusrat Khan, Dr. Ahmed El Hadidi, Dr. Aiman Rahmani and Zohra Siwji
Department of Pediatrics, Tawam Hospital, UAE
Nisha Viji Varghese, Neonatal unit, Department of Pediatrics, Tawam Hospital, UAE.
Received Date: January 05, 2021; Published Date: January 22, 2021
Introduction
Central venous catheters (CVCs) are essential in Neonatal Intensive care Units (NICUs) and are commonly used to provide fluids, medications and Parenteral Nutrition (PN) to critically ill infants, especially Very Low Birth Weight (VLBW) and very preterm infants, in line with the practice of minimal handling, allowing longer dwell
Methods
A retrospective chart review for the indications and the major PICC related complications in newborns was conducted for the fiveyear period [January 1st, 2014 to December 31st, 2019].
Inclusion criteria were all babies admitted to our NICU who underwent PICC insertion.
For all the babies, the following data were entered into a computerized database: 1] age; 2] sex; 3] gender; 4] gestation; 5] age at time of insertion of PICC line; 6] indications for PICC insertion; 7] number of days of PICC use; 8] reason for line removal; 9] site of insertion; 10] any adjustment done post insertion of PICC line; 11] number of X-rays needed to confirm the PICC line position; 12] age at which baby developed complications in relation to PICC line; 13] if the line was removed as soon as the complication occurred; 14] any positive culture for late onset sepsis [blood, urine, CSF] during the time PICC line remained in situ.
Extreme preterm babies were defined as those babies less than or equal to 27+6 weeks, very preterm babies between 28+0 weeks and 32+6 weeks, preterm babies as those between 33+0 to 34+6 weeks, late preterm babies as those between 35+0 to 36+6 weeks, early term babies between 37+0 to 38+6 weeks, term babies between 39+0 to 40+6 weeks and post term above or equal to 41+0 weeks.
Indications for PICC line insertion were sub-classified into: 1] babies in whom UVC insertion failed at birth [or] UVC was removed due to malposition/duration exceeding 14 days of remaining in place; 2] babies who received prolonged TPN exceeding 1 week without evidence of NEC such as in surgical conditions like short bowel syndrome, gastroschisis; 3] babies who received TPN as the baby was kept NPO due to NEC; 4] babies who received antibiotics for sepsis [or] other medications such as Prostin; 5] difficult peripheral venous cannulation; 6] cases of hypoglycaemia when infusions of dextrose exceeding 12.5% was needed.
PICC line insertion sites were categorized into those inserted into upper extremity [or] lower extremity and further subclassified as per the anatomical landmarks. Data regarding all nonselective removals were collected from all the neonates. Catheter tips were defined as central at the time of placement if they were in the superior vena cava (SVC), right atrium (RA), or high inferior vena cava (IVC), at or above the level of the diaphragm, and as non-central if located elsewhere [5]. The complications audited included leakage at the PICC insertion site, phlebitis (erythema, swelling, pain, or palpable cord), infection (positive blood cultures, urine cultures, CSF cultures), catheter occlusion (inability to infuse or withdraw), pleural/pericardial effusion, cardiac arrhythmias, ascites and mechanical malfunction (catheter damage/catheter breakage). Malposition was defined as catheter tip beyond cavoatrial junction in PICC of upper limb, renal veins [L2 vertebra] in PICC of lower limb after the catheter was initially placed in an optimal position and later migrated to an undesirable position [5]. Duration of PICC line was defined as the time interval between insertion of PICC and removal of the same.
Statistical Analysis
The data analysis was performed using the SPSS software. The statistical tests applied were the Chi square test and Fischer’s exact test using which ‘p’ value was calculated and value of <0.05 was considered to be statistically significant.
Results
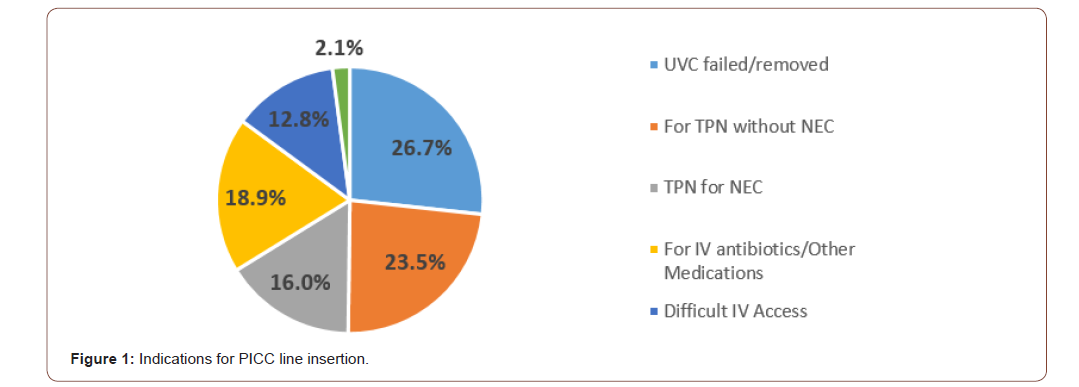
During the study period, 243 PICC lines were inserted in our NICU patients. Eighty two percent of the babies were nationals. The mean weight was 1398gms with SD of 856gms (Range 370gms – 4140gms), while the median was 1100gms (IQR 1250gms). The mean gestation was 29.8 weeks with SD of 5.1 weeks (Range: 22 weeks to 41 weeks), and the median for gestational age was 29 weeks (IQR 9 weeks). PICC line was inserted predominantly in extreme preterm babies who formed almost 43% of all gestations. The mean age at the time of insertion was around 13 days with a median of 6 days [IQR 12 days], whereas the mean duration of PICC line was 15 days (R 0-125 days) with a median of 10 days [IQR 14 days]. Figure 1 shows the indications for insertion of PICC line and most commonly was due to failed UVC insertion [or] when the baby needed prolonged central access necessitating replacement of UVC with a PICC line [26%].
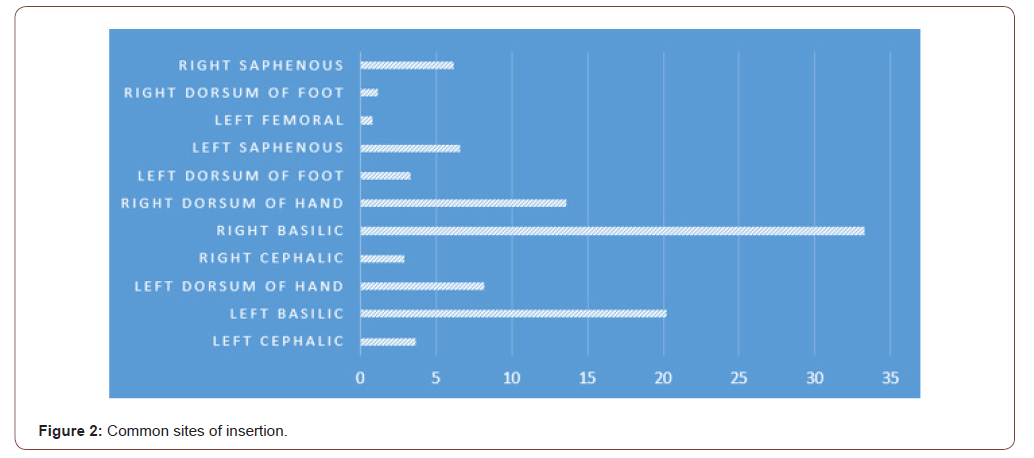
Eighty-two percent of the PICC Lines were inserted in upper limbs as shown below in Figure 2; mostly on right side and the most common site was the Basilic veins of either side followed by the veins on dorsal hand (Figure 3).
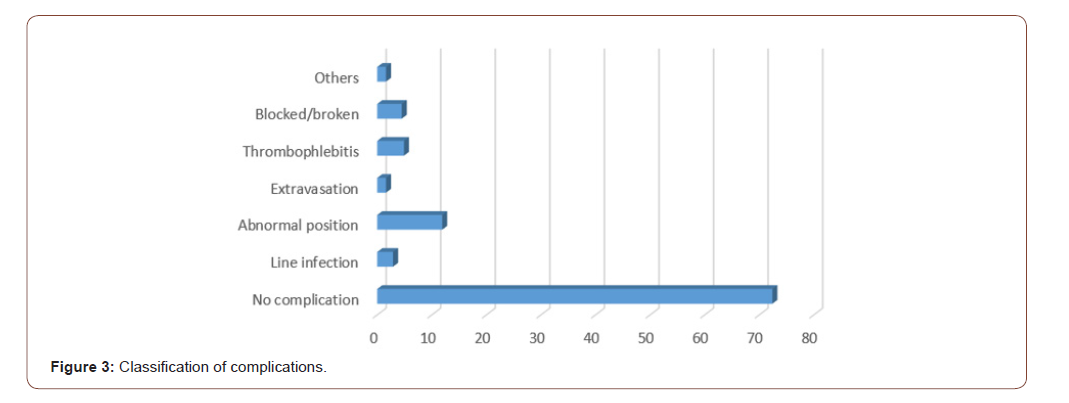
The most common complication was abnormal position of PICC line [43%] followed by thrombophlebitis/erythema of skin around the PICC line [18%]. Line occlusion/line breakage was found to constitute 16% of total complications. Infectious complications occurred in 10% while extravasation and arrhythmias occurred in another 10%.
In 66% of line insertions, only one X-ray was done to confirm the position of PICC line, whereas in 26% cases, a 2nd X-ray was needed. 5-7% of the babies needed more than 2 X-rays for final confirmation of PICC line position following adjustment and fixing. Though true line associated infection occurred only in 7 cases, total of 63 neonates had a positive culture [blood/CSF/urine].
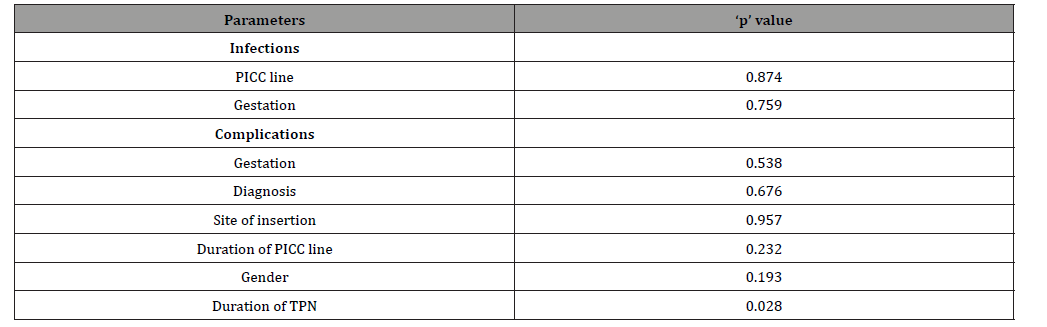
No association was found between PICC line position and infection [P=0.87], gestation and infection [P=0.75], gestation and complications [P=0.53], diagnosis and complication [P=0.67], site of insertion and complication [P=0.95], duration of PICC line and complication [P=0.23], gender and complication [P=0.19]. However, there was significant correlation noted between duration of TPN and complication [P=0.02] (Table 1).
Table 1:
Discussion
Vascular access in neonates plays a pivotal role in management but is technically challenging [7]. PICC has been used extensively due to the advantage of being placed at the bedside without general anesthesia and remaining in situ for days or weeks with minimal mechanical complications [7]. Janes et al. [5] concluded that PICCs used in VLBW infants significantly reduced IV insertions and needle punctures without adding morbidity. In contrast to central catheters, PICC lines are less invasive and have lower morbidity and mortality [7]. The overall incidence of complications varies widely among studies, ranging between 25-50% [8-10]. Our study showed that 74.8% of our babies who received PICC insertion were preterm babies, which is comparable to most studies where the median gestation receiving PICC insertions were 28 weeks as was ours [11]. The common site of insertion was the upper limbs as shown in other studies [1]. The optimal position remains controversial, but the consensus is that it should rest at the junction of superior vena cava [SVC] and the right atrium [RA] if inserted from the upper extremity and below the level of the renal veins if inserted from the lower extremity [12-14]. The location between the SVC and RA ensures a proximal position with high blood flow which prevents thrombosis [especially of concern with parenteral nutrition solutions and chemotherapeutic agents] and yet lies outside the atrium and thus prevents arrhythmias from catheter tip irritation of the right atrial wall [15]. Some authors have classified the subclavian vein as a central position for the catheter tip [2,12]. There was no difference in the rate of complications among PICC line placed in the upper limb compared to the lower limb in our study. A standard chest radiograph traditionally assesses the tip position. In majority of patients, the tip moves caudally by at least 2 cm on arm adduction, though this study population included adults [16]. PICC tips also move cranially by an average of 2 cm on changing position from adduction to abduction though this was mostly again in adults [16]. It has been suggested that the PICC lines placed on the right arm moves more than those placed in the left arm. Malposition were also noted to be more common in the upper extremities in few studies done in neonates [3]. Malposition may trigger arrhythmias either during [or] after insertion of PICC line [15, 17]. Rarely, malposition causes cardiac tamponade, which may be fatal [18, 15]. However, there is no clear evidence in the literature indicating the association of catheter tip position and complication rates in neonatal PICCs [2]. Some pediatric studies have found that PICCs placed in non-central veins provided safe and reliable intravenous access, whereas others have suggested that PICCs terminating in non-central venous positions have higher risks of complication [3]. Nevertheless, these studies cannot be easily compared due to inconsistent definitions of central veins. The positive association between duration of TPN and complications [P=0.02] may in fact be attributed to the migration of PICC tips to non-central locations despite positioning the catheter tip optimally at the time of insertion. This highlights the important fact that position of PICC line should be confirmed in all patients immediately following insertion and if the tip is not in the correct position, it should be correctly repositioned before starting TPN [19-25]. In most cases TPN was used longer than the PICC duration itself due to underlying surgical conditions [or] for infectious reasons. Our analysis did not show any correlation between complications and gestation/gender/PICC line position/ duration of PICC line [26-31].
Conclusion
Adequate precautions should be taken, and position must be confirmed during and after PICC line insertion to avoid undue complications. Risk factors and etiologies are multifactorial.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Xiaohe Yu, Shaojie Yue, Mingjie Wang, Chuanding Cao, Zhengchang Liao, et al. (2018) Risk Factors Related to Peripherally Inserted Central Venous Catheter Nonselective Removal in Neonates Biomed Res Int 2018: 3769376.
- RA Bashir, A Callejas, H Osiovich, JY Ting (2014) Major PICC Complications in a Neonatal Intensive Care Unit (NICU): A Five Year Review. Paediatrics & Child Health 19(6): e57.
- Pet GC, Eickhoff JC, McNevin KE, Do J, McAdams RM (2020) Risk factors for peripherally inserted central catheter complications in neonates. J Perinatol 40(4): 581-888.
- Panagiotounakou P, Antonogeorgos G, Gounari E, Papadakis S, Labadaridis J, et al. (2014) Peripherally inserted central venous catheters: Frequency of complications in premature newborn depends on the insertion site. J Perinatol 34(6): 461-463.
- Singh A, Bajpai M, Panda SS, Jana M (2014) Complications of peripherally inserted central venous catheters in neonates: Lesson learned over 2 years in a tertiary care center in India. Afr J Paediatr Surg 11(3): 242-247.
- Ainsworth SB, Clerihew L, McGuire W (2007) Percutaneous central venous catheters versus peripheral cannulae for delivery of parenteral nutrition in neonates. Cochrane Database Syst Rev (3): CD004219.
- Jumani K, Advani S, Reich NG, Gosey L, Milstone AM (2013) Risk factors for peripherally inserted central venous catheter complications in children. JAMA Pediatrics 167(5): 429-435.
- Janes M, Kalyn A, Pinelli J, Paes B (2000) A randomized trial comparing peripherally inserted central venous catheters and peripheral intravenous catheters in infants with very low birth weight. J Paediatr Surg 35(7): 1040-1040.
- Crowley JJ, Pereira JK, Harris LS, Becker CJ (1997) Peripherally inserted central catheters: Experience in 523 children. Radiology 204(3): 617-621.
- Thiagarajan RR, Ramamoorthy C, Gettmann T, Bratton SL (1997) Survey of the use of peripherally inserted central venous catheters in children. Pediatrics 99(2): E4.
- Rani A Bashir, Allison M Callejas, Horacio C Osiovich, Joseph Y Ting (2017) Percutaneously Inserted Central Catheter-Related Pleural Effusion in a Level III Neonatal Intensive Care Unit: A 5-Year Review (2008-2012). JPEN J Parenter Enteral Nutr 41(7): 1234-1239.
- Racadio JM, Doellman DA, Johnson ND, Bean JA, Jacobs BR (2001) Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics 107(2): E28.
- Harako ME, Nguyen TH, Cohen AJ (2004) Optimizing the patient positioning for PICC line tip determination. Emerg Radiol 10(4): 186-189.
- Bivins MH, Callahan MJ (2000) Position dependent ventricular tachycardia related to peripherally inserted central catheter. Mayo Clin Proc 75(4): 414-416.
- Orme RM, Mc Swiney MM, Chamberlain-Webber RF (2007) Fatal cardiac tamponade as a result of a peripherally inserted central venous catheter. A case report and review of literature. Br J Anaesth 99(3): 384-388.
- Schuster M, Nave H, Piepenbrock S, Pabst R, Panning B (2000) The carina as a landmark in central venous catheter placement. Br J Anaesth 85(2): 192-194.
- PE Collier, GB Goodman (1995) Cardiac tamponade caused by central venous catheter perforation of the heart: a preventable complication. J Am Coll Surg 181(5): 459-463.
- Trerotola SO, Thompson S, Chittams J, Vierregger KS (2007) Analysis of tip malposition and correction in peripherally inserted central catheters placed at bedside by a dedicated nursing team. J Vasc Interv Radiol; 18(4): 513-518.
- Aikaterini Konstantinidi, Rozeta Sokou, Polytimi Panagiotounakou, Maria Lampridou, Stavroula Parastatidou, et al. (2019) Umbilical Venous Catheters and Peripherally Inserted Central Catheters: Are They Equally Safe in VLBW Infants? Medicina (Kaunas) 55(8): 442.
- Ainsworth SB, McGuire W (2016) Peripherally inserted central catheters vs peripheral cannulas for delivering parenteral nutrition in neonates. JAMA 315(23): 2612-2613.
- Litz CN, Tropf JG, Danielson PD, Chandler NM (2017) The idle central venous catheter in the NICU: When should it be removed? J Pediatr Surg 53(7): 1414-1416.
- Kisa P, Ting J, Callejas A, Osiovich H, Butterworth SA (2015) Major thrombotic complications with lower limb PICCs in surgical neonates. J Pediatr Surg 50(5): 786-789.
- Hoang V, Sills J, Chandler M, Busalani E, Clifton-Koeppel R, et al. (2008) Percutaneously inserted central catheter for total parenteral nutrition in neonates: Complications rates related to upper versus lower extremity insertion. Pediatrics 121(5): e1152-e1159.
- Colacchio K, Deng Y, Northrup V, Bizzarro MJ (2012) Complications associated with central and non-central venous catheters in a neonatal intensive care unit. J Perinatol 32(12): 941-946.
- Ohki Y, Maruyama K, Harigaya A, Kohno M, Arakawa H (2013) Complications of peripherally inserted central venous catheter in Japanese neonatal intensive care units. Pediatr Int 55(2): 185-189.
- Cartwright DW (2004) Central venous lines in neonates: A study of 2186 catheters. Arch Dis Child Fetal Neonatal Ed 89(6): F504-F508.
- Van Winkle P, Whiffen T, Liu IL (2008) Experience using peripherally inserted central venous catheters for outpatient parenteral antibiotic therapy in children at a community hospital. Pediatr Infect Dis J 27(12): 1069-1072.
- Fletcher SJ, Bodenham AR (2000) Safe placement of central venous catheters: where should the tip of the catheter lie? Br J Anaesth 85(2): 188-191.
- Foarauer AR, Alonzo M (2000) Change in peripherally inserted central catheter tip position with abduction and adduction of the upper extremity. J Vasc Interv Radiol 11(10): 1315-1318.
- Verdino RJ, Pacifico DS, Tracy CM (1996) Supraventricular tachycardia precipitated by a peripherally inserted central catheter. J Electrocardiol 29(1): 69-72.
- Tan PL, Gibson M (2006) Central venous catheters: the role of radiology. Clin Radiol 61(1): 13-22.
-
Nisha Viji Varghese, Omar Abu Sa’ada, Uzma Afzal, Nusrat Khan. PICC Line in Neonates: Indications and Complications. A Single Level 3 NICU Experience in the UAE and Review of Literature. Glob J of Ped & Neonatol Car. 3(2): 2021. GJPNC.MS.ID.000558.
PICC line, Neonates, Central venous catheters, NICU, Infants, Preterm babies, Malposition, Catheter tip, Infection, Risk factors
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






