 Research Article
Research Article
Neonatal Risk Factors for Term Newborn Mortality at the Sylvanus Olympio University Hospital from 2013 to 2017
Tchagbele Ouro-Bagna1*, Segbedji KAR1, Ganame MKL2, Agrigna H1, Talbousouma SM1, Takassi OE3, Atakouma YD3 and Azoumah KD1
1Department of Pediatrics, University of Kara, Togo
2Faculty of Health Sciences at University of Lomé, Togo
3Department of Pediatrics, University of Lomé, Togo
Tchagbele O-B, Faculty of Health Sciences, Department of Pediatrics, University of Kara, Togo.
Received Date: September 13, 2020; Published Date: September 24, 2020
Abstract
Introduction: The reduction of neonatal mortality requires the identification of its risk factors. The objective of this study was to assess the causes of death in term newborns at the Sylvanus Olympio University Hospital Center (CHU SO).
Material and method: This was a retrospective descriptive and analytical study of term newborns who died in hospital. The main parameters studied were clinical and therapeutic data and causes of death.
Results: The hospital frequency of mortality of term newborns was 10.3%, of which 84.4% in the early neonatal period. Neonatal factors associated with early neonatal death were perinatal asphyxia, neonatal infection and congenital malformations, resuscitation in the delivery room. Inborn transfer and triple antibiotic therapy in the newborn were protective factors.
Conclusion:b> Neonatal mortality remains a major public health problem in Togo. Huge efforts remain to be made in the surveillance and followup of the mother, fetus and newborn.
Keywords: Neonatal death; Term newborn; Neonatal risk factors; Togo
Introduction
Neonatal deaths remain a major public health problem in countries with limited resources [1]. These countries are characterized by the absence of care structures adapted to newborns or by an inadequate neonatal transfer system from one center to another, explaining a high rate of neonatal hospital mortality [2]. In Togo, the infant and child mortality rate was 89‰ and that of neonatal mortality 27‰ according to the Demographic Health Survey in Togo, 3rd Edition (EDST III) of 2013 [3].
The achievement of Sustainable Development Goals (SDGs) in infant and child health requires a significant reduction of neonatal mortality in countries with limited resources [1]. Thus, several government actions whose objectives were to improve the survival of the newborn were undertaken. These included free cesarean sections, nationwide training for care providers in charge of newborns in maternity hospitals and peripheral care units on essential newborn’s care and on neonatal resuscitation based on the HBB (Helping Babies Breathe) approach [4].
It is three decades since the work on the mortality of term newborns was carried out in Togo. However, several studies have often focused on premature and low birth weight newborns in the country [5,6]. Even if overall, the causes of death of term newborns are well known in Togo, each hospital center, depending on its level in the pyramid of care and the realities of the population served, has specificities that must be identified. Thus, the absence of specific hospital studies in each care unit does not allow us to pinpoint the different causes of death of term newborns and therefore to identify the appropriate actions to be taken to reduce neonatal mortality. It therefore seemed appropriate to us to carry out this work on the mortality of term newborns at the Sylvanus Olympio Teaching Hospital (CHU SO) in Lomé, in order to determine the different neonatal factors related to this neonatal mortality.
Material and Method
Study framework
The intensive care unit for term newborns in the pediatric department of the Sylvanus Olympio Teaching Hospital served as a study ward.
Type and period of study
This was a descriptive and analytical retrospective study covering a period of 05 years from January 1st, 2013 to December 31st, 2017.
Study material
Were included in our study, all records of term newborns aged between 0 and 28 days who died in the ward during the study period. Our study did not include records of newborns who died at admission to the ward, premature, and low birth weight newborns. Were excluded, non-or incorrectly completed records of deceased infants where information on the course of the pregnancy and perinatal history was missing.
The data collection tools consisted of the department’s hospitalization register and records of hospitalized newborns who died during the study period.
The studied parameters were age, sex, perinatal manifestations, clinical data, treatment received at birth and in hospital, and causes of death. Data processing was carried out with Excel 2016 and Epi Info software version 7.2.3.0. The values of p≤0.05 were considered significant. The 95% confidence interval (CI95) was significant when it did not contain the value 1. When the odds ratio (OR) is greater than 1, CI95 is significant and p≤0.05 we are in the presence of ‘a risk factor. When the odds ratio is less than 1, IC95 is significant and p≤0.05 we are faced with a protection factor.
Results
Epidemiological data
From January 1st, 2013 to December 31st, 2017, 7,241 newborns were hospitalized in the pediatric neonatology unit of the CHU SO. Of these 7,241 newborns, 746 had died, of which 692 were included in this study according to our criteria and 6,549 were released alive. The average in-hospital neonatal mortality rate was 10.3%. The deceased newborns in our sample (N=692) were male in 426 cases (61.6%) and female in 263 cases (38.4%), for a sex ratio of 1.6. Three cases of sexual ambiguity were found (0.4%).
The mean age at admission was 2.26 days with extremes of 0 and 28 days. Three hundred and eighty-one (381) newborns out of the 692 (55.1%) had been admitted to pediatric hospitalization on the first day of life, 244 between the second and the seventh day, and 67 between the eighth and the twenty-eighth day.
As for the age at death, 217(31.4%) newborns had died within the first 24 hours of life. Death in the first week of life amounted to 584 cases, an early neonatal mortality of 84.4%; and 15.6% for late neonatal mortality.
Factors of neonatal death linked to newborns
Newborns who died were from a single pregnancy in 98.8% and multiple pregnancy in 1.2% of cases. The mean gestational age of these newborns was 38 weeks of amenorrhea (WA) + 6 days (range 37 WA and 41 WA + 5 days).
The mean duration of hospitalization for deceased newborns was 2 days ± 2.9 with extremes of 0 and 25 days.
The main causes of death were neonatal infection (74.4%), perinatal asphyxia (51.4%), birth defects (10.7%), and hemorrhagic disease of the newborn (2.9%).
Table 1:Apportionment of deceased newborns according to neonatal death factors.
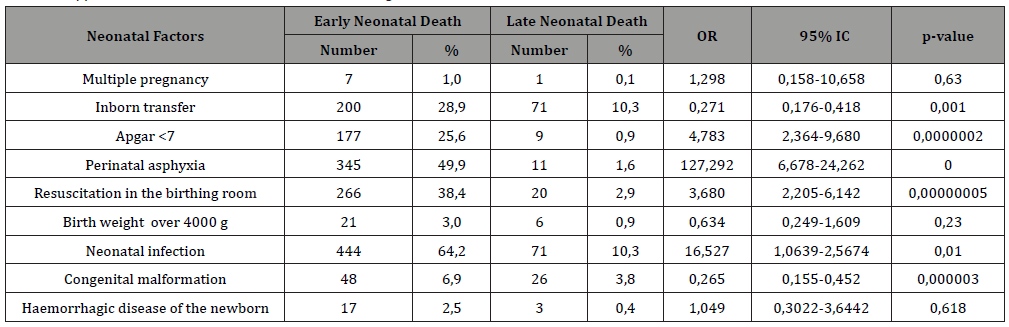
We describe the deaths according to the different neonatal factors of early mortality in Table 1.
Neonatal factors significantly associated with early neonatal death were an Apgar score of less than 7 at the fifth minute (p=0.0000002), perinatal asphyxia (p=0), neonatal infection (p=0.01), a congenital malformation (p=0.000003), resuscitation in the delivery room (p=0.00000005).
Inborn transfer was a protective factor against early neonatal mortality (p=0.001), as was triple antibiotic therapy (p=0.01).
Pregnancy type (single or multiple), excess birth weight greater than 4000 g, and neonatal hemorrhagic disease were not significantly associated with neonatal mortality. Neither were the absence of treatment or therapies such as the use of anticonvulsants, corticosteroids, mono or biotherapy antibiotics which did not influence early neonatal death.
Discussion
Neonatal risk factors
An Apgar score of less than 7 at the fifth minute was associated with early neonatal mortality. Our results are similar to those found in Cameroon [7]. The Apgar score measures the well-being of the newborn. An Apgar score of less than 7 is associated with perinatal asphyxia, the management of which is complex in our work context where neonatal care units are poorly equipped or sometimes even non-existent with providers who do not often master resuscitation procedures [8,9].
Internal transfer (inborn) was a protective factor against early neonatal mortality. It is the same in the work of Chiabi et al. [7]. Assisted deliveries should be encouraged and referral delays avoided.
Treatment received at hospital
The transition from fetal to ectopic life involves dramatic changes in the cardiovascular and respiratory systems of newborns. Most of them adjust without help; but in 3% of cases resuscitation does not turn out necessary [10]. In our study, newborns who received resuscitation in the delivery room or in the hospital room had a significant risk of dying during the first week of life. This finding differs from that of Manley et al. who argue that effective resuscitation has the potential to improve disability-free survival of newborns [10]. This observation was made from studies in high income countries; hence the difficulty of extrapolating to modest clinical settings in low- and middle-income countries.
The combination of three antibiotic molecules, namely two beta-lactams and an aminoglycoside, was a protective factor in early neonatal death in term newborns. Tripathi et al. also found that clinicians used combinations of empiric antibiotics at the first sign of neonatal infection [11]. However, this approach has its limitations, as the clinical response may be different in newborns due to maturation differences in immunity or the innate toxicity of antibiotics [12].
Duration of hospitalization
The mean duration of hospitalization for deceased newborns was 2 days ± 2.9 with extremes of 0 and 25 days. This short hospital stay reflects the seriousness of the situations in which these newborns arrive in the unit. Parental control of danger signs and consultation as soon as the first signs of disease appear in newborns would improve the vital prognosis of these newborns. These figures are similar to those obtained by Susana de Paula et al. in Brazil [13]. What differs from the results of Simiyu et al. in Kenya [14] and Kambarami et al. in Zimbabwe [15] who found an average hospital stay of 4 and 8 days for dead newborns.
Age at death time
Most neonatal deaths occurred during the early neonatal period, i.e. 84.4%, compared to 15.6% in the late neonatal period. Of these early neonatal deaths, almost one-third occurred within the first 24 hours of life. These results are similar to those of Azoumah et al. au in Kara in Togo, who found an early neonatal mortality of 95.6%, of which 58.7% before the first 24 hours of hospitalization [16]. For Chiabi et al., Mortality during the early neonatal period represented 93.4% of which 18.1% during the first 24 hours [7]. However, in these two studies mentioned above, the figures found were not reported only to term newborns. The high mortality recorded during the early neonatal period and especially during the first 24 hours is explained by poor monitoring of pregnancies and complications during childbirth. In fact, 39.4% of mothers had not followed ANC correctly, 39.2% and 12.6% had respectively had a PPR and fever during labor. These different maternal factors determine the immediate prognosis of newborns and could explain the high early neonatal mortality recorded in the various studies [7,16].
Inpatient pathologies and causes of neonatal deaths
The three main pathologies leading to death were neonatal infection, perinatal asphyxia and severe congenital malformations. These results are in agreement with global studies on neonatal mortality where it emerges that the two main pathologies responsible are respectively neonatal infection (30%) and perinatal asphyxia (30%) [17-19]. Compliance with prenatal consultation, correct management of parturient and identification of newborns with risk will significantly reduce neonatal mortality.
The management of newborns with a malformation is complex. The presence of a malformation should lead to a search for other associated malformations, in particular of the heart, the ignorance of which can sometimes be fatal for newborns. The antenatal diagnosis of these malformations would facilitate their management. Unfortunately, at CHU SO, the lack of mobile radiography and portable ultrasound in the hospital room, which is correlated with hemodynamic and respiratory instability in newborns, often makes it impossible to find cardiac malformations; some being subclinical.
Conclusion
Neonatal mortality is a silent drama and represents a major public health problem with modifiable risk factors found. Even if progress has been made over the past decade, the level of this mortality remains very high and reflects the still insufficient quality of obstetric and neonatal care in Togo.
Acknowledgement
None.
Conflict of Interest
The authors report no conflicts of interest in this work.
References
- Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, et al. (2010) Global, regional and national causes of child mortality in 2008 : a systematic analysis. Lancet 375(9730): 1969-1987.
- Faye PM, Dieng YJ, Diagne-Guèye NR, Guèye M, BA A, et al. (2016) Problem of Neonatal Transfers in the Region of Dakar. Rev Med Perinat 8(2): 94-102.
- (2014) Togolese Republic. Preliminary report of the 2013 Togo Demographic and Health Survey. Lomé: Ministry of Planning, Development and Land Use Planning, pp. 32.
- Tchagbele OB, Azoumah KD, Segbedji KAR, Kpegouni MT, Djadou KE, et al. (2015) Evaluation of the Care Providers’ Skills during the Neonatal Resuscitation in the Maternity Wards of Togo. Rev Med Perinat 7: 245-253.
- Azoumah KD, Segbedji KAR, Douti KN, Ahouankpo KA, Tchagbele OB, et al. (2017) Low birth weight newborn: epidemiological, therapeutic and evolutive aspects in the commune of Kara (TOGO) from 2014 to 2015. Int J Pediatr Res 4(12): 746-753.
- Djadou KE, Takassi OE, Guedehoussou T, Fiawoo KM, Guedenon KJ, et al. (2018) Factors associated to low birth-weight in Togo population. Rev Med Perinat 10: 169-174.
- Chiabi A, Takou V, Mah E, Nguefack S, Siyou H, et al. (2014) Risk Factors for Neonatal Mortality at the Yaounde Gynaeco-Obstetric and Pediatric Hospital, Cameroon. Iran J Pediatr 24(4): 393-400.
- Azoumah KD, Agbeko F, Douti KN, Segbedji KAR, Tchagbele OB, et al. (2017) Assessment of knowledge of maternity care providers in specific care of newborns with perinatal diseases in Togo in 2015. Rev Med Perinat 9: 247-252.
- Azoumah KD, Améwuame ANE, Agbodjan-Djossou O, Aboubakari AS, Agbèrè AD (2009) Human and material resources assessment for the neonatal intensive care at birth in Togo public hospitals of reference. J Ped Puer 22(7-8): 346-353.
- Manley BJ, Owen LS, Hooper SB, Jacobs SE, Cheong JLY, et al. (2017) Towards evidence-based resuscitation of the newborn infant. Lancet 389(10079): 1639‑16
- Tripathi N, Cotten CM, Smith PB (2012) Antibiotic use and misuse in the neonatal intensive care unit. Clin Perinatol 39(1): 61‑6
- Allegaert K, van den Anker J (2019) Neonates are not just little children and need more finesse in dosing of antibiotics. Acta Clin Belg 74(3): 157‑1
- Susana de Paula R, Luiz FCN (2010) Risk factors for neonatal death in neonatal intensive care unit according to survival analysis. Rev Bras Ter Intensiva 22(1): 19-26.
- Simiyu DE (2003) Morbidity and mortality of neonates admitted in general paediatric ward at Kenyatta national hospital. East Afr Med J 80(12): 611-616.
- Kambarami RA, Matibe P, Pirie D (1999) Risk factors for neonatal mortality: Harare Central Hospital Neonatal Unit-Zimbabwe. Cent Afr J Med 45(7): 169-173.
- Azoumah KD, Balaka B, Aboubakari AS, Matey K, Agbèrè AD (2010) Morbidity and neonatal mortality at CHU Kara (Togo). Med Afr Noire 57: 109-12.
- World Health Organization (2015) Causes of neonatal death, Geneva 2015.
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, et al. (2013) Maternal and child undernutrition and overweight in low-income and middle-income countries. Maternal and Child Nutrition Study Group. Lancet 382(9890): 427-451.
- Roberfroid D, Huybregts L, Lanou H, Henry M-C, Meda N, et al. (2008) Effects of maternal multiple micronutrient supplementation on fetal growth: a double-blind randomized controlled trial in rural Burkina Faso. Am J Clin Nutr 88(5): 1330-1340.
-
Tchagbele O-B, Segbedji KAR. Neonatal Risk Factors for Term Newborn Mortality at the Sylvanus Olympio University Hospital from 2013 to 2017. Glob J of Ped & Neonatol Car. 2(4): 2020. GJPNC.MS.ID.000546.
Neonatal death, Term newborn, Neonatal risk factors, Togo, Neonatal mortality, Newborns, Neonatal infection, Antibiotics, Birth weight
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






