 Research Article
Research Article
LISA-CODE; A Novel Method to Confirm Tracheal Catheter Placement in Less Invasive Surfactant Administration (LISA)
Mustafa Al Abdullatif* and Aiman Rahmani
Department of Pediatrics, Tawam Hospital, United Arab Emirates
Mustafa Al Abdullatif, Consultant physician Neonatology division, Department of Pediatrics, Tawam Hospital, Al Ain, United Arab Emirates.
Received Date: December 14, 2022; Published Date: January 02, 2023
Abstract
Respiratory distress syndrome is common in premature infants, and exogenous surfactant administration has been shown to be an effective treatment.
In 1992, The less invasive surfactant administration (LISA) method was first described as placing a small catheter in the trachea with Magill forceps under direct laryngoscopy, during spontaneous breathing with continuous Pressure Airway pressure (CPAP) support [1].
A recent Cochrane systematic review [2] reported a decrease in death and bronchopulmonary dysplasia and a reduction of the need for mechanical ventilation within 72 and severe intracranial hemorrhage when LISA is used.
The main challenge in applying LISA is the absence of reliable methods of confirming the placement of the thin catheter into the airway [3].
We are presenting the LISA-CODE method which is a novel method to confirm the placement of the LISA catheter into the airway using a CO2 detector attached to a connector from a size 3.0 mm endotracheal tube attached to the distal part of LISA catheter. In All our LISA-CODE cases, the CO2 detector color changed yellow demonstrating the presence of CO2. In only one case there was suspicion that the catheter wasn’t in the airway and didn’t show the change in the CO2 detector initially then the color changed after reinsertion of the catheter with the use of the same CO2 detector.
Introduction
Respiratory distress syndrome (RDS) is common in premature infants. Exogenous surfactant administration has been shown to be an effective treatment for RDS since the 1980s. There are different reported methods of surfactant administration that progressed over the last decades from administration via an endotracheal tube, to a less invasive method via a fine catheter under visualization with a laryngoscope blade (LISA) to a non-invasive method via nebulization.
In 1992, Verder et al. [1] first described the LISA method of placing a small catheter in the trachea with a Magill forceps under direct laryngoscopy, while the infant spontaneously breathes with the assistance of CPAP support.
A recent Cochrane systematic review [2] included 16 RCTs comparing LISA versus ETT surfactant administration has demonstrated the benefits of LISA method in decreasing mortality and severe intraventricular hemorrhage (IVH) (NNTB 22). In addition to reducing the need for mechanical ventilation within 72 hours (NNTB 8).
The main challenge in applying LISA is the lack of a reliable method of confirming the placement of the thin catheter into the airway [3].
We are presenting the LISA-CODE method which is a novel method to confirm the placement of the less invasive surfactant catheter into the airway.
Methods
LISA is not only a single technical procedure but rather a component of a complex care bundle. We aim to introduce using LISA at Tawam hospital (which is a tertiary teaching hospital in the United Arab Emirates and has a capacity of 51 level III NICU beds.) A multidisciplinary team including attending neonatologists, neonatal-perinatal medicine fellows, respiratory therapists, and nurses was formed. The protocol was formulated, and we started applying LISA at our hospital in February 2022 (Figure 1).
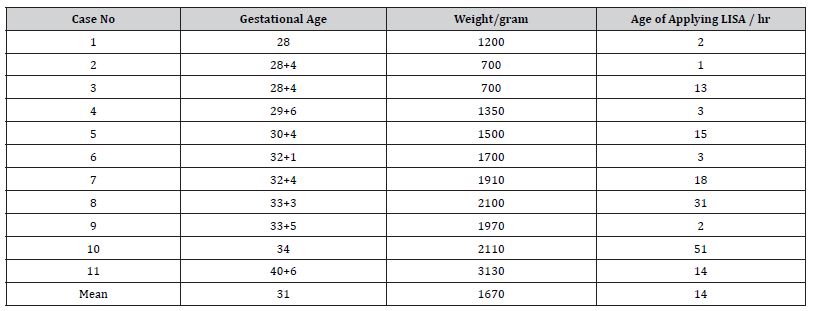
11 cases received surfactant through LISA in 2022. Table 1 shows the demographic characteristics. The mean gestational age of LISA recipient neonates was 31 weeks, and the median birth weight was 1,670 grams.
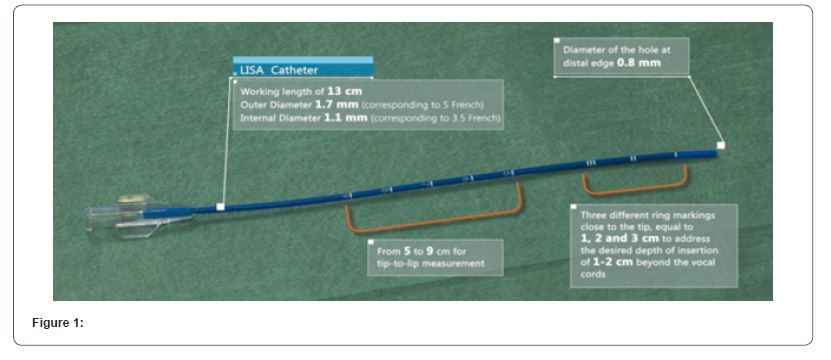
Table 1:
We use LISA Cath, (Chiesi Farmaceutici S.p.A, Parma, Italy) Figure 1 shows the specifications of the catheter.
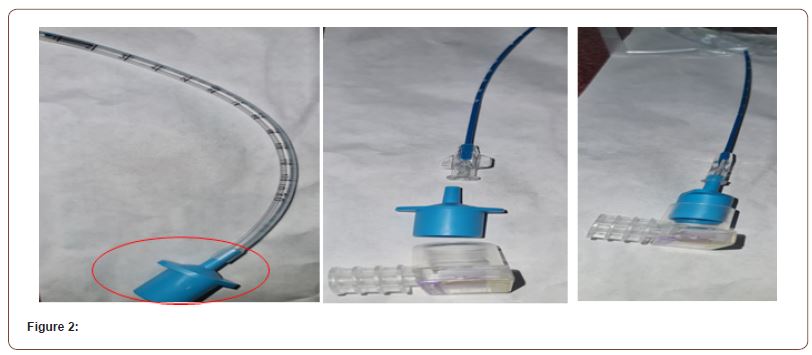
To confirm the position of the LISA catheter in the airway. We obtained a connector from a size 3.0mm Endotracheal (SUMI Tracheal Tube without Cuff ETT reference number 04-3014). We used this connector as an adaptor to attach the distal part for the LISA catheter with CO2 Detector (Westmed #562135 Pedi CO2 Easy Carbon Dioxide Detector) Figure 2.
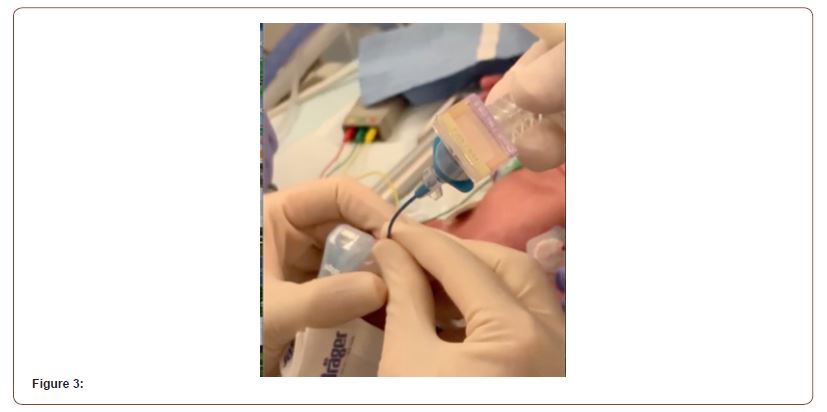
In all LISA-CODE cases, the CO2 detector color changed to yellow demonstrating the presence of CO2. In only one case there was suspicion that the catheter wasn’t in the airway and didn’t show the change in the CO2 detector initially then the color changed after reinsertion of the catheter with the use of the same CO2 detector Figure 3.
Conclusion
Using LISA-CODE can provide a reliable method to confirm the placement of a less invasive surfactant catheter into the airway.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Verder H, Agertoft L, Albertsen P, Christensen NC, Curstedt T, et al. (1992) Surfactant treatment of newborn infants with respiratory distress syndrome primarily treated with nasal continuous positive air pressure. A pilot study. Ugeskr Laeger 154(31): 2136-2139.
- Abdel-Latif ME, Davis PG, Wheeler KI, De Paoli AG, Dargaville PA (2021) Surfactant therapy via a thin catheter in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database Syst Rev 5(5): CD011672 .
- Kakkilaya V, Gautham KS (2022) Should less invasive surfactant administration (LISA) become routine practice in US neonatal units?. Pediatr Res pp. 1-11.
-
Mustafa Al Abdullatif* and Aiman Rahmani. LISA-CODE; A Novel Method to Confirm Tracheal Catheter Placement in Less Invasive Surfactant Administration (LISA). Glob J of Ped & Neonatol Car. 4(2): 2023. GJPNC.MS.ID.000581.
Catheter, Premature infants, Less invasive surfactant administration, CO2 detector, Exogenous surfactant, Direct laryngoscopy, Tawam hospital, Neonates, Orogastric tube, Tracheal Tube, Airway
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






