 Opinion
Opinion
Investigating A Child with Failure to Thrive, How Vigilante We Should Be?
Amar Al-Shibli and Abdulla Al Amri*
Consultant Pediatrician, Tawam Hospital, UAE
Abdulla Al Amri, Consultant Pediatrician, Tawam Hospital, UAE.
Received Date: August 23, 2019; Published Date: August 30, 2019
Opinion
Failure to thrive (FTT) or growth failure has long been a major focus of attention and critical thought for pediatricians. Over many years, consensus has evolved about its cause, outcome, diagnosis, and management.
The Definition of FTT in children younger than 2 years of age include: a child whose weight is below the 3rd or 5th percentile for age on more than one consecutive occasion, a child whose weight drops down two major percentile lines, a child whose weight is less than 80% of the ideal weight for age, and a child who is below the 3rd or 5th percentile on the weight-for-length curve.
It is really important to address the child with the FTT appropriately from the diagnosis to the treatment as it was shown that children with FTT are prone to more problems like growth failure, cognition and educational problem in addition to the micronutrient deficiencies and its complications.
It can be classified as nonorganic FTT (NOFTT) in majority of children and organic FTT (OFTT) in minority.
“Nonorganic” FTT (NOFTT) and its synonym, “psychosocial” FTT, were often used to imply that the child was intrinsically normal and healthy and that the observed growth failure was due to environmental issues, most commonly family factors such as neglect, indifference, or other failures of parenting. Organic FTT mostly secondary to underlying disease.
The pediatrician role is to determine, an ordered and logical workup to try to determine the cause of inadequate nutrition and, when possible, to treat the underlying pathophysiologic issues, which often are multifactorial.
It is essential to determine if FTT truly is present by using the appropriate growth centile charts and make sure that the child growth parameters are going within the same centile overtime. Some children may require special charts or considerations when using the standard charts like those with chromosomal abnormalities or those with special consideration include children who are chronically immobilized, such as those who have severe neuromotor disabilities.
Once FTT is diagnosed, a diagnostic test should be performed based on the following diagnostic classification:
Inadequate Nutritional Intake: This should be addressed from the history regarding
• Not enough food offered
• Food insecurity
• Poor knowledge of child’s needs
- Poor transition to table food
- Avoidance of high-calorie foods
• Formula dilution
• Excessive juice intake
• Breastfeeding difficulties
• Neglect
• Child not taking enough food
• Oromotor dysfuncti
• Developmental delay
• Behavioral feeding problem
• Altered oromotor sensitivity
• Pain and conditioned aversion
• Emesis
• Gastroesophageal reflux
• Malrotation with intermittent volvulus
• Increased intracranial pressure
• Malabsorption
• Cystic fibrosis
• Celiac disease
• Food protein insensitivity or intolerance
Increased Metabolic Demand
• Insulin resistance (e.g. intrauterine growth restriction)
• Congenital infections (e.g. human immunodeficiency virus, TORCH)
• Syndromes (e.g. Russell-Silver, Turner, Down)
• Chronic disease (e.g. cardiac, renal, endocrine)
During the approach for a child with FTT a
Red Flag Signs and Symptoms Suggesting Medical Causes of Failure to Thrive
• Cardiac findings suggesting congenital heart disease or heart failure (e.g., murmur, edema, jugular venous distention)
• Developmental delay
• Dysmorphic features
• Failure to gain weight despite adequate caloric intake
• Organomegaly or lymphadenopathy
• Recurrent or severe respiratory, mucocutaneous, or urinary infection
• Recurrent vomiting, diarrhea, or dehydration
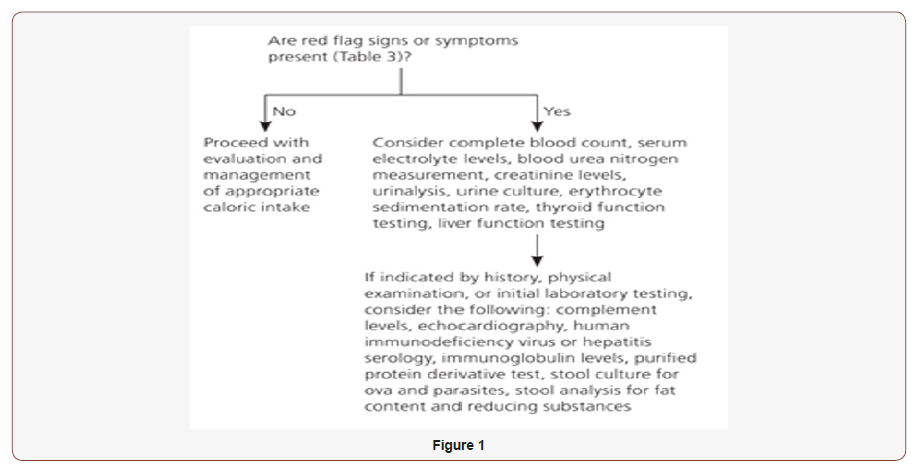
Evaluation of Failure to Thrive
(Figure 1)
Treatment: some general consideration for a child with FTT
• If a diagnosis of FTT is made and no medical conditions are suggested on examination, appropriate guidance for catch-up growth should be made. Age-appropriate nutritional counseling should be provided to parents.
• For parents of breastfed infants, recommending breastfeeding more often, ensuring lactation support, or discussing formula supplementation until catch-up growth is achieved may be helpful.
• Parents of formula-fed infants may be instructed on how to make energy-dense formula by concentrating the ratio of formula to water during periods of catch-up growth.
• Toddlers should avoid excessive juice or milk consumption because this can interfere with proper nutrition. Nutritional supplements may be given until catch-up growth is achieved. During a period of catchup growth, parents may also be instructed to provide calorie-dense foods by adding rice cereal to foods for toddlers, or adding gravies, cream sauces, or butter to foods for older children or adolescents.
• Close follow-up should be performed in the physician’s office, including evaluation of height (or length) and weight. Multidisciplinary interventions, including home nursing visits, should be considered to improve weight gain, parent-child relationships, and cognitive development.
• If a disease or medical condition is identified on history, physical examination, or additional testing, the correct approach will vary depending on the condition. Appropriate management may include specific treatment of the condition or seeking consultation from a subspecialist or other health care professional for further evaluation and management recommendations.
• In rare cases, hospitalization for observed feeding and further investigation may be helpful.
Admitting child with FTT may be warranted in the following conditions:
• The child does not improve with outpatient management
• Suspicion of abuse or neglect exists
• Signs of traumatic injury are present
• Severe psychosocial impairment of the caregiver is evident
• There are signs of serious malnutrition (e.g., child is less than 70% of the predicted weight for length).
• In summary, we proposed a simplified approach for workup a child with FTT to early diagnose and prevent its sequel.
Acknowledgement
None.
Conflict of Interest
None.
-
Amar Al-Shibli and Abdulla Al Amri. Investigating A Child with Failure to Thrive, How Vigilante We Should Be?. Glob J of Ped & Neonatol Car. 1(4): 2019. GJPNC.MS.ID.000517.
Family, Mirror Therapy, Physical therapy specialty, Infantile hemiplegia, House calls, Upper extremity
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






