 Research Article
Research Article
Diagnosis and Management of Androgen Insensitivity Syndrome in Children
Ilhama Jafarli*, Brejeetta John, Mohamed Fahmy, Mobin Syed, Pankaj Mishra, Irada Huseynova
Paediatric Surgery Department, Guy’s and St Thomas’ Hospital, Evelina Children’s Hospital, UK,
Ilhama Jafarli, Paediatric Surgery Department, Guy’s and St Thomas’ Hospital, Evelina Children’s Hospital London, UK.
Received Date: March 18, 2023; Published Date: March 31, 2023
Abstract
Introduction: Androgen Insensitivity Syndrome (AIS) is a rare X-linked disorder characterised by an impaired virilisation in an individual with 46, XY karyotype. It is caused by several mutations in the Androgen receptor gene. There are 3 main phenotypes seen in AIS: Complete, partial and mild AIS. AIS can be difficult due to late diagnosis in puberty as well as due to the lack of clear guidelines present. This systematic review looks at the diagnosis and management of AIS in children.
Methods: A systematic search was conducted looking into the process of diagnosis of AIS and the surgical and non-surgical interventions available to treat AIS. The studies were collated mentioning the year, type of study and the number of patients involved. The review also includes studies that looked at adults >18yrs due to limited literature on children.
Results: A total of 28 articles were identified that fit the inclusion criteria.
Conclusion: The main aim of the management of AIS should address the full disclosure of diagnosis, functional, sexual and psychological issues associated with it. The diagnosis of AIS may be made before or after puberty using karyotyping, ultrasounds and MRI scans. The main surgical intervention includes a gonadectomy followed by oestrogen replacement therapy especially for Complete AIS and PAIS after puberty. Mammoplasty for the reduction of gynecomastia can be offered to those with PAIS/ MAIS that identify as male. It is also important to involve the MDT and the family whilst making decisions about gender assignment.
Keywords: Androgen insensitivity syndrome; Manage
Introduction
Androgen Insensitivity Syndrome (AIS) is a rare X-linked disorder characterised by an impaired virilisation in an individual with 46, XY karyotype and testes producing age-appropriate normal/low concentrations of androgens (Lancet, 2012). This is caused due to multiple mutations in regions of the AR gene (Xq12) coding for the androgen receptor. 70% of these mutations are because of maternally inherited mutations whereas the other 30% are de novo mutations [1]. The receptor is responsible for mediating the differentiation and development of a normal male phenotype [2]. The clinical phenotype of AIS is variable and can be classified into 3 main broad groups: Complete Androgen Insensitivity (CAIS), Partial Androgen Insensitivity (PAIS) and Mild Androgen Insensitivity (MAIS). The site of the mutation in the AR gene will influence the phenotype of the individual with AIS. It has been found that large mutations in the N-terminal domain (NTD) will mainly lead to CAIS however, mutations in the Ligand Binding Domain (LBD) of the gene will mainly cause either CAIS or PAIS [1].
‘Those with Androgen Insensitivity Syndrome has a wide spectrum of clinical presentation such as having gynecomastia or reduced fertility due to impaired spermatogenesis to primary amenorrhoea.’ Complete AIS shows complete feminisation of the external genitalia; PAIS can have variable clinical presentations (female, ambiguous or male genitalia) and mild AIS is characterised by male external genitalia and impaired pubertal virilisation [1]. Impaired virilisation describes when an individual with a karyotype 46, XY fails to develop male characteristics which can include hirsutism, deepening of the voice and increased muscularity. Whilst some patients present before puberty having identified bilateral inguinal masses (later identified as testes), others can present after puberty due to primary amenorrhoea or sparse to little public and axillary hair in AIS [3]. The development of oestrogendependent secondary sexual characteristics occurs as a result of excess aromatisation of the androgens (Lancet, 2012). These presentations along with feminisation of the external genitalia in a karyotype 46, XY should prompt investigations to diagnose androgen insensitivity syndrome however, the diagnosis of AIS can happen by chance due to the mismatch between prenatal sex prediction and the phenotype at birth. Some of the investigations include DNA sequencing, karyotyping, laboratory investigations and ultrasonography/ MRI scans to identify the undescended testes.
The management of androgen insensitivity syndrome will depend on the type of AIS however, the main aims of the interventions should address the functional, sexual and psychological issues such as gonadectomy accompanied hormone replacement therapy, creation of a functional vagina and providing genetic advice [4]. It is important to have a holistic approach and involve the MDT as the diagnosis can be psychologically distressing and important decisions need to be made about the timing of surgical interventions if needed.
There have been many case reports of those diagnosed with androgen insensitivity syndrome as well as other systematic reviews exploring the management options for AIS in adults. Currently, there might be a higher chance of this diagnosis in infants due to DNA karyotyping and prenatal scans so, it is important to consider age-appropriate disclosure as well as consider the risks and benefits of certain invasive treatment options for the child. Therefore, the main aim of this systematic review is to look at the diagnosis and management of androgen insensitivity syndrome in children.
Methodology
The clinical questions that were explored in this systematic review include: 1) State the process of diagnosis of Androgen Insensitivity in children. 2) What are the surgical and nonsurgical interventions for Androgen Insensitivity in children? The systematic review related literature published in the last 15 years using Medline, Embase, PubMed and Cochrane Library. The English translations for the foreign studies were also included in this review.
The criteria for possible inclusion are as follows:
1) Patients age group 0-18yrs
2) Diagnosis of Androgen Insensitivity Syndrome
3) Management of Androgen Insensitivity Syndrome
There is limited data specifically exploring the diagnosis and management of AIS in children, therefore this systematic review has included all possible studies including adults >18years. The lack of literature could be because of the sensitivity around the diagnosis of AIS. It might make it harder to also gain informed consent from children and address the potential emotional distress.
The studies were collated mentioning the year, type of study, the number of patients involved and their mean age. Any duplicates of the study were also noted and excluded during the collection. The quality of evidence of the studies included in this systematic review was not evaluated.
Results
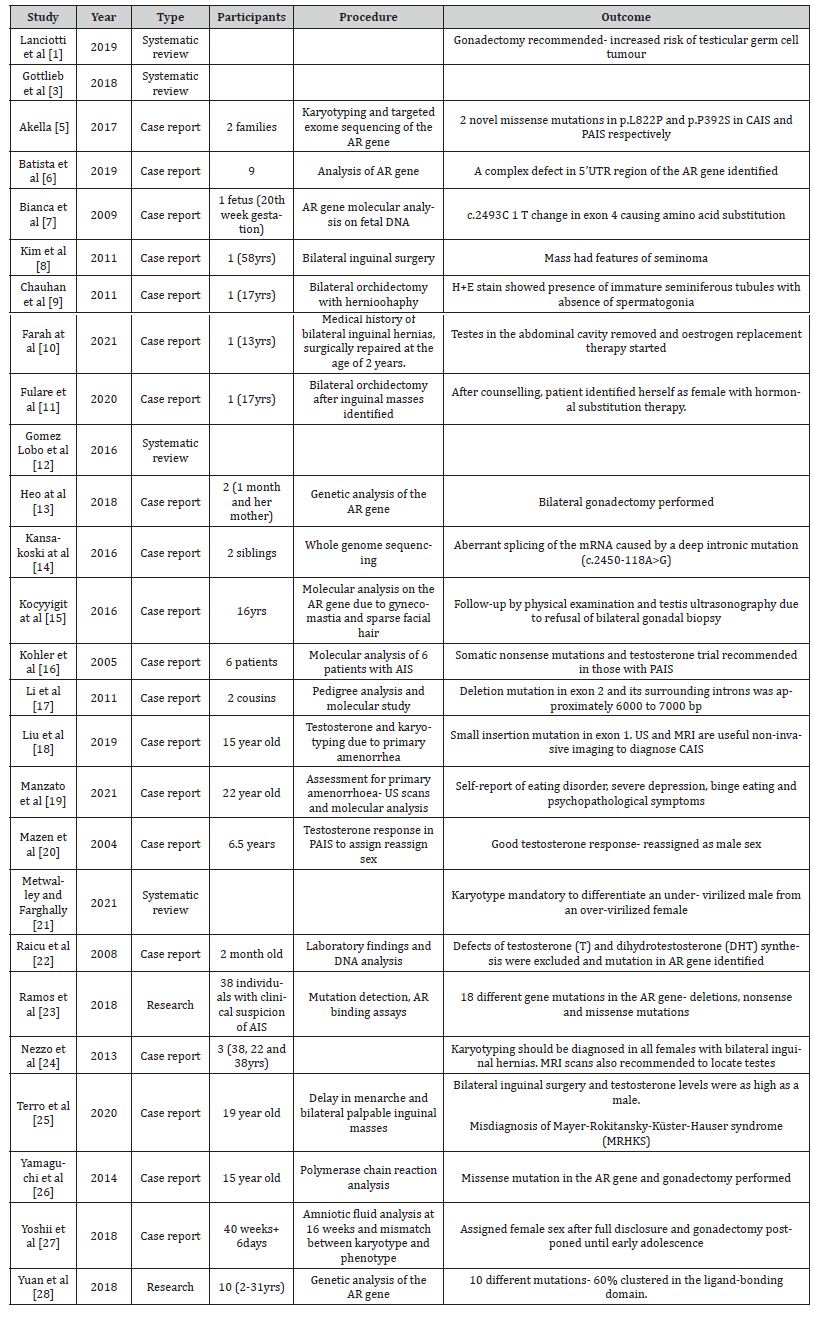
A total of 28 studies looking at the diagnosis and management of androgen insensitivity syndrome were chosen to be included in this systematic review. They all fit the inclusion criteria mentioned above. This can be seen in Table 1.
Table 1:Full list of all articles used in the systematic review.
Discussion
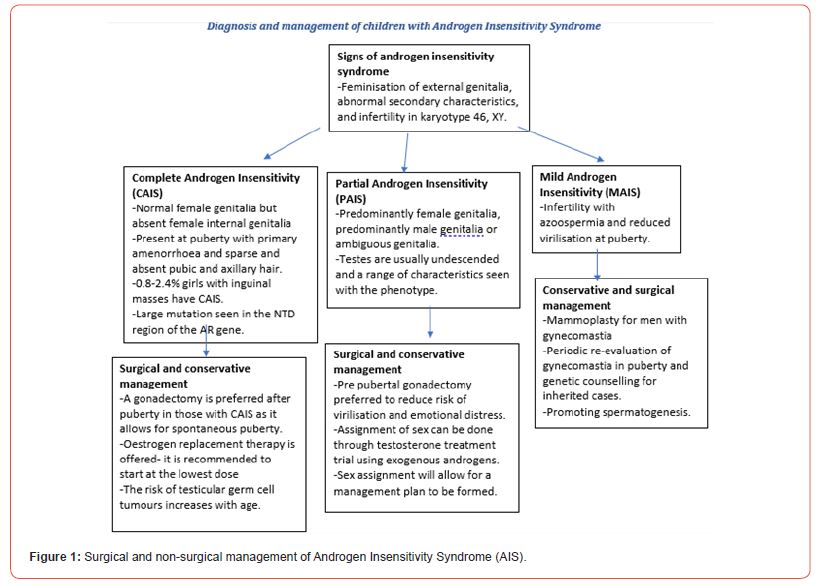
The management of Androgen Insensitivity Syndrome (AIS) will require the correct diagnosis of the type of AIS (Figure 1). The diagnosis of AIS should be established in someone that has a 46, XY karyotype with feminisation of the external genitalia, abnormal secondary characteristics and infertility [3]. A molecular DNA analysis of those with AIS would most likely show a mutation in the various regions of the AR gene that causes frameshifts, deletions and single base mutations which can reduce the transcriptional activity of the Androgen receptor [23]. Many studies suggest that mutations in different parts of the gene can determine the type of AIS; large NTD mutations mainly lead to Complete AIS [1] whereas missense mutations in the NTD/ DBD of the gene has a milder effect on the AR function therefore leading to either mild or partial CAIS.
A hCG test can also help to exclude a 5-alpha reductase 2 deficiency and a decreased testosterone biosynthesis that may present with similar clinical presentations [2]. It is also useful to draw a family tree to identify manifesting carriers with spare/ delayed axillary hair, delayed puberty or hypospadias. The use of ultrasonography is the first line to look for Mullerian structures and an MRI can assist in locating the undescended testes in the abdominal cavity [25].
Complete androgen insensitivity syndrome
Those with CAIS mainly have normal female genitalia with absent internal genitalia. Therefore, many of these individuals will present at puberty with primary amenorrhea and absent pubic and axillary hair. They can also present with bilateral inguinal hernias that are later established to be undescended testes. This should trigger a karyotype study. The measured length of vagina during hernia operations can also be short in females with CAIS. A gonadectomy is delayed allowing for spontaneous puberty to occur which is then followed by oestrogen replacement therapy [4]. However, if gonadectomy is performed before puberty, puberty will have to be induced using oestrogen replacement therapy. There is evidence of an increased risk of testicular germ cell tumor with age from the undescended gonads [1,8] however the removal of gonads is increasingly controversial. Vaginoplasty or vaginal dilator therapy may be considered to avoid dyspareunia despite this being controversial and not routinely recommended [10].
Partial androgen insensitivity syndrome
In those with PAIS, full disclosure is more beneficial with gender assignment deemed to be very crucial [4]. A prepubertal gonadectomy is preferred in those with PAIS that have predominantly female genitalia to reduce the risk of virilisation and the psychological discomfort [2]. This can be combined with oestrogen replacement therapy. However, in those with PAIS and either ambiguous or male genitalia, assignment of sex can be determined through testosterone treatment using exogenous androgens. The treatment will check for androgen responsiveness to assign sex using expert evaluation in infancy. However, more data is required to establish the effectiveness of androgen treatment at puberty in these children [16].
A reduction mammoplasty would be recommended in those with gynecomastia. Other surgical interventions involve hypospadias repair and bringing undescended testes into the scrotum [4,15].
Mild androgen insensitivity syndrome
Those with MAIS mostly have reduced virilisation at puberty such as high pitch voice, sparse hair, gynecomastia and reduced fertility due to impaired spermatogenesis [2,7]. Therefore, those with MAIS may require mammoplasty for gynecomastia and promoting spermatogenesis through testosterone therapy.
Additional management and support
A diagnosis of AIS should be carried out with full disclosure that involves the patients and the family using an MDT that addresses functional, sexual and psychological issues. It is also important to have genetic counselling to discuss the consequences of infertility and for the evaluation of any relatives at risk. Genetic counselling is important to also address the guilt of passing on the mutation in the mother [26]. It is also recommended to supplement both Calcium and Vitamin D to improve bone density in those with AIS [3,23].
Conclusion
There are a variety of both surgical and non-surgical interventions that are available to treat Androgen Insensitivity Syndrome. However, it is vital to establish a correct diagnosis of the type of AIS and address the main clinical presentations whilst forming a management plan. Gonadectomy is advised for CAIS after puberty to allow for spontaneous pubertal development however, there is a risk of prepubertal tumors. However, it can help to reduce the psychological discomfort associated with the diagnosis of AIS in individuals identifying as females. A full disclosure of the diagnosis is important along with psychological support and genetic counselling to address infertility and the risk of relatives that may be asymptomatic carriers.
A more complex management is required when patients present with partial AIS with various phenotypes, therefore, care and priority should be to provide sex assignment in infancy and establish androgen responsiveness. However, more research is needed to understand the effectiveness of an androgen responsiveness test and its reliability in guaranteeing the same response during puberty. Hormonal replacement therapy proves to be vital when managing those with AIS throughout puberty as well as to prevent secondary manifestations such as increasing bone density.
Funding
None.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Lanciotti L, Cofini M, Leonardi A, Bertozzi M, Penta L, et al. (2019) Different Clinical Presentations and Management in Complete Androgen Insensitivity Syndrome (CAIS). Int J Environ Res Public Health 16(7): 1268.
- Galani A, Kitsiou-Tzeli S, Sofokleous C, Kanavakis E, Kalpini-Mavrou A (2008) Androgen insensitivity syndrome: clinical features and molecular defects. Hormones (Athens) 7(3): 217-29.
- Gottlieb B, Trifiro MA, Nezzo M (2018) Androgen insensitivity syndrome. International journal of surgery case reports 26(3): 167-169.
- Hughes IA, Davies JD, Bunch TI, Pasterski V, Mastroyannopoulou K, et al. (2012) Androgen insensitivity syndrome. Lancet 380(9851): 1419-28.
- Akella RR (2017) Mutational Analysis of Androgen Receptor Gene in Two Families with Androgen Insensitivity. Indian J Endocrinol Metab 21(4): 520-23.
- Batista RL, Yamaguchi K, Rodrigues AdS, Nishi MY, Goodier JL, et al. (2019) Mobile DNA in Endocrinology: LINE-1 Retrotransposon Causing Partial Androgen Insensitivity Syndrome. J Clin Endocrinol Metab 104(12): 6385-90.
- Bianca S, Cataliotti A, Bartoloni G, Torrente I, Barrano B, et al. (2009) Prenatal diagnosis of androgen insensitivity syndrome. Fetal Diagn Ther 26(3): 167-69.
- Kim HO, Kim CH, Kim SA, You RM, Kang HJ, et al. (2011) A large advanced seminoma in an older woman with androgen insensitivity syndrome. Clin Exp Reprod Med 38(2): 115-18.
- Chauhan NS, Sharma YP, Sharma S, Sharma S (2011) Complete androgen insensitivity syndrome with microtia: a rare presentation. Jpn J Radiol 29(1): 67-71.
- Farah S, El Masri D, Hirbli K (2021) Complete androgen insensitivity syndrome in a 13-year-old Lebanese child, reared as female, with bilateral inguinal hernia: a case report. J Med Case Rep 15(1): 202.
- Fulare S, Deshmukh S, Gupta J (2020) Androgen Insensitivity Syndrome: A rare genetic disorder. Int J Surg Case Rep 71: 371-373.
- Gomez-Lobo V, Amies Oelschlager AM, North American Society for Pediatric and Adolescent Gynecology (2016) Disorders of Sexual Development in Adult Women. Obstet Gynecol 128(5): 1162-73.
- Heo YJ, Ko JM, Lee YA, Shin CH, Yang SW, et al. (2018) Two Korean girls with complete androgen insensitivity syndrome diagnosed in infancy. Ann Pediatr Endocrinol Metab 23(4): 220-25.
- Kansakoski J, Jaaskelainen J, Jaaskelainen T, Tommiska J, Saarinen L, et al. (2016) Complete androgen insensitivity syndrome caused by a deep intronic pseudoexon-activating mutation in the androgen receptor gene. Sci Rep 6: 32819.
- Kocyigit C, Saritas S, Catli G, Onay H, Dundar BN (2016) A Novel Mutation in Human Androgen Receptor Gene Causing Partial Androgen Insensitivity Syndrome in a Patient Presenting with Gynecomastia at Puberty. J Clin Res Pediatr Endocrinol 8(2): 232-35.
- Kohler B, Lumbroso S, Leger J, Audran F, Grau ES, et al. (2005) Androgen insensitivity syndrome: somatic mosaicism of the androgen receptor in seven families and consequences for sex assignment and genetic counseling. The Journal of clinical endocrinology and metabolism 90(1): 106-11.
- Li BK, Ding Q, Wan XD, Wang X (2011) Clinical and genetic characterization of complete androgen insensitivity syndrome in a Chinese family. Genet Mol Res 10(2): 1022-31.
- Liu S, Wang Z, Jiang J, OuYang H, Wei S, et al. (2019) Severe forms of complete androgen insensitivity syndrome caused by a p.Q65X novel mutation in androgen receptor: Clinical manifestations, imaging findings and molecular genetics. Steroids 144: 47-51.
- Manzato E, Gualandi M, Roncarati E (2021) Complete androgen insensitivity syndrome (CAIS) and eating disorders: a case report. Eat Weight Disord 26(7): 2421-26.
- Mazen I, Lumbroso S, Abdel Ghaffar S, Salah N, Sultan C (2004) Mutation of the androgen receptor (R840S) in an Egyptian patient with partial androgen insensitivity syndrome: review of the literature on the clinical expression of different R840 substitutions. J Endocrinol Invest 27(1): 57-60.
- Metwalley K, Farghaly H (2021) Hormone resistance in children: what primary care physicians need to know. Acta Biomed 92(4): e2021255-e55.
- Raicu F, Giuliani R, Gatta V, Palka C, Franchi PG, et al. (2008) Novel mutation in the ligand-binding domain of the androgen receptor gene (l790p) associated with complete androgen insensitivity syndrome. Asian J Androl 10(4): 687-91.
- Ramos L, Chavez B, Mares L, Valdes E, Vilchis F (2018) Mutational analysis of the androgen receptor (NR3C4) gene in patients with 46,XY DSD. Gene 641: 86-93.
- Nezzo M, De Visschere P, T'Sjoen G, Weyers S, Villeirs G (2013) Role of imaging in the diagnosis and management of complete androgen insensitivity syndrome in adults. Case Rep Radiol 2013: 158484-84.
- Terro JJ, El-Helou E, Jammoul K, El Lakkis R, Shibli A, et al. (2020) Bilateral inguinal masses or hernias in a female teenager with delayed menarche: Think of Complete Androgen Insensitivity Syndrome (CAIS), a case report. Int J Surg Case Rep 76: 25-29.
- Yamaguchi M, Sameshima H, Ikenoue T (2014) Genetic diagnosis and genetic counseling for androgen-insensitivity syndrome: a report of three cases. J Obstet Gynaecol Res 40(3): 723-27.
- Yoshii K, Naiki Y, Terada Y, Fukami M, Horikawa R (2018) Mismatch between fetal sexing and birth phenotype: a case of complete androgen insensitivity syndrome. Endocr J 65(2): 221-25.
- Yuan SM, Zhang YN, Du J, Li W, Tu CF, et al. (2018) Phenotypic and molecular characteristics of androgen insensitivity syndrome patients. Asian J Androl 20(5): 473-78.
-
Ilhama Jafarli*, Brejeetta John, Mohamed Fahmy, Mobin Syed, Pankaj Mishra, Irada Huseynova. Diagnosis and Management of Androgen Insensitivity Syndrome in Children. Glob J of Ped & Neonatol Car. 4(2): 2023. GJPNC.MS.ID.000584.
Androgen insensitivity syndrome, Manage, 46, XY karyotype, Children, Androgen receptor, Diagnosis, MRI scans, Gonadectomy, Ultrasonography, Testosterone, Infertility, Risk, Gynecomastia, Virilisation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






