 Research Article
Research Article
Challenges in Neonatal Intensive Care Unit Design: Barriers for Kangaroo Mother Care Implication
Sorour Roustazadeh1, Fatemesadat Mousaviasl2 and Mahboobeh Namnabati3*
1Art University of Isfahan, Iran
2Isfahan University of Medical Sciences, Isfahan, Iran
3Nursing and Midwifery Care Research Center, Isfahan University of Medical Sciences, Iran
Mahboobeh Namnabati RN, MSc, PhD, Association Professor .Department of Pediatric and Neonates. Nursing and Midwifery Care Research Center, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
Received Date: November 01, 2021; Published Date: December 06, 2021
Abstract
Background: The Neonatal intensive care unit (NICU) design models can have a negative impact on neonatal health care. Kangaroo Mother Care (KMC) has been a care method and needs privacy spaces for mothers considering religious culture, especially for the premature infants.
Objective: We conducted this study to explore barriers to the KMC implementation regarding to existing NICU design.
Material and methods: This is a qualitative study in which 28 mothers and NICU specialist nurses enrolled based on a purposive sampling. The data was collected through intensive interviews, presence of the researcher in the field, and the infants’ files in the NICUs in Isfahan-Iran.
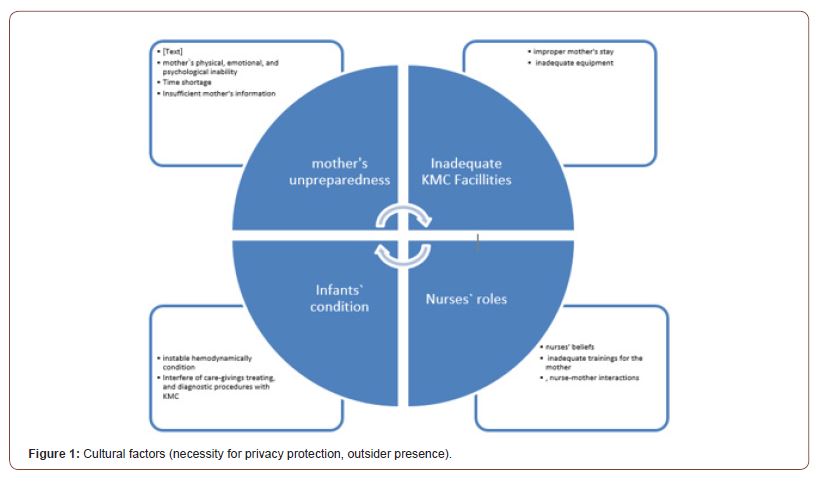
Results: The findings were analyzed through qualitative content analysis. The findings classified in four themes including: A) mother’s unpreparedness B) infant’s condition C) NICU design based on cultural-religious factor (D) nurse’s role.
Conclusion: NICU designing is an important barrier to applying KMC. Thus, it is suggested that architecture of NICU involve with privacy and sufficient space for breast feeding and skin to skin infant-mother.
Keywords: Barriers; Kangaroo mother care; Design; Infants; Health care architecture
Introduction
Nowadays, most of in NICU hospitalized infants are premature Infant low-weight side effects have decreased with the advancement of technology but not as much as mortality and morbidity. Although, the mortality has decrease but the premature infants’ care needs increase because many of them are hospitalized in NICU [1].
The process of Infant-mother separation starts with the hospitalization of premature infant that may persist days or weeks. This separation leads to release of stressing hormones that affects heart and respiration rate, and body temperature [2]. Delivery and hospitalization of a premature infant is also a crisis to the family, especially the mother who will lose self-confidence and selfsatisfaction [3].
KMC has been suggested to the mothers and health professionals’ teams as a family centered care-giving approach that improves both confidence and satisfaction in mothers. The infant has a vertical skin-to-skin contact on mother’s chest in this natural, easy, and affectional approach. World Health Organization introduced the KMC as an excellent approach for giving care to the infants, especially premature infants in 1993. Mother’s Psychological depression, stress, and guilty conscience are decreased, and she is helped toward a deeper affection for her infant by this method. Oxytocin hormone that stimulates secretion of milk and is a relaxing agent is also released in this method, enabling the mother for giving a better care [4].
Therefore, KMC, improving mother-infant, especially motherpremature infant, attachment, affection, and interaction, as well increased breastfeeding self-efficacy perception of the mothers and reduced the perceived insufficient milk supply effect on breastfeeding perceptions decreases the side effects of the separation vigorously that in turn leads the mother to more selfconfidence in giving care and to establish a stronger affection for her infant [3-5].
On the other hand, KMC will decrease infection, mortality and morbidity, expedite weight gain, prolong sleep duration and improve sleep pattern, alleviate the pain of colic, and integrate physiologic indexes and oxygenation among infants [6]. Therefore, we understand from the worldwide studies that KMC has been suggested as a conventional care method for the infants, especially premature infants.
For implementing KMC, the NICU design must be considered for both usability and emotional experience between mother and infant based on cultural issues. In the standard design, there must be a privacy room for family and be well equipped. These days, design for emotion in an interior architecture design process are significantly considered [7].
There are a limited number of studies conducted about barriers to KMC implementation worldwide. Social, cultural, and religious factors and available facilities of the countries affect the implementation of every type of care. Accordingly, barriers to KMC implementation should considered with respect to culture, facilities, and the staff available in neonate wards of Iran. Therefore, the present study was to explore the mother`s perception to KMC implementation regarding to existing NICU design, while the mothers are the main KMC performers, to improve the care effectiveness to the possible extent.
Methods
This is a qualitative study incorporating conventional content analysis approach. The researchers gathered the data through file reviews, unit observation, and interviews with participants in an NICU in Isfahan-Iran.
The participants were 20 mothers of premature infants, and 8 nurses, employed in two NICUs in Isfahan- Iran.
All participants were informed about the study and that they could terminate the study anytime they wished.
Enrollment was done through a purposive sampling, with respect to the inclusion criteria. Mothers, when completely ready, were individually interviewed in a public room. The nurses were also individually interviewed in staff break room. Unit observation continued in all working shifts of morning, evening, and night until the data was saturated. The study took eight months’ time through. The data was inductively, which is a suitable way to explore the facts and to specify the existing condition, analyzed through qualitative content analysis.
Results
Perceived barriers to the KMC classified in four themes and ten sub-themes. The themes are: Mother’s unpreparedness, Infant’s condition, NICU design based on cultural-religious factor, Nurse’s role and (Figure 1).
Mother’s unpreparedness
Mother’s physical, emotional, and psychological inability: The pain of delivery makes the mother reluctant to body movements and may multiply the depression of an unexpected preterm delivery. Therefore, as we noticed among the participants, mothers with premature infants are physically and emotionally in a poor condition. A mother of a premature infant mentioned, “On sitting on a chair, I feel pain at my sutures; and I don’t hug my baby”.
A nurse said, “The infant’s mother just cries and it is water off a duck’s back with her when we tell her that the baby would be fine”. Another mother said, “To be truth, I afraid touch this little baby. Just I fondle it while in the device”.
The researcher found the high stress and anxiety in mothers’ of premature infants obviously.
Time shortage: Both mother and infant need time, enough to perform the KMC. Due to having another child at home, some mothers cannot stay in the unit permanently. In the interviews, mothers indicated that they were too busy full time milking, feeding, and diaper changing for their twins or triplet.
Insufficient mother’s information: In order to implement the KMC, mothers need ample information about the advantages of the care to intend implementation; and it true when they indicated too little familiarization with the useful effects of the care in negotiations that has resulted in their low interest in KMC.
Infant’s condition
Instable hemodynamically condition: In NICU hospitalized infants may encounter instable oxygenation and need oxygen after some improvement due to blood infection, low blood content, etc. They cannot receive KMC in this instable hemodynamical condition, even though they received it earlier. A mother claimed, “I used to keep my baby on my chest in recent days, but I don’t know how he suddenly got oxygen drop and then was injected blood. That is why I don’t do KMC today”.
Interfere of care-giving, treating, and diagnostic procedures with KMC: There are daily repeated care, diagnostic, and treatment procedures such as lumbar puncture (LP), brain sonography and vain puncture that prevent KMC implementation. A premature infant’s mother said “I could not hold my baby on my chest today because, my baby had LP. And instructed me not to move him”.
A nurse suggested, “KMC should be done in the nighttime. There are many things to do during the day. Mothers may not keep their babies on their chest for hours”.
NICU design based on cultural-religious factor
Improper mother’s stay: KMC implementation essentially necessitates permanent stay of mother in unit to keep the infant on her chest continuously. Therefore, suitable NICU design and equipment such as having a single room, comfortable bed, etc. should be available. However, most of the mothers stated during negotiations that they go back home because mothers’ room is not designed based on their needs.
Inadequate equipment: Some equipment such as suitable chair, pulse oximeter, mother’s private life deserve, etc., are necessary to implement the KMC. Any shortage or lack of these equipment will prevent the implementation. A mother stated in this regard, “the mother who arrives in hospital earlier in the morning would take and use the black leather chair to do the KMC and those who are late should use the plastic type which is not convenient at all”.
Another mother said “I couldn’t do KMC yesterday and today because they took the pulse-oxy-meter to another infant who was in emergency; and I afraid my baby might get oxygen drop during KMC.
Taking the role of a participant, the researcher observed in the unit that the KMC interrupted during physician’s visit just because the physician could interfere mother’s private life, even though unintended.
Nurse’s role
Nurses’ beliefs: Studies indicate that the nurses play a key role in KMC implementation. Therefore, knowledge upgrade and a change in their viewpoint would be most effective on KMC implementation. Negotiation with the nurses has indicated in this study that their viewpoint and beliefs caused low interest toward KMC implementation. A nurse of the unit stated in this regard, “There is no need to KMC when the infant goes under mother’s chest because skin to skin contact is established”. Another nurse said, “Isn’t KMC the same as breast feeding?”.
Insufficient training for mother: Mothers of premature infants are less interested in KMC implementation due to insufficient information. The nurses can persuade them by giving enough trainings including correct infant positioning during the care. A mother stated in this regard, “My infant turned black (cyanotic) the first day I did KMC and I promised myself not to pick her up ever again”. The mother of an infant that was under breast-feeding stated, “I was not told to lay the infant of my chest. They just said to put it under the breast.” In addition, a nurse said, “Honestly, it is too difficult to instruct the mothers broadly about duration and time of KMC implementation when we have a few infants to care about”.
Mother-nurse interactions: Nurses’ communication and interaction with the premature infant’s mother, who suffers stress, are quite effective. The mother of a 30 weeks’ infant said, “I request my baby’s nurse to help putting her on my chest when I arrive in the unit early at the morning, but she wants me to wait until she finishes her works, therefore it takes time. Next is the physician’s visit, when I cannot do KMC at all”.
An experienced nurse of the unit said, “A mother for instance is afraid to touch her baby. She expect a nurse be with her and support her all the time. But, we, the nurses are really busy; nevertheless, it is our pleasure to help mothers”.
Discussion
Today, KMC is known as a conventional care in the NICUs. The aim of this study was to identify the most frequently perceived barriers to the implementation KMC. As an intervention to the care of premature infants, KMC improves mother’s role and developmental care. This method has been suggested in numerous studies since, it significantly decreases morbidity and mortality, expedites weight gaining, prolongs sleep duration, and integrates infant’s physiologic indexes [8]. It also increases self-confidence in mother and makes stronger affectional attachment between mother and infant [2]. Therefore, it is seen that the KMC has been suggested in all related studies as an effective care method for all, especially premature infants.
The result of study showed that the unprepared mother, infant’s condition, insufficient equipment, nurse’s role, and cultural issues were found as barriers to implementation of KMC through interviews with NICU nurses and premature infants’ mothers. The theme of unprepared mother classified to three subthemes including: mother’s psychological and physical - emotional inability, insufficient available time, and inadequate mother’s information. In a study on the extent of KMC implementation and the barriers from mothers’ viewpoints, they mentioned uncooperative family members as the most important barrier that they could not spend permanent time for their infant because they had to do the chores and take some rest as pregnancy and delivery caused them a chronic tiredness. Referring to the mothers’ insufficient information, the nurses stated in this study that the mothers are hard to be reasoned with the importance of KMC [9]. Salimi et al. [10] conducted a study, aiming to assess the experiences of in NICU hospitalized premature infants’ mothers about the implementation of KMC, and indicated that fathers’ disaffiliation in KMC implementation and mothers’ tiredness resulted in less KMC implementation [10]. Contrary to the above studies that indicated mother’s insufficient available time and information as parts of barriers to KMC implementation, Blomqvist indicated in another study, conducted to assess facilitating factors to KMC implementation from Swedish parents’ viewpoints, that the mothers able in terms of sufficient time and physical power to perform the KMC [11]. Also, Gupta explained the KMC may be implemented either by grandmothers or sisters in India [9].
Inadequate KMC equipment was another barrier that was noted in this study. Similarly, Salimi et al. mentioned the lack private room in NICU for the parents, especially the mothers, that resulted in less KMC implementation by the mothers [10]. Thus, it is suggested that the design of NICU architecture must have more privacy and comfortability through interior designing. Solomons et al. indicated in their study that, according to 66.7 nurses` viewpoints, lack of a comfortable bed and a suitable area for the mother to stay in and keep her belongings is a barrier to KMC implementation in South Africa [12]. In the study in Sweden, that according to the parents’ viewpoints the equipment and residence, needed for their permanent round the clock stay, as well as wireless and portable monitor, a facilitator to KMC implementation, was available. Physical preparations are important to KMC implementation [13].
Nurse’s role with three subtheme of nurse’s beliefs, insufficient trainings to the mothers, and nurse-mother interactions, is another barrier to the KMC implementation and, according to a study, is suitably met by only 10%of the mothers [14]. Another study has notified the nurses and physicians about the importance of their role for training the mothers [15].
Conducting a similar study in India, based on nurses’ viewpoints, the main prevention to KMC implementation is the difficulty in convincing the mothers of the importance of KMC. Believing in usefulness of the KMC, most of the nurses were positive and supportive to the care method in this study [9].
Regarding cultural religious factors in Iran, KMC must be done in a single room. The single-family room system was implemented for keeping privacy for families and provide developmental care. This family room has a significant impact on the mother`s perceptions for implementing KMC [16]. Cultu1ral factors are the most important issues in the care of infant in the Iranian NICU for parents [17,18]. Blomqvist et al indicated the supporting and training the parents by the nurses was a facilitating factor to KMC in Sweden and that their attitude was effective on parents’ desire to KMC implementation 11. The result of studies indicated the NICU nurses must be trained and helped the parents. These nurses had rendered enough information and required support to some 83.3% of the parents that had resulted in permanent and round the clock KMC implementation [17-19].
Infant’s condition was another barrier to the KMC, noted in this study. Diagnostic - treatment procedures such as LP, venipuncture that may prevent to perform the KMC. It is similarly stated in the results of a study that vein or vessel damages is considered a barrier to KMC in the United States [15].
Implications for Practice
Identified barriers to the KMC can help to policy makers to solve the problems. Proper interior designing of the NICU leads to remove some barriers and improve privacy for skin to skin contact and implementing KMC. Providing continue education for nurses improve their practice in the NICU.
Acknowledgment
We would like to thank vice-chancellery for research of Isfahan University of Medical Sciences. Researchers greatly appreciate friendly cooperation of the nurses and mothers in Al-Zahra and Shahid Beheshti hospitals. This study was approved by the Ethics Committee of Isfahan University of Medical Sciences. The number of projects is 393308.
Conflicts of Interest
The authors declare that there is no conflict of interest.
References
- Hockenberry, Marilyn J, Wilson D (2019) Wong's nursing care of infants and children. E-book. Elsevier Health Sciences.
- Valizadeh L, Ajoodaniyan N, Namnabati M, Zamanzadeh V, layegh V (2013) Nurses' viewpoint about the impact of Kangaroo Mother Care on the mother–infant attachment. Journal of Neonatal Nursing 19(1): 38-43.
- Valizadeh L, Namnabati M, Zamanzadeh V, Badiee Z (2013) Factors affecting infant's transition from neonatal intensive care unit to home: A qualitative study. Iranian journal of nursing and midwifery research 18(1): 71-78.
- WHO (2003) Department of reproductive health and research: Kangaroo Mother Care. A practical guide. Geneva, Switzerland: World Health Organization.
- Yilmaz F, Küçükoglu S, Özdemir AA, Ogul T, Aski N (2020) The effect of kangaroo mother care, provided in the early postpartum period, on the breastfeeding self-efficacy level of mothers and the perceived insufficient milk supply. The Journal of Perinatal & Neonatal Nursing 34(1): 80-87.
- Boundy EO, Dastjerdi R, Spiegelman D, Fawzi WW, Missmer SA, et al. (2016) Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics 137(1): e20152238.
- White RD, Smith JA, Shepley MM, Committee to Establish Recommended Standards for Newborn ICU Design (2013) Recommended standards for newborn ICU design. Journal of Perinatology 33(Supply1): S2-S16.
- Als H, McAnulty GB (2011) The newborn individualized developmental care and assessment program (NIDCAP) with kangaroo mother care (KMC): comprehensive care for preterm infants. Current women's health reviews 7(3): 288-301.
- Gupta M, Jora R, Bhatia R (2007) Kangaroo Mother Care (KMC) in LBW Infants - A Western Rajasthan Experience. Indian Journal of Pediatrics 74(8): 747-749.
- Salimi T, Khodayarian M, Bokaie M, Antikchi M, Javadi S (2014) Mothers’ Experiences with Premature Neonates about Kangaroo Care: Qualitative Approaches. Intern J Pedi 2(1): 75-82.
- Blomqvist Y, Frolund L, Rubertsson C, Nyqvist K (2013) Provision of Kangaroo Mother Care: supportive factors and barriers perceived by parents. Scand J Caring Sci 27(2): 345-353.
- Solomons N, Rosant C (2012) Knowledge and attitudes of nursing staff and mothers towards kangaroo mother care in the eastern sub-district of Cape Town. S Afr J Clin Nutr 25(1): 33-39.
- Chisenga JZ, Chalanda M, Ngwale M (2015) Kangaroo Mother Care: A review of mothers׳ experiences at Bwaila hospital and Zomba Central hospital (Malawi). Midwifery 31(2): 305-315.
- Shah U, Banker D, Parikh S, Bala DV (2013) Barriers in Implementing Community Based Kangaroo Mother Care In Low Income Community. NHL Journal of Medical Sciences 2(1): 36-38.
- Chan G, Bergelson I, Smith ER, Skotnes T, Wall S (2017) Barriers and enablers of kangaroo mother care implementation from a health systems perspective: a systematic review. Health policy and planning 32(10): 1466-1475.
- Lester BM, Salisbury AL, Hawes K, Dansereau LM, Bigsby R, et al. (2016) 18-month follow-up of infants cared for in a single-family room neonatal intensive care unit. The Journal of pediatrics 177: 84-89.
- Namnabati M, Zamanzadeh V, Valizadeh LV, Nyqvist KH (2017) Theory of infants' transition management from the neonatal intensive care unit to home: A qualitative study. International Journal of Pediatrics 5(1): 4151-4162.
- Zamanzadeh V, Namnabati M, Valizadeh L, Badiee Z (2013) Mothers' experiences of infants discharge in Iranian NICU culture: a qualitative study. Advances in Neonatal Care 13(4): E1-E7.
- Stadd K, Diehl B, Yenokyan G, Aucott SW (2020) A Kangaroo Care Pathway for NICU Staff and Families: The Proof Is in the Pouch. Advances in Neonatal Care 120(1): 14-24.
-
Sorour Roustazadeh, Fatemesadat Mousaviasl, Mahboobeh Namnabati. Challenges in Neonatal Intensive Care Unit Design: Barriers for Kangaroo Mother Care Implication. Glob J of Ped & Neonatol Car. 4(1): 2021. GJPNC.MS.ID.000576.
Barriers, Kangaroo mother care, Design, Infants, Health care architecture, Intensive care, Mothers, NICU design, Mortality, KMC implementation, Breastfeeding
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






