 Review Article
Review Article
Maternal And Perinatal Health in Sudan
Dr. Ahmed Bashir* and Almana General Hospital Jubail
Professor, Stanley Nelson Laboratory Genetics Department, UCLA, USA
Dr. Ahmed Bashir, Professor, Stanley Nelson Laboratory Genetics Department, UCLA, USA.
Received Date:February 12, 2024; Published Date:February 22, 2024
Introduction
The UN has Millennium Development Goals (MDGs) which includes various goals, and Goals 4 and 5 are as follows: Reduce Child Mortality and Improve Maternal Health. These are MDG Goal 4 targets; a.) Reduce by two thirds, between 1990 and 2015, the under-five mortality rate while MDG Goal 5 specifically has the following targets, a.) Reducing the Maternal Mortality Ratio (MMR) by 75% between 1990-2015, b.) Achieving universal access to Reproductive Health by the end of the year 2015.
The UN launched the Accountability for Women and Children’s Health under MDG 5 and introduced the General Global Strategy for Women and Children’s Health. The government of Sudan, Civil society organizations, and other development partners are urging the commitment of concerned individuals to accelerate progress towards MDG 4 and 5, aiming to reduce childhood mortality. Enhancing the effectiveness of international institutional arrangements is crucial for global reporting, oversight, and accountability in Women and Children’s health.
Sudan is actively working towards achieving the UN’s MDGs but recent reports indicate certain challenges or progress in their efforts. Political backing is seen as a key factor in diminishing maternal mortality and morbidity, especially in developing nations like Sudan. Sudan, facing significant HIV epidemics, is actively participating in the global UN initiative to eliminate new HIV infections among children while preserving maternal health. The objective is to achieve a 50% reduction in maternal mortality among HIV-positive mothers by 2015.
Sudan’s incomplete civil registry systems coupled with a limited correlation of cause of death poses challenges in accurately assessing the progress towards MDG 5. Subsequently, the Maternal Mortality Estimation Inter-Agency Group (MMEIG) comprising the World Health Organization (WHO), the United Nations Children’s Fund (UNICEF), United Nations Population Fund (UNFPA), the United Nations Population Division (UNPD) and the World Bank, along with a team from University of California at Berkeley, United States of America, collaborates to produce internationally comparable Maternity Mortality Ratios (MMR). Sudan has actively participated, evolving both methods and data sources for MMR, showcasing improvements over time.
Consultations with Sudan and other countries were conducted
following the development of MMR estimates, serving several
purposes:
1. Provide the country the opportunity to review the country
estimates,
2. Provide the data methods and sources,
3. Obtain additional primary data source that might not
have been given, reported or used;
4. Establish dual understanding of the weakness and
strength of available data and ensure broad ownership of the
results.
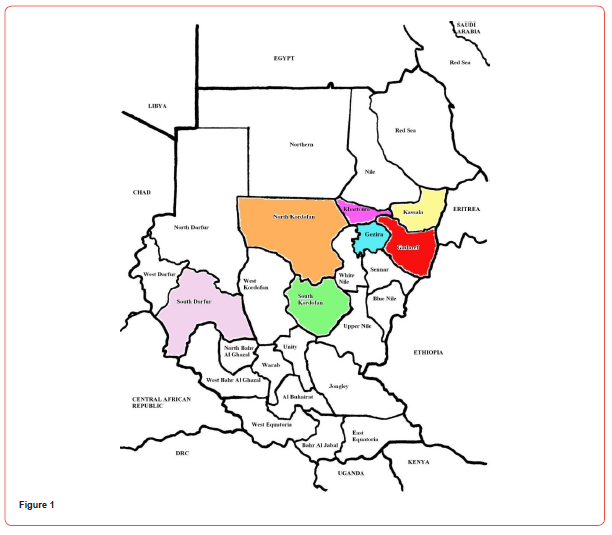
This report presents Sudan estimates of maternal mortality adapted from the global UN estimates of maternal mortality in 2010, as well as trends from 1990 to 2010.The main source is from Situation Analysis (SA) study done collaboratively by Population Council and Sudan Ministry of Health (MOH) with Funds from UNFA, UNICEF, and Packard Foundation. The study took place in seven States, namely: Gadarif, Gezera, Kassala, Khartoum, North Kordofan, South Kordofan, and South Darfur and excluding nine states (as it is part of South Sudan since 2005). Among the states in this study, three do not share borders (North Kordofan, Khartoum, and Gezera) while the rest are bordered by other countries including Eretria and Ethiopia (Gadarif), Central Africa and South Sudan (South Darfour), Eretria (Kassala). The population of these nations utilize shared health facilities due to the limited or nonexistent health resources within their borders. To enhance health levels in these borders states, collaborative efforts with neighboring countries are essential to bolster their health resources. Otherwise, improvements in health facilities within these states may benefit neighboring populations, making it challenging to measure and enhance health outcomes effectively.
Concepts and Definitions
International statistical classification of diseases and related
health problems, 10th revision (ICD-10), defined Maternal Death
as: the death of a woman while pregnant or within 42 days of
termination of pregnancy, from any cause related or aggravated by
pregnancy or it is management, (irrespective of duration and site of
pregnancy), but not from accidental or incidental causes. These are
further divided into:
(i) Direct maternal mortality are those resulting from
obstetrical complications of pregnancy state (pregnancy, delivery,
or postpartum), intervensions, omissions, incorrect treatment, or
any other sequele from the above mentioned causes. Examples
of direct causes of death included but not limited to, obstetric
haemorrhage, hypertensive disorders in pregnancy, complications
of anesthesia, or caesarean section.
(ii) The indirect causes comprise of those resulting from
previously existing diseases, or diseases that developed during
pregnancy aggravated by physiological effects of pregnancy,
example are renal and cardiac diseases.
The formally referred as “pregnancy-related death” or the now called “death during pregnancy, childbirth and pueperum” is defined as any death temporal to pregnancy, childbirth, pureperum period, even if it’s due to accidental or incidental causes. This later definition is helpful in setting where accurate information about causes of death based in medical certificate is unavailable as in rural areas in Sudan.
In Sudan, population-based surveys provides information in the pregnancy-related status rather than maternal deaths, while in modern world (as complications of pregnancy can extend beyond six weeks postpartum, due to increased availability of modern lifesustaining procedures and technologies it enables more women to survive the adverse outcomes of pregnancy and delivery.
Coding Maternal Deaths
The UN successfully established a standardized definition for maternal death; nevertheless, determining accurate causes in developing countries remains challenging due to home deliveries and limited applicability of civil registration systems in various regions.
Despite the World Health Organization’s publication of the ICD- 10, its implementation was lacking in numerous countries, with Sudan being one of them. In 2012, WHO introduced the ICD-MMR aiming to assist countries in reducing errors in coding maternal deaths.
The correlation between HIV and pregnancy reveals an exacerbating impact of pregnancy on HIV infection, potentially resulting in maternal death categorized as indirect cause. In cases of IDS, pregnancy is incidental, with a woman’s demise often attributed to complications related to AIDS, termed as AIDS-related death.
Accurate reporting of both HIV or AIDS and pregnancy on death certificate will enhance precise coding and identification of maternal deaths.
Measures of maternal mortality
Two major factors measures the extent of maternal mortality:
(i) The risk of death in a single pregnancy or single live birth.
(ii) The fertility level.
Moreover there are other items to be defined;
MMR (Maternal Mortality Rate): the number of maternal death
in a population divided by the number of Live birth. The Maternal
Mortality Rate is defined as the number of maternal deaths in a
population divided by the number of women aged 15-49 years. This
will capture the maternal death per pregnancy (both live birth and
stillbirth) and the level of fertility in the population.
PM (Proportion of Maternal Deaths): is calculated by the
number of maternal deaths divided by the total deaths among
women aged 15-49 years.
Approaches for measuring maternal mortality
Several factors obscure the attainment of precise civil registry
accuracy in Sudan and other developing nations. Some of these
reasons include:
1. Lack of precise identity of deaths of women in the
reproductive age or no record at all.
2. Even if the deaths were reported, the cause of death might
not be known and has not been reported as maternal death.
3. In Sudan and many developing countries medical
certifications of cause of death is not practiced in many
provinces, accurate attribution of female death as a maternal
death is difficult to achieve.
Even within developed nations with established death registration systems, there remains the potential for misclassification of ICD-10 coding.
Underreporting of maternal deaths is often prevalent in the
following circumstances or contexts:
- maternal deaths at the early pregnancy months, or those
which was not linked to birth outcome
- Late postpartum deaths.
- Deaths in very young or very old (at extremes of maternal
ages)
- Miscoding by ICD-9 or ICD-10 as in Cerebrovascular and
Cardiovascular diseases.
Inaccuracies in reporting maternal mortality may arise from a deficient comprehension of ICD rules. Death certificates may omit pertinent information such as pregnancy, driven by concerns over legal repercussions or a deliberate inclination to withhold details like abortion. To address the limitations posed by incomplete or inaccurate civil registration systems, diverse alternative sources including household surveys, census calculations, reproductive age and mortality studies (RAMOS), and verbal autopsies, are utilized to substitute MMR estimates. However, it is crucial to acknowledge the substantial constraints inherent in these methods when attempting to accurately estimate maternal mortality levels within given population.
In 2006 Sudanese National Unity Government and the Government of Southern Sudan jointly reported a staggering Maternal Mortality Rate (MMR) of 1,107 per 100,000 live births, positioning Sudan among the nations with the highest maternal mortality worldwide. Furthermore, for each maternal death, an alarming 20 women endure consequences such as obstetric fistula, vaginal prolapse, infertility or, depression. The primary direct causes of maternal mortality in Sudan encompasses hemorrhage, infection, unsafe abortion, and pregnancy-induced hypertension, while the indirect causes include malaria, anemia, and hepatitis. (Sudanese Government of National Unity and the Government of South Sudan 2006, Kenaro et al, .2009). Concurrently, Sudan faced a notable infant mortality rate of 81 per 1,000, with half of these deaths occurring within the neonatal period, specifically in the first month of life. Asphyxia, sepsis, and preterm deliveries emerged as the predominant contributors to infant mortality in the region. These findings underscore the urgent need for comprehensive maternal and infant health interventions to address the multifaceted challenges faced by Sudan in reducing maternal and neonatal mortality rates. (Sudanese Government of Unity and the Government of South Sudan, 2006)
The United Nations proposed four pillars for ensuring maternal
safety:
1. Family Planning (FP)
2. Antenatal Care (ANC)
3. Skilled birth attendance (skilled health personnel,
commodities, drugs, and equipment) and
4. Emergency obstetrics and neonatal care.
In order to prevent to prevent maternal mortality or disability,
there are three delays model:
(i) Delay in making decisions to seek healthcare
(ii) Delay in reaching appropriate care
(iii) Delay in receiving care in health facilities
The health authorities in Sudan should design programs to manage obstetrics complications and to prevent maternal death or injury. (UNFPA: No Woman Should Die giving Life)
Methodology for 1990-2010 estimates of Maternal Mortality and Infant Mortality in Sudan
Leveraging the Situational Analysis (SA) Criteria established by the Reproductive Health Ministry of Health-Sudan and supported by funding from UNFPA, UNICEF, and the Packard Foundation, this study systematically assessed the current state of health in Sudan. Conducted across seven states - Khartoum, Kassala, Gadarif, Gazera, North Kordofan, South Kordofan and South Darfour- the evaluation involved 348 healthcare facilities.
These facilities (Primary, Secondary and Tertiary) were scrutinized for their preparedness to deliver reproductive health services, with a concurrent evaluation of the quality of the services provided. A comprehensive approach included 909 participants composed of physicians, nurses, midwives, and Health Officers, 1,029 Village Midwives (VMW), 1,0313 clients seeking advice, and 1,012 antenatal care visitors.
Finding
Availability and Accessibility of Reproductive Health Services:
Khartoum State (the Capital) has the highest Health facility
Staff (28 per facility), Kassala having the lowest (10 per facility).
Family Planning
Antenatal Care
Skilled Birth Attendance
Emergency Obstetrics Care
Acknowledgment
None.
Conflicts of Interest
None.
-
Dr. Ahmed Bashir* and Almana General Hospital Jubail. Maternal And Perinatal Health in Sudan. Glob J of Ped & Neonatol Car. 4(3): 2024. GJPNC.MS.ID.000590.
Maternal Health, Global Strategy, Society organizations, Global reporting, Children’s health, Neighboring populations, Physiological effects, Death during pregnancy
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






