 Research Article
Research Article
What is the Real Gain in Lumbar Lordosis with Stand-Alone ALIF Cages?
João Gabriel Belegante Scalabrin1*, André Luis Sebben1, Álynson Larocca Kulcheski1, Pedro Grein Del Santoro1, Felipe de Negreiros Nanni1, João Elias Braga1 and Xavier Soler I Graells1,2
1Hospital do Trabalhador, Orthopedics and Traumatology Service, Spine Surgery Group, Brasil
2Universidade Federal do Paraná, Curitiba, Brasil
Corresponding AuthorJoão Gabriel Belegante Scalabrin, Hospital do Trabalhador, Orthopedics and Traumatology Service, Spine Surgery Group, Curitiba, PR, Brasil
Received Date:August 16, 2025; Published Date:August 25, 2025
Introduction
The technique for anterior lumbar interbody fusion (ALIF) began in 1930 with Capener [1] and Burns [2]. Initially, this surgery was associated with high rates of complications due to the transperitoneal approach [3]. However, since 2002, the description of the retroperitoneal approach by Brau [4] revolutionized this procedure, significantly reducing complication rates and making it a safe option for lumbar arthrodesis currently [5].
One of the objectives to be achieved with this technique is the restoration of total lumbar lordosis (LL) [5], as it is directly related to spinopelvic balance, which is crucial for achieving good surgical outcomes [6]. Failure to achieve this balance harmoniously can potentially lead to long-term functional disability and pain [6].
With the aim of restoring this balance, coupled with the good results obtained by the ALIF technique, many surgeons have utilized lordotic anterior cages. No study to date has demonstrated the actual gain in segmental lordosis that an anterior lumbar cage without pedicular instrumentation can promote. Therefore, the objective of the present study is to evaluate the real gain in segmental and total lumbar lordosis, respectively, using anterior cages via the ALIF technique without posterior instrumentation.
Materials and Methods
This was a longitudinal and retrospective study, conducted at a tertiary hospital that is a reference centre for spinal surgery. The study was approved by the Research Ethics Committee (CAAE: 82656124.8.0000.5225). Information was collected from electronic medical records and imaging archives (radiographs) of patients who underwent spinal surgery using the ALIF technique between January 2018 and January 2023. Lateral (P) radiographs of patients were analyzed at pre-operative (Pre-OP), first postoperative day (POD1), and 12 months post-operative (POD12m). These radiographs were taken with the patient standing, hands crossed anteriorly over the chest, supported on the contralateral shoulder, using a 35x43 cm plate. The radiographs encompassed the entire lumbar curvature, with L1 as the most proximal vertebra and the superior plateau of S1 as the most distal criterion.
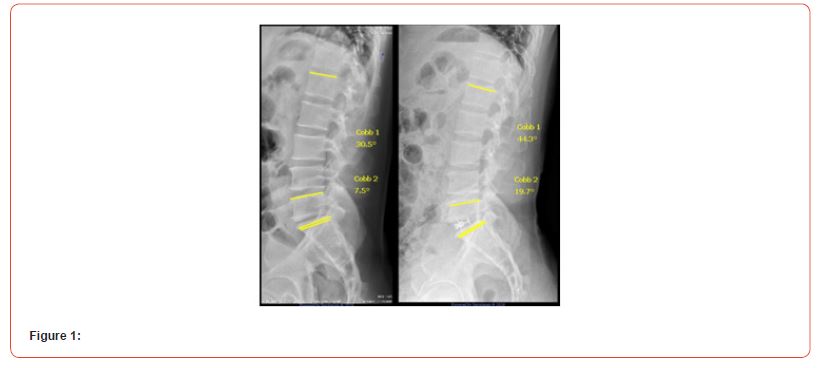
The study included patients aged between 18 and 80 years, who presented with degenerative spinal diseases and underwent surgical treatment using the ALIF technique. Only cases subjected to 1 level of arthrodesis, performed in a stand-alone manner (without posterior supplementation with pedicle screws), and who had a minimum radiographic follow-up of 12 months after surgery, were selected. Exclusion criteria were patients who required any type of revision surgery, those who developed surgical site infection, those who experienced cage subsidence, and those who did not have adequate radiographs for the evaluation of total lumbar lordosis (LL) or segmental lordosis of the operated level. The procedures were performed by 06 spine surgeons who are members of the Brazilian Spine Society, experienced in the technique, and by 3access surgeons. Neither the orthopedic surgeons nor the access surgeons were the same across all surgeries. Radiographic evaluations of segmental lumbar lordosis of the operated level (L4- L5 or L5-S1) and total lordosis (L1-S1) were performed. The COBB technique was used for these measurements (Figure 1).
The cages used for the arthrodesis varied between NUVASIVE®, Globus®, and Orthofix® brands, according to material availability on the day of the procedure. The values found for segmental lordosis (LS) and total lordosis (LL) were compared between Pre- OP, POD1, and POD12m radiographs. These measurements were then associated with the lordotic angulation of each cage used.
Statistical analysis was performed using R Software (version 4.3.2) and Microsoft Excel, in addition to the T-test and ANOVA test for hypothesis evaluation. The T-test verifies the hypothesis that the mean of the observed variable is statistically different from a given reference value. This technique was used to verify if the parameters above showed a statistically different variation from zero (positive or negative). The ANOVA test represents a global hypothesis, i.e., it measures whether at least one of the categories of a certain variable has a statistically different mean from the others (p-value < 0.05 column). It will be applied when the objective is to compare a parameter in relation to sex, for example. For all applied statistical tests, a significance level of 5% (p-value = 0.05) was adopted. When p-value < 0.05, it can be said that there is statistical evidence that the parameter in question showed a gain or loss of lordosis.
Results
For the initial analysis, 165 patients were included. After applying the exclusion criteria, 100 patients remained. 33 (20.1%) were excluded because they underwent anterior and posterior arthrodesis with pedicle screws, 14 (8.5%) due to inadequate radiographs, 14 (8.5%) because they underwent arthrodesis at 2 or more levels, and 4 (2.4%) due to previous surgery (Flowchart 1).
Flowchart 1
“Patient Sampling Flowchart”: Of the 100 eligible patients, 54 (54%) were female and 46 (46%) were male. Age ranged from 18 to 79 years, with 65% of the sample being 46 years or older. The most addressed level was L5-S1 with a total of 95 patients (95%), followed by L4-L5 with 5%. All patients presented with degenerative pathology (100%), and of these, only 7 (7%) had grade 1 listhesis (Table 1).
A greater use of the NUVASIVE® cage was observed, with a total of 71 (71%), followed by the Globus® cage 19 (19%) and Orthofix® 10 (10%). There was no statistical difference in the brand used regarding the obtained results. The angulation of the implant used varied between 8° (5%), 10° (22%), 12° (49%), and 15° (24%) (Table 1).
(Table 2) presents the variables of segmental and total lordosis gain represented as a percentage of gain relative to the cage used. The percentage of segmental lordosis gain at 12 months (%GSeg12m) represents the percentage gain in angulation relative to the cage (real segmental lordosis gain after 12 months). Through the T-test, statistical evidence of segmental lordosis gain by patients was observed (on average 77.7% of the angulation of the cage used).
The percentage of total lordosis gain at 12 months (%GLL12m) represents the percentage gain in angulation relative to the cage (real total lordosis gain after 12 months). Through the T-test, statistical evidence of total lordosis gain by patients was observed (on average 91.9% of the angulation of the cage used).
Table 1: Demographic and Surgical Data.
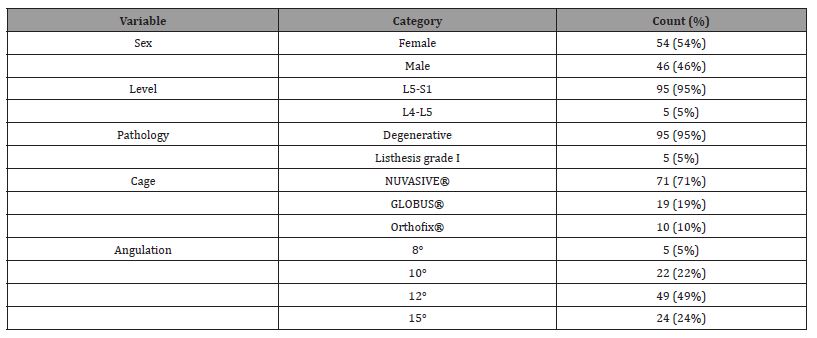
Table 2: Variables of Lordosis Gain.
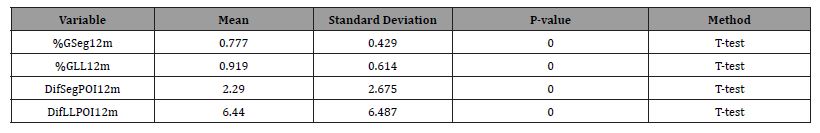
The Difference in segmental lordosis gain between POD1 and POD12m (DifSegPOI12m) represents the difference (in degrees) of segmental lordosis between POD1 and 12 months post-operative. Through the T-test, statistical evidence of segmental lordosis gain by patients 12 months after the procedure was observed. As there is a positive mean, it is stated that, on average, patients had a gain of segmental lordosis (2.29 degrees on average) 12 months after POD1.
The difference in total lordosis gain between POD1 and POD12m (DifLLPOI12m) represents the difference (in degrees) of total lordosis between POD1 and 12 months post-operative. Through the T-test, statistical evidence of total lordosis gain by patients 12 months after the procedure was observed. As there is a positive mean, it is stated that, on average, patients had a gain of total lordosis (6.44 degrees on average) 12 months after POD1.
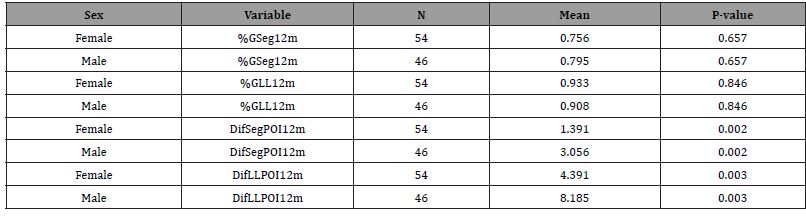
Significant differences were identified between different sexes for the parameters “Difference in segmental lordosis gain between POD1 and POD12m” and “Difference in total lordosis gain between POD1 and POD12m.” It was observed that men exhibit greater gain in segmental or total lordosis (on average) 12 months after the procedure. For the remaining variables, there was no statistically significant difference between men and women (Table 3).
Table 3: Sex vs. Measured Parameters.
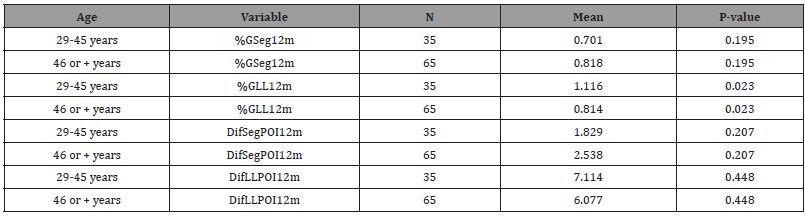
In (Table 4), significant differences can be observed among different age groups for the parameter %GLL12m. It is noted that younger individuals (29 to 45 years) show a greater percentage gain, on average, in total lordosis relative to the cage, 12 months after the procedure. For the other variables, there is no statistically significant difference between different ages.
Table 4: Age vs. Measured Parameters.
Discussion
Currently, the ALIF technique is safe and demonstrates low rates of adverse events [7,8]. It allows for extensive resection of the degenerated disc, restoring its height and lumbar lordosis [9,10]. To achieve spinopelvic balance, surgeons use angled cages according to the need for LS and LL gain [11]. Nanni, Vialle, and Brunet [11] found an average gain of 5.2° in LS when using 12° angled cages, which means 43.3%, and a loss of LL of 3.54° (both measured at POD1), but without a new measurement after a longer period. In the present study, it was observed that after 12 months of surgery, the LS gain was, on average, 77.7% of the angulation of the cage used, which signifies an average gain of 9.3° when using a 12° cage. The LL gain reached 91.9% of the cage’s angulation. These data corroborate the conclusion of the aforementioned authors, who suggest that this loss of lumbar curve at POD1 is due to the antalgic position the patient presents [12,13].
Huec et al. [14] in 2019 presented a series of compensatory mechanisms that can occur after lumbar instrumentation to achieve a harmonious balance between the spine and pelvis. They also demonstrated that the male and younger population, who have more efficient musculature, can adapt better to these changes. In the present study, it is possible to verify that the population aged between 29 and 45 years had a greater gain in lumbar lordosis after 12 months than the population aged 46 years or older (p<0.05) (Table 4). Regarding sex, a statistically significant difference in gain between POD1 and POD12m was observed for the male sex (Table 3).
With these findings, it is possible to affirm that the ALIF technique has the power to effectively restore part of the lumbar curve [15,16], being advantageous compared to more traditional techniques, such as posterior or transforaminal lumbar interbody fusion (PLIF/TLIF) [17]. This is shown by the results of Vialle E et al. [18], where there was a loss of segmental lordosis from 11.4° to 11.06° (p=0.85) after TLIF surgery, whereas in the present study, LS had a significant increase with an average gain of 77.7% of the angulation of the cage used. Regarding total lumbar lordosis, Martinelli et al. [19] found an average loss of -1.6° ± 12.5° (TLIF) and a gain of +2.6° ± 12.1° (PLIF), data much inferior when compared to the technique in this study (ALIF) where total lumbar lordosis corresponded to an average gain of 91.9% of the angulation of the cage used. Several factors can be decisive for this difference, such as the anterior position of the ALIF cage compared to other techniques [20]. Lovecchio et al. [20] reported in their study that 100% of ALIF cages are positioned in the anterior part of the disc space compared to 75% of TLIF cages. They also emphasize the importance of Anterior Longitudinal Ligament (ALL) resection in this technique, further facilitating lordosis gain [20-22]. When the study focuses on evaluating lordosis gain with PLIF and TLIF cages, the result is that they are totally dependent on good surgical technique [20], considering the cage position, posterior osteotomies, and effective discectomy [23-25].
Observing more recent techniques, such as extreme lateral intervertebral fusion (LLIF), also reveals advantages compared to ALIF regarding lumbar lordosis gain [17]. This is what Lazzari et al. [26]’s study shows, reporting a gain of only 26.6% of LL after single-level LLIF. Arnoni et al. [27] found an average gain of 2.55° in segmental lordosis for the LLIF technique with 10° cages, meaning a gain of only 25%, corroborating other studies in the literature [20,28]. It is observed that the same anatomical limitation found for PLIF and TLIF techniques applies to LLIF, i.e., dependence on ALL release and posterior column osteotomies for relevant lordosis gain [20,30]. Thus, the present study provides surgeons with a good perspective on the real lordosis gain that a stand-alone ALIF cage can provide to their patients, enabling more effective pre-operative planning and better post-operative spinopelvic parameter results.
Although the present study provides valuable information about the gain in lumbar lordosis with the use of stand-alone ALIF cages, some limitations should be considered. Firstly, it is a retrospective study, which inherently introduces selection bias and dependence on the quality of data recorded in electronic medical records andimaging files. The sample, although reasonable with 100 patients, was obtained from a single tertiary reference center, which may limit the generalization of the results to other populations or surgical practices. Additionally, the variation in the cages used (NUVASIVE®, Globus®, and Orthofix®) and the angulations of the implants (8°, 10°, 12°, and 15°) may have influenced the results, despite no statistically significant differences being found between them. Finally, radiographic evaluation was performed at only three time points (pre-operative, immediate post-operative, and 12 months), which may not capture the complete long-term evolution of lumbar lordosis. Based on the obtained results, it is important to emphasize that the evaluation of lumbar lordosis over a longer period (beyond 12 months) would allow verification of the durability of the results and identification of possible risk factors for long-term lordosis loss. Furthermore, detailed biomechanical analyses could investigate the impact of different cage characteristics (material, design, angulation) and patient characteristics (pre-operative disc height, sacral slope and pelvic tilt, Roussouly spine types [31]) on lumbar lordosis gain, further refining the obtained values.
Conclusion
The anterior lumbar cages, via the stand-alone ALIF technique at 1 LEVEL, allowed for a real gain in segmental lordosis of 77.7% relative to their original angulation and a gain of 91.9% in total lordosis relative to the angulation of the cage used.
References
- Capener N (1932) Spondylolisthesis. Br J Surg19(75): 374-86.
- Burns B (1933) An operation for spondylolisthesis. Lancet 1: 1233.
- Samudrala S, Khoo LT, Rhim SC, Fessler RG (1999) Complications during anterior surgery of the lumbar spine: an anatomically based study and review. Neurosurg Focus 7(6): e9.
- Brau SA (2002) Mini-open approach to the spine for anterior lumbar interbody fusion: description of the procedure, results and complications. Spine J 2(3): 216-223.
- Felipe Silva Klingelfus, André Luis Sebbenet, Álynson Larocca Kulcheski, Cristiano Silva Pinto, Pedro Grein Del Santoro, et al. (2023) Anterior Lumbar Arthrodesis: Epidemiological, Radiological Profile. Coluna/Columna 22(03): e272928.
- Shulga AE, Zaretskov VV, Ostrovsky VV, Bazhanov SP, Likhachev SV, et al. (2021) Features of the sagittal balance of patients with post-traumatic deformities of the thoracic and lumbar spine. Genij Ortopedii 27(6): 709-716.
- Amaral R, Ferreira R, Marchi L, Jensen R, Nogueira-Neto J, et al. (2017) Stand-alone anterior lumbar interbody fusion - complications and perioperative results. Rev Bras Ortop 52(5): 569-574.
- Härtl R, Joeris A, McGuire RA (2016) Comparison of the safety outcomes between two surgical approaches for anterior lumbar fusion surgery: anterior lumbar interbody fusion (ALIF) and extreme lateral interbody fusion (ELIF). Eur Spine J 25(5): 1484-521.
- Rao PJ, Maharaj MM, Phan K, Abeygunasekara ML, Mobbs RJ. 2015) Indirect foraminal decompression after anterior lumbar interbody fusion: a prospective radiographic study using a new pedicle-to-pedicle technique. Spine 15(5): 817-824.
- Malham GM, Parker RM, Ellis NJ, Blecher CM, Chow FY, et al. (2014) Anterior lumbar interbody fusion using recombinant human bone morphogenetic protein-2: a prospective study of complications. J Neurosurg Spine 21(16): 851-860.
- Nanni FN, Vialle EN, Brunet MD (2020) Radiographic analysis of the results of anterior intersomatic arthrodesis on sagittal lumbopelvic parameters. Coluna/Columna 19(2): 104-107.
- Rao PJ, Ghent F, Phan K, Lee K, Reddy R, et al. (2015) Stand-alone anterior lumbar interbody fusion for treatment of degenerative spondylolisthesis. J Clin Neurosci 22(10): 1619-1624.
- Rao PJ, Phan K, Giang G, Maharaj MM, Phan S (2017) Subsidence following anterior lumbar interbody fusion (ALIF): a prospective study. J Spine Surg 3(2): 168-175.
- Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28(9): 1889-1905.
- Teng I, Han J, Phan K, Mobbs R (2017) A meta-analysis comparing ALIF, PLIF, TLIF, and LLIF. J Clin Neurosci 44:11-17.
- Phan K, Thayaparan GK, Mobbs RJ (2015) Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion - systematic review and meta-analysis. Br J Neurosurg 29(5): 705-711.
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1(1): 2-18.
- Vialle E, Schleifer D, Carneiro A, Colina O, Vialle LR 2015) Changes in radiographic parameters after minimally invasive lumbar interbody fusion. Coluna/Columna 14(4): 265-267.
- Martinelli TC, Effgen EA, Brazolino MAN, Cardoso IM, Maia TC, et al. (2018) Evaluation of the discal height gain and lumbar lordosis variation obtained by the techniques of transforaminal and posterior lumbar intersomatic fusion. Rev bras ortop 53(5): 527-531.
- Lovecchio FC, Vaishnav AS, Steinhaus ME, Othman YA, Gang CH, et al. (2020). Does interbody cage lordosis impact actual segmental lordosis achieved in minimally invasive lumbar spine fusion? Neurosurg focus 49(3): E17.
- Watkins RG IV, Hanna R, Chang D, Watkins RG III (2014) Sagittal alignment after lumbar interbody fusion: comparing anterior, lateral, and transforaminal approaches. J Spinal Disord Tech 27(5): 253-256.
- Lee N, Kim KN, Yi S, Yoon Ha, Dong Ah Shin et al. (2017) Comparison of outcomes of anterior, posterior, and transforaminal lumbar interbody fusion surgery at a single lumbar level with degenerative spinal disease. World Neurosurg 101: 216-226.
- Robertson PA, Armstrong WA, Woods DL, Rawlinson JJ (2018) Lordosis recreation in transforaminal and posterior lumbar interbody fusion: a cadaveric study of the influence of surgical bone resection and cage angle 43(22): E1350-E1357.
- Hong TH, Cho KJ, Kim YT, Jae-Woo Park, Beom-Ho Seo, et al. (2017) Does lordotic angle of cage determine lumbar lordosis in lumbar interbody fusion? Spine (Phila Pa 1976) 42(13): E775-E780.
- Jagannathan J, Sansur CA, Oskouian RJ Jr, Kai-Ming Fu, Christopher I Shaffrey (2009) Radio-graphic restoration of lumbar alignment after transforaminal lumbar interbody fusion. Neurosurgery 64(5): 955-964.
- Lazzari FF, Kulcheski ÁL, Sebben AL, Santoro PGD, Benato ML, et al. (2023) Thoracic-Lumbar Arthrodesis Via Extreme Lateral Approach: A Retrospective Study. Coluna/Columna [Internet] 22(3): e250452.
- Arnoni D, Amaral R, Pokorny GH, Moriguchi R, Pimenta L (2022) Impacto dos parâmetros espinopélvicos pré-operatórios na correção de lordose segmentar após fusão intersomática lombar por via lateral de um ní Revista Brasileira de Ortopedia 57(05): 828-835.
- Acosta FL, Liu J, Slimack N, David Moller, Richard Fessler, et al. (2011) Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine 15(1): 92-96.
- Sharma AK, Kepler CK, Girardi FP, Frank P. Cammisa, Russel C. Huang et al. (2011) Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech 24(4): 242-250.
- Lovecchio F, Qureshi SA (2019) The current state of minimally invasive approaches to adult spinal deformity. Curr Rev Musculoskelet Med 12(3): 318-327.
- Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30(3): 346-353.
-
João Gabriel Belegante Scalabrin*, André Luis Sebben, Álynson Larocca Kulcheski, Pedro Grein Del Santoro, Felipe de Negreiros Nanni, João Elias Braga and Xavier Soler I Graells. What is the Real Gain in Lumbar Lordosis with Stand-Alone ALIF Cages?. Glob J Ortho Res. 5(2): 2025. GJOR.MS.ID.000609.
-
Anterior Lumbar Interbody Fusion (ALIF); Lumbar Lordosis (LL); Segmental Lordosis (SL); Stand-alone Cage; Spinopelvic Balance
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






