 Research Article
Research Article
Use of a New Arthrometer to Assess Knee Pathology
Sommer Hammoud1, Kerstin M Palombaro2, Dawn T Gulick3*
1Rothman Institute, Philadelphia, PA USA
2Widener University, Chester, PA USA
3Widener University, Chester, PA USA
Corresponding AuthorDawn T Gulick, Widener University, Chester, PA USA.
Received Date: December 16, 2021; Published Date: January 06, 2022
Abstract
Purpose: The purpose of this study was to compare the results of Mobil-Aider testing on the involved and uninvolved knees of individuals with
anterior cruciate ligament (ACL) injuries to MRI results.
Methods: Individuals with reported knee injuries (N=26) were tested for ACL laxity using the Mobil-Aider arthrometer. A foam bolster was used
to position the knee in 20-30° flexion. The arthrometer was used to perform a Lachman test on the tibio-femoral joint. The maximal translation of 3
measurements on each knee was recorded. The clinical data and the MRI results were matched.
Result: For the test of between-subject differences, an interaction effect was found between side and MRI result (p = 0.008). A simple main
effect was found in between involved versus uninvolved side (p = 0.001). There was no simple main effect size found for MRI result (p = 0.415).
Conclusion: Excessive anterior translation of the knee is part of the patient presentation of an ACL injury. The clinician should also be cognizant
of the mechanism of injury, the report of a “pop,” presence of rapid swelling, loss of range of motion, and instability. This is the first study using the
Mobil-Aider to assess ACL injuries. Although the device has been validated and determined to be reliable in prior studies of healthy individuals,
testing individuals with injuries are important to demonstrate its clinical value. The sample size is limited but the study was adequately powered to
be able to state the Mobil-Aider has the potential to provide valuable clinical information when assessing ACL injuries.
Keywords: Knee sprain; ACL injury; Lachman technique; Arthrometer
Introduction
There are over 7.2 million orthopedic injuries annually in the USA. Approximately 6.6 million knee injuries presented to United States emergency departments between 1999 and 2008 [1]. It has been estimated 40% of all sports related injuries are of the knee. Of those knee injuries, anterior cruciate ligament (ACL) damage is the most common (over 200,000 per year). Furthermore, it has been estimated that approximately 74% of acute ACL injuries are missed in the emergency department [2].
Part of the challenge in assessing ACL damage is the technique used. The Lachman test is considered the gold standard with sensitivity of 63-99%, specificity of 42-100%, (+) likelihood ratio of 1.12-40.81, and (-) likelihood ratio of 0.02-0.83 [3-14]. The wide range of the statistical data can be related to the criteria for a positive test. Are the positive criteria a lack of an end feel or excessive anterior translation relative to the contralateral side? As a dichotomous test, what constitutes “excessive translation?” It is generally believed that when excessive translation is considered, 5 millimeters or more of increased anterior knee translation on the KT-1000 test is indicative of an ACL either torn or stretched to the point where it is no longer functional [15]. Likewise, Bach et al (1990) reported a side-to-side KT-1000 difference of 0.2 mm is considered normal and differences of 4.8 and 5.5 mm are present in acute and chronic ACL injuries, respectively [16].
Until recently, the KT1000 was the only clinical device used to quantify ACL injuries. However, there are a number of interfaces in the use of the KT1000. The device straps on the knee in a very precise way but the function of the device actually pulls it away from the anterior tibia. If the straps are not secured tightly, a gap occurs between the device and the tibia. This can produce an erroneous value. The counter force to stabilize the proximal leg is delivered via the patella. It is not only uncomfortable, but also not consistent with the Lachman technique of stabilizing the femur. In fact, several studies have reported substantial variability in the measures using the KT1000/2000 [17-19]. Wiertsema et al [20] examined the reliability of the KT1000 arthrometer and found the intra-rater reliability and the inter-rater reliability to be low (ICC = 0.47 and 0.14). Barcellona et al [17] stated that the KT1000 and KT2000 knee joint arthrometers (MEDmetric Corp, San Diego, CA) have been shown to over-estimate the measurement of knee joint sagittal laxity between 22% and 24%.
In 2021, the development of the Mobil-AiderTM (Figure 1) (Therapeutic Articulations, LLC, Spring City, PA) sought to address the pain points of quantifying ACL laxity via simple positioning, stabilizing the femur with contoured attachments, and the use of a light-weight tool that pulls the tibia into the device in the same format as the Lachman test (Figure 2). The Mobil-Aider TM has been shown to be valid in the lab (2% margin of error) when compared to the Zeus Smartzoom [21]. Clinical testing of the posterior translation of the shoulder and volar translation of the wrist have demonstrated reliability of 0.77-0.83 and 0.90, respectively [22- 23].
Magnetic resonance imaging (MRI) is often used for ACL injury diagnosis [14,24]. However, the ability of MRI to identify partial ACL tears has been called into question [25]. Furthermore, MRI is a static image and offers no data about the dynamic instability of the knee (Figure 1&2).


The purpose of this study was to assess the ability of the Mobil- AiderTM device to identify injury to the ACL. The goals were 1) to see if the Mobil-AiderTM consistently identified laxity associated with ACL injuries; 2) identify the magnitude of the anterior displacement present in injured, partial, and complete tears as compared to intact contralateral ACL; and 3) compare the magnitude of displacement with that of the MRI.
Methods
Participants
Eligible participants were anyone over 18 years of age who was suspected to have an anterior cruciate ligament injury or had an MRI with confirmed ACL damage. Participants needed to have an uninjured contralateral knee for comparison. Individuals who had a prior surgery were not eligible. All participants had a scheduled appointment with the researcher (SH) for a suspected knee injury. At the conclusion of the knee examination, the study was explained to the patient, and s/he was asked if s/he was willing to give permission to test his/her knees. Researcher #3 (DG) obtained consent and performed the testing. The uninvolved knee was tested first, then the involved knee. Researcher #3 was blinded to the MRI results prior to testing.
Procedure
The testing procedure involved placing a foam bolster under the knee to obtain a standardized amount of flexion (approximately 20- 30 degrees) in the supine position (figure 2). The tibio-femoral joint line was identified. The device axis was aligned with the joint line and secured on the knee with Velcro straps around the thigh and the calf. The device was set in the “A” mode to hold the maximal reading of anterior translation of the tibia on the femur (Lachman test). The maximal translation of 3 measurements was recorded on the data form for each knee. The MRI results were obtained. The MRI was interpreted by a musculoskeletal radiologist and confirmed by a fellowship trained orthopaedic surgeon (SH). Both the radiologist and surgeon were blinded to the Mobil-AiderTM measurements. The clinical data and the MRI results were matched.
Statistical analysis
The MRI data was coded as “0” for intact ACL, “1” for partial damage to the ACL, and “2” for complete tear of the ACL. A two-way ANOVA was used to compare the ACL laxity of the involved versus uninvolved knee with the MRI result after determining that the data were normally distributed, and Levene’s equality of error variance test had no significant differences. Data were analyzed using SPSS version 27 (IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). Descriptive statistics including frequencies, means and standard deviations were calculated in order to describe the sample.
Result
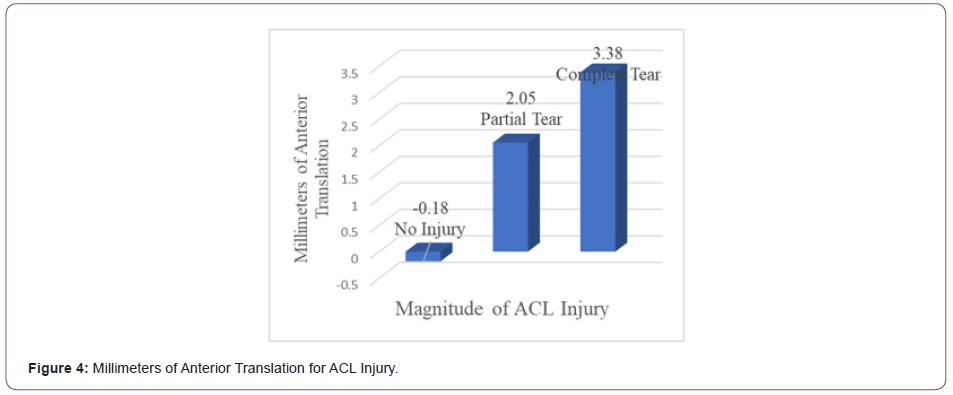
The participants in the study included 12 females and 14 males with a mean age of 32.3 (SD=13.0). Nine had left knee involvement and 17 had right knee involvement. Six were found to have no ACL tear, 10 had a partial and 10 had a full ACL tear. The means and standard deviations of the involved/uninvolved knees for each condition are displayed in Table 1. The mean difference between the involved and uninvolved knees were -0.18, 2.05, and 3.38 for the no tear, partial tear, and complete tear, respectively (Table1).
Conclusion
The present review shows that minimally invasive percutaneous US-guided surgery for CTR offers multiple technical possibilities. As only four of these techniques have been the focus of RTCs, more work is needed to assess the efficacy of this approach in improving the pain and hand functionality problems experienced by patients with CTS.
Table 1: Mean, Standard Deviation of Involved/Uninvolved Knees with MRI Results.
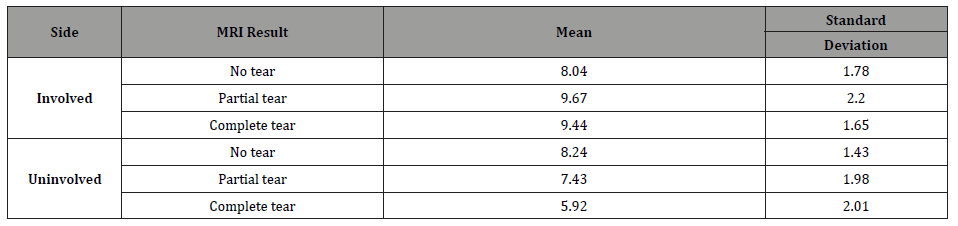
For the test of between-subject differences, an interaction effect was found between side and MRI result (p = 0.008). A simple main effect was found in between involved versus uninvolved side (p = 0.001). There was no simple main effect size found for MRI result (p = 0.415).
Discussion
The Lachman test is a passive accessory movement performed on the knee to assess the integrity of the ACL. Despite being widely accepted in the orthopaedic community, there are several issues related to the performance of the Lachman test. First, a mismatch in the size of the patient’s leg to that of the clinician’s hands can make it difficult to stabilize the knee and obtain maximal anterior tibial translation. Second, positioning of the knee in 20-30 degrees of flexion and relaxation of the hamstring are important to not block the translation of the knee. Finally, the inability to quantify millimeters of translation can be a significant concern when comparing the involved to uninvolved knee.
There are two alternatives to the Lachman to address the larger diameter leg of the patient and/or smaller hands of the clinician. Adler et al [26] described a modification of this method, which they called the “drop leg Lachman test.” In supine, the patient’s leg is abducted off the side of the examining table, and the knee is flexed to 25°. The clinician’s hand stabilizes the femur against the table while the patient’s foot is held between the clinician’s knees. Thus, the examiner’s other hand is free to apply the anterior translation force to the tibia. Another alternative is the “prone Lachman test.” In this position, with the knee in 25 degrees of flexion, the thigh does not need to be stabilized and gravity helps to translate the tibia anteriorly (Figure 3).
The drop leg and prone Lachman both address the issue of a “size” mismatch and even the knee positioning but neither provide any quantification of the amount of tibial translation. When one is applying a significant amount of force to stabilize the thigh and translate the tibia, distinguishing a few millimeters difference between the knees can be very challenging. Endfeel is often used to assess the ACL qualitatively. The lack of an endfeel may be indicative of a complete tear but when a partial tear is present a subjective endfeel will not contribute information about the magnitude of the injury. Thus, having objective values can contribute to the assessment of the ACL is important. Having a valid and reliable device is also important. The statistically significant differences of the magnitude of the linear translation in the knee injuries in this study corresponded to the MRI results (Figure 4). Larger differences between knees (3.38 mm) corresponded with complete tears, while smaller differences (2.05 mm) corresponded with partial tears. Participants with no ACL injury had no difference between the knees (-0.18 mm). Being able to quantify the magnitude of an ACL injury with a dynamic testing technique can assist the clinician in determining a treatment course of action. Although the sample size of this study was limited (N=26), it was found to be adequately powered (81.8%) for the interaction effect of side and MRI result. As an introductory study for using the Mobil-Aider TM on joint pathology, the current study demonstrates the device has promise for accurately quantifying ACL laxity (Figure 4).

Clinical Significance
Excessive anterior translation of the knee is part of the patient presentation of an ACL injury. The clinician should also be cognizant of the mechanism of injury, the report of a “pop,” presence of rapid swelling, loss of range of motion, and instability. This is the first study using the Mobil-AiderTM to assess ACL injuries. Although the device has been validated and determined to be reliable in prior studies of healthy individuals [21-23,27-29], testing individuals with injuries are important to demonstrate its clinical value. The sample size is limited but the study was adequately powered to be able to state the Mobil-AiderTM has the potential to provide valuable clinical information when assessing ACL injuries.
Acknowledgement
The authors wish to acknowledge Ms. Kelsey Curlen, MS, LAT, ATC for her commitment to patient scheduling. We would also like to thank Ms. Emma Johnson, Research Fellow, for her assistance with the IRB process.
Conflicts of Interest
Dr. Dawn T Gulick declares she holds the patent for the Mobil- Aider device.
References
- Gage BE, McIlvain NM, Collins CL, Fields SK, Comstock RD (2012) Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med 19(4): 378-385.
- Guillodo Y, Rannou N, Dubrana F, Lefevre C, Saraux A (2008) Diagnosis of anterior cruciate ligament rupture in an emergency department. Journal of Trauma 65(5): 1078-1082.
- Jonsson T, Althoff B, Peterson L (1982) Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparative study of the Lachman test and the anterior drawer sign. American Journal Sports Medicine 10(2): 100-102.
- Logan MC, Williams A, Lavelle J (2004) What really happens during the Lachman test: a dynamic MRI analysis of tibiofemoral motion. American Journal Sports Medicine 32(2): 369-375.
- Cooperman JM, Riddle DL, Rothstein JM (1990) Reliability and validity of judgments of the integrity of the anterior cruciate ligament of the knee using the Lachman test. Physical Therapy 70(4): 225-233.
- Frank C (1986) Accurate interpretation of the Lachman test. Clinical Orthopedics 213: 163-166.
- Benjaminse A, Gokeler A, van der Schans CP (2006) Clinical diagnosis of an anterior cruciate ligament rupture: A meta-analysis. Journal Orthopedics Sports Physical Therapy 36(5): 267-288.
- Lui SH, Osti L, Henry M, Bocchi L (1995) The diagnosis of acute complete tears of the anterior cruciate ligament. Journal of Bone & Joint Surgery 77(4): 586-588.
- Hardaker WT, Garrett WE, Bassett FH (1990) Evaluation of acute traumatic hemarthrosis of the knee joint. Southern Medical Journal 83(6): 640-646.
- Tonino AJ, Huy J, Schaafsma J (1986) The diagnostic accuracy of knee testing in the acutely injured knee. ACTA Orthopedia 52(4): 479-487.
- Jain DK, Amaravati R, Sharma G (2009) Evaluation of the clinical signs of anterior cruciate ligaments & meniscal injuries. Indian Journal of Orthopedics 43(4): 375-378.
- Boyer P, Dijan P, Christel P, Paoletti X, Degeorges R (2004) Reliability of the KT-1000 arthrometer (Medmetric) for measuring anterior knee laxity: comparison with Telos in 147 knees. Review of orthopedic surgery and repair of the motor system 90(8): 757-764.
- Arneja A, Leith J (2009) Review article: Validity of the KT-1000 knee ligament arthrometer. Journal of Orthopaedic Surgery 17(1): 77-79.
- Huang W, Zhang Y, Yao Z, Ma L (2016) Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta Orthopedic Traumatology 50(1): 22-31.
- La Prade R (2021) https://drrobertlaprademd.com/kt-1000-testing-for-acl-tear.
- Bach BR, Warren RF, Flynn WM, Kroll M, Wickiewiecz TL (1990) Arthrometric evaluation of knees that have a torn anterior cruciate ligament. J Bone Joint Surg Am 72(9): 1299-1306.
- Barcellona MG, Christopher T, Morrissey MC (2013) Bench testing of a knee joint arthrometer. Orthopedics 36(8): e1000-e1006.
- Forster JW, Warren-Smith CD, Tew M (1989) Is the KT1000 knee ligament arthrometer reliable? Journal of Bone and Joint Surgery (Br) 71(5): 843-847.
- Graham GP, Johnson S, Dent CM, Fairclough JA (1991) Comparison of clinical tests and the KT1000 in the diagnosis of anterior cruciate ligament rupture. British Journal of Sports Medicine 25(2): 96-97.
- Wiersema SH, van Hooff HJA, Migchelsen LAA, Steultjens MPM (2008) Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. The Knee 15(2): 107-110.
- Gulick DT (2020). Novel Device to Quantify ACL Laxity. Journal of Health Sciences & Medicine.
- Tuzson A, Tarleton G (2021) Validating the Mobil-AiderTM to measure joint accessory motion in healthy adult shoulders. Open J Health Sci Med 2(1): 106.
- O’Donohue JM, Wise CH (2021) Measurement of accessory motion of the glenohumeral and radiocarpal joints: Inter-rater reliability of the Mobil-AiderTM device for measurement of linear translation. Annals of Physiotherapy Clinics 3(1): 1014
- Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J (1988) Anterior cruciate ligament tears: MR imaging compared with arthroscopy & clinical tests. Radiology 166(3): 861-864.
- Mikashima Y, Tomatsu T, Miyawaki M, Koshiishi T, Takagi T, et al. (2016) Can MRI distinguish between a partial anterior cruciate ligament tear and a normal ACL? International Journal of Orthopedics & Rehabilitation 3: 51-57
- Adler GG, Hoekman RA, Beach DM (1995) Drop leg Lachman test: a new test of anterior knee laxity. The American Journal of Sports Medicine 23(3): 320-323.
- Gulick DT (2020) Quantifying joint mobilizations with the Mobil-AiderTM. Journal of Yoga, Physical Therapy and Rehabilitation 5: 1074
- Gulick DT (2019) Proof of Concept: Taking the Guessing Out of Assessing Knee Stability. International Journal of Sports and Exercise Medicine.
- Gulick DT (2019) Reliability and Validity of an Innovative Device for ACL Testing: The Mobil-AiderTM. Journal of Sport Rehab 29(2): 257-261.
-
Sommer Hammoud, Kerstin M Palombaro, Dawn T Gulick. Use of a New Arthrometer to Assess Knee Pathology. Glob J Ortho Res.3(4): 2022. GJOR.MS.ID.000569. DOI: 10.33552/GJOR.2022.03.000569.
-
Galloway-Mowat syndrome, Rare genetic disorder, WDR73 gene, Neurological abnormalities, Kidney disease, Hypotension, Dystonia, Nystagmus, Nephrotic syndrome
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






