 Case Report
Case Report
Sacral Hypogenesis with Fixed Lumbosacral Deformity: A Case Report
Mohannad W Awwad1*, Talal Alghadir1 and Waleed Awwad2
1Medical student, College of Medicine, King Saud University, Saudi Arabia
2Department of Orthopedic surgery, King Saud University, Saudi Arabia
Corresponding AuthorMohannad W Awwad, College of Medicine, King Saud University, Riyadh, 12372, Saudi Arabia
Received Date:August 12, 2025; Published Date:August 20, 2025
Abstract
Background: Congenital scoliosis caused by vertebral malformations such as block vertebrae and sacral hypogenesis often leads to complex spinal deformities, particularly when involving an oblique take-off at the lumbosacral junction. These deformities pose significant surgical challenges related to coronal and sagittal imbalance, pelvic alignment, and neural compression.
Case Presentation: We report the case of a 23-year-old female with longstanding non-progressive scoliosis who developed worsening lower back pain and right-sided sciatica. Imaging revealed a sharp angular lumbar curve secondary to a block vertebra, sacral hypogenesis, and an oblique lumbosacral take-off, with no spinal canal stenosis or cord abnormalities. After comprehensive multidisciplinary evaluation and failed conservative management, the patient underwent posterior spinal instrumentation and fusion from T10 to S2 with S2-alar-iliac fixation, radical facetectomy, partial hemi vertebrectomy, right-sided L4–L5 decompression, and transforaminal lumbar interbody fusion at L5–S1. Intraoperative neuromonitoring was employed throughout.
Conclusions: This case illustrates the importance of multidisciplinary preoperative assessment and meticulous surgical planning guided by deformity-specific classifications. Complex congenital lumbosacral deformities with oblique take-off require focused correction at the lumbosacral junction combined with robust pelvic fixation and neural decompression when indicated. Despite anatomical challenges, such carefully tailored surgery can significantly improve patient outcomes.
Introduction
Congenital scoliosis results from vertebral malformations occurring during early embryogenesis, typically between the third and sixth weeks of gestation. These include failures of formation (e.g. hemivertebrae) and segmentation (e.g. block vertebrae), or combinations thereof, leading to progressive spinal deformity depending on type, anatomical location, and the biomechanical environment during growth [1–3]. The lumbar spine, although less commonly affected than the thoracic region, presents unique diagnostic and therapeutic challenges due to its central role in spinal balance, pelvic alignment, and neural integrity. Block vertebrae arising from segmentation failure may induce sharp, angular curves- especially when associated with asymmetric growth or adjacent anomalies. The situation becomes more complex in the presence of sacral hypogenesis (or agenesis), a rare congenital entity characterized by partial or complete underdevelopment of the sacrum (also termed caudal regression or sacral agenesis). This anomaly, which may be associated with maternal diabetesand exhibits variable neurological, musculoskeletal, and visceral involvement [4,5], can substantially compromise spinopelvic alignment, stability, and load transfer [6,7].
In congenital deformities involving the lumbosacral region, an oblique “take-off” at the lumbosacral junction is of particular concern. Such obliquity not only distorts the biomechanical axis of the spine but also predisposes to pelvic obliquity and trunk imbalance, increasing the risk of curve progression and functional impairment [8]. Moreover, sacral agenesis has been identified as an independent risk factor for postoperative coronal imbalance in surgical management of lumbosacral deformities, highlighting the necessity for vigilant preoperative detection and appropriate spinopelvic stabilization strategies [6]. Together, these multifaceted anatomical subtleties underscore the complexity of congenital lumbar deformities involving vertebral segmentation failures, sacral anomalies, and oblique lumbosacral alignment. Understanding their interplay is critical for optimizing early diagnosis, surgical planning, and long-term outcomes.
Case Description
A 23-year-old female with a known history of scoliosis for over 13 years presented with longstanding waist asymmetry that had remained non-progressive during adolescence. In recent years, however, she developed gradually worsening lower back pain accompanied by right-sided sciatica. The pain was persistent, disabling, and significantly affected her daily activities and overall quality of life. Extensive multidisciplinary evaluation and comprehensive conservative management- including structured physical therapy, pharmacologic treatment, and image-guided pain interventions-were undertaken but provided only minimal and transient relief.
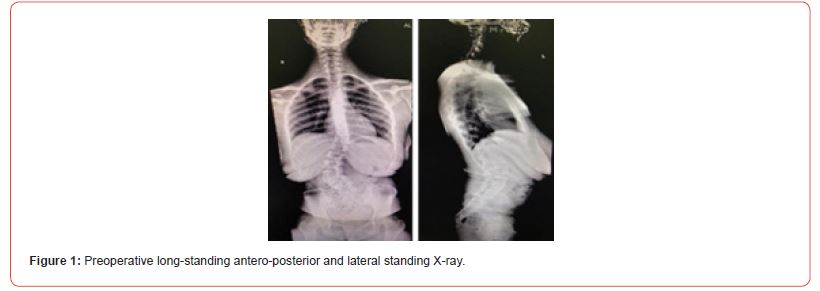
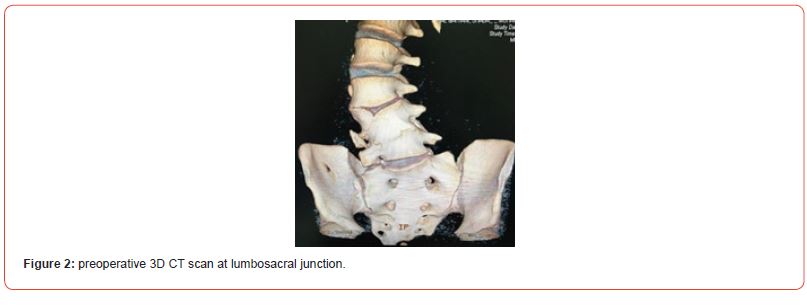
Radiographic assessment, comprising standing full-length spinal radiographs (Figure 1), three- dimensional computed tomography (CT) reconstruction (Figure 2), and magnetic resonance imaging (MRI), confirmed congenital scoliosis. The deformity was characterized by a sharp, angular lumbar curve secondary to a block vertebra, sacral hypogenesis, and an oblique take- off at the lumbosacral junction. No evidence of spinal canal stenosis or intrinsic spinal cord abnormality was identified. Systemic screening for other congenital anomalies-including renal ultrasonography, echocardiography, and detailed neurological examination-yielded unremarkable results.
Management and Follow Up
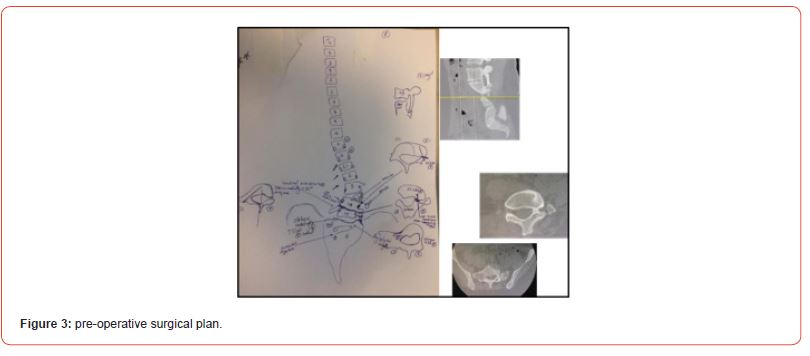
Following multidisciplinary discussion, detailed preoperative planning was performed (Figure 3). Under continuous intraoperative neuromonitoring, the patient underwent posterior spinal instrumentation and fusion extending from T10 to S2 using bilateral S2-alar-iliac (S2AI) screws. Surgical correction included a radical left-sided facetectomy and partial hemi vertebrectomy to address the angular deformity. Additionally, a right-sided L4– L5 decompression was performed to relieve neural compression responsible for her radicular symptoms. A transforaminal lumbar interbody fusion (TLIF) at L5–S1 was carried out to enhance segmental stability and promote fusion at the lumbosacral junction.
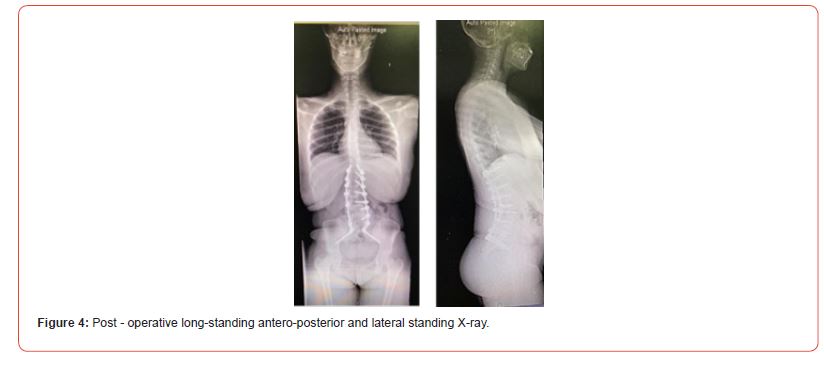
The procedure was completed without intraoperative complications. The patient was monitored in the intensive care unit for 24 hours postoperatively as part of routine care before being transferred to the ward. She demonstrated marked improvement, with significant reduction in both back pain and radicular symptoms noted early in the postoperative period. At the one-year follow-up, the patient remained neurologically intact and reported sustained clinical improvement. Radiographic follow-up demonstrated maintenance of the corrected oblique lumbosacral take-off and satisfactory restoration of coronal and sagittal spinal alignment, with stable instrumentation and no evidence of hardware failure (Figure 4).
Discussion
The surgical strategy in this case was guided by the treatmentoriented classification system for coronal malalignment (CM) in adult scoliosis and spinal deformity proposed by Obeid, Berjano, and Lamartina [9]. This framework is particularly valuable for determining the optimal level of correction based on the type of CM present. In their system, concave CM (Type 1) warrants primary correction at the apex of the scoliotic curve, while convex CM (Type 2)-frequently associated with an oblique take-off at the lumbosacral junction-requires correction at the lumbosacral level to restore coronal balance. Although developed for adult spinal deformity, this classification can be extrapolated to congenital scoliosis cases that share similar deformity mechanics, as in the present patient. Our case demonstrated a Type 2 CM pattern, which dictated a surgical plan emphasizing correction at the lumbosacral junction.
Congenital scoliosis due to vertebral anomalies such as block vertebrae and sacral hypogenesis presents significant surgical challenges, especially when combined with lumbosacral obliquity. The fixed and often rigid nature of such deformities requires a comprehensive strategy that addresses both the structural curvature and associated spinopelvic parameters to optimize coronal and sagittal alignment [2,10]. In our patient, the deformity’s sharp angular nature, combined with pelvic obliquity, necessitated a multi-faceted correction involving resection, decompression, and robust pelvic fixation
Surgical strategies for such cases typically include posterior spinal instrumentation and fusion, hemivertebra or partial vertebrectomy for focal deformity correction, and S2-alar-iliac (S2AI) fixation for achieving durable lumbopelvic stability [11,12]. In patients with concurrent neural compression, decompression and interbody fusion may be indicated to relieve radicular symptoms while maintaining segmental stability [13]. The present case utilized a combination of radical facetectomy, partial hemi vertebrectomy, right-sided L4–L5 decompression, and transforaminal lumbar interbody fusion (TLIF) at L5–S1-allowing both angular correction and neural decompression in a single-stage posterior approach.
Postoperative coronal imbalance is a recognized risk following deformity correction, particularly when preoperative factors such as significant L4 tilt, inadequate lumbosacral correction, or mismatched correction ratios between thoracolumbar and lumbosacral curves are present [13-15]. In congenital scoliosis, these risks are compounded by atypical vertebral morphology and pelvic asymmetry [10]. Targeted correction at the lumbosacral junction and meticulous preoperative planning are therefore essential to prevent persistent or iatrogenic malalignment. The satisfactory radiographic and clinical outcomes observed in this case underscore the importance of these principles.
The choice of S2AI screws for pelvic fixation offered biomechanical advantages, including lower profile hardware, reduced risk of prominence, and improved load distribution compared to traditional iliac bolts [12,16]. Additionally, TLIF at L5– S1 supported fusion in a zone prone to pseudarthrosis, particularly in the context of high mechanical demand and altered sacropelvic anatomy. From a broader perspective, this case highlights the applicability of adult spinal deformity classifications to complex congenital presentations, the critical role of individualized surgical planning, and the value of combining decompression with corrective fusion to optimize both functional and structural outcomes. Longer-term follow-up is warranted to monitor maintenance of correction and fusion integrity, especially given the elevated risk of adjacent segment disease and implant-related complications in such anatomically complex cases [17].
Conclusion
Congenital scoliosis with complex deformities such as block vertebrae, sacral hypogenesis, and an oblique lumbosacral takeoff presents significant diagnostic and surgical challenges. This case underscores the critical importance of a multidisciplinary approach to comprehensive preoperative evaluation, ensuring identification of associated anomalies and optimization of patient status prior to surgery. Meticulous preoperative surgical planning, guided by established classification systems and individualized deformity analysis, is essential for achieving effective correction while minimizing complications.
Surgical management must carefully balance the potential for functional improvement against the inherent risks posed by sagittal imbalance and spinopelvic deformities. The use of intraoperative neuromonitoring and advanced navigation technologies is indispensable for enhancing surgical safety in the context of distorted and atypical anatomy where conventional landmarks are absent or unreliable. Despite these complexities, appropriately planned and executed surgical intervention can result in meaningful improvement in pain, neurological function, and spinal alignment, as demonstrated by the favorable clinical and radiographic outcomes in this patient. This case reinforces that tailored, evidence-based strategies integrating deformity-specific considerations are key to optimizing outcomes in congenital scoliosis with challenging lumbosacral pathology.
References
- Hedequist D, Emans J (2007) Congenital scoliosis: A review and update. J Pediatr Orthop 27(1): 106-116.
- McMaster M J, Ohtsuka K (1982) The natural history of congenital scoliosis: A study of 251 patients. The Journal of Bone and Joint Surgery 64(8): 1128–1147.
- Kawakami N, Tsuji T, Imagama S, Lawrence GL, Rolando MP, et al. (2009). Classification of congenital scoliosis and kyphosis: A new approach to the three-dimensional classification for progressive vertebral anomalies requiring operative treatment. Spine, 34(16): 1756–1765.
- Jasiewicz B, Kacki W (2023) Caudal regression syndrome-A narrative review: An orthopedic point of view. Children 10(3): 589.
- Zhang H, Guo H, He S, Hui H, Hao D (2018) Sacral agenesis combined with spinopelvic dissociation: A case report and literature review. Medicine 97(37): e12162.
- Zhang T, Shu S, Jing W, Gu Q, Liu Z, et al. (2025) Sacral agenesis: A neglected deformity that increases the incidence of postoperative coronal imbalance in congenital lumbosacral deformities. Global Spine J 12(5): 916-921.
- Schwender JD (2020). Details from discussion citing sacral obliquity as risk for persistent postoperative coronal imbalance. Global Spine Journal 10(3): 589.
- Obeid I, Berjano P, Lamartina C, Chopin D, Boissière L, et al. (2019) Classification of coronal imbalance in adult scoliosis and spine deformity: A treatment-oriented guideline. Eur Spine J 28(1): 94–113.
- Xia L, Xu L, Wang Y (2019) Surgical strategies and outcomes in congenital scoliosis associated with lumbosacral oblique take-off. Journal of Neurosurgery: Spine 31(1): 105–113.
- Sebaaly A, Daher M, Salameh B, Ghoul A, George S, et al. (2022) Congenital scoliosis: A narrative review and proposal of a treatment algorithm. EFORT Open Reviews, 7(5): 318–327.
- Ruf M, Harms J (2002) Hemivertebra resection by a posterior approach: Innovative operative technique and first results. Spine 27(10): 1116–1123.
- Jain A, Hassanzadeh H, Strike SA, Menga E N, Sponseller PD, et al. (2015). Pelvic fixation in adult and pediatric spine surgery: Historical perspective, indications, and techniques. J Bone Joint Surg Am 97(18):1521-1528.
- Bao H, Liu Z, Xu M, (2018) Coronal imbalance in degenerative lumbar scoliosis: Prevalence, influence factors, and correlations with health-related quality of life. Spine 43(15): 1058–1064.
- Diebo BG, Henry JK, Lafage R, Challier V, Oren JH et al. (2016) Predicting cervical alignment required to maintain horizontal gaze based on global spinal alignment. Spine 41(23): 1795–1800.
- Bao H, Yan P, Qiu Y (2020) Coronal imbalance after posterior spinal fusion in adolescent idiopathic scoliosis: Prevalence, risk factors, and clinical implications. Journal of Orthopaedic Surgery and Research 15(1): 328.
- Elder BD, Ishida W, Lo SF, Holmes C, Goodwin CR, et al (2016) Use of S2-alar-iliac screws associated with less symptomatic screw prominence than iliac screws: Radiographic assessment and patient-reported outcomes. Spine 41(1): E19–E25.
- Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab JF et al. (2012). Risk–benefit assessment of surgery for adult scoliosis: An analysis based on patient age. Spine 36(10): 817–824.
-
Mohannad W Awwad*, Talal Alghadir and Waleed Awwad. Sacral Hypogenesis with Fixed Lumbosacral Deformity: A Case Report. Glob J Ortho Res. 5(2): 2025. GJOR.MS.ID.000608.
-
Congenital scoliosis; oblique lumbosacral take-off; sacral hypogenesis; s2-alar-iliac fixation; spinal deformity correction
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






