 Review Article
Review Article
Overview of the Recent Advancements in Surgical Management of Shoulder Instability in the Patients with Ehlers-Danlos Syndrome Diagnosis
Adamus J1*,Roszkowska Z1,Surma A1,Sokalski D1,Struzik S2,Łęgosz P2 and Sibilska A2
1Faculty of Medicine, Medical University of Warsaw, Warsaw, Poland
2Department of Orthopaedics and Traumatology of the Musculoskeletal System, Infant Jesus Teaching Hospital, Medical University of Warsaw, Warsaw, Poland
Corresponding AuthorAdamus J, Faculty of Medicine, Medical University of Warsaw, Warsaw, Poland
Received Date:April 04, 2024; Published Date:May 01, 2024
Abstract
Ehlers-Danlos Syndromes (EDS) are complex connective tissue disorders, historically described over a century ago, but with increasing recognition and classification into 13 subtypes. Among these, hypermobile EDS (hEDS) is the most common, characterized by joint hypermobility and musculoskeletal complications. While genetic tests are lacking, diagnosis relies on clinical manifestation and family history. Patients with shoulder-related hEDS often experience bidirectional shoulder instability, posing challenges in treatment. Traditionally, surgical interventions for EDS, including shoulder instability, faced high failure rates. However, recent advancements have led to more optimistic outcomes. Arthroscopic techniques, such as posterior glenohumeral capsular reconstruction with allografts, have shown promise in stabilizing shoulders, offering benefits like minimal invasiveness, and reduced postoperative pain.
Additionally, open surgical approaches like inferior capsular shift and shoulder arthroplasty have demonstrated effectiveness in improving stability and relieving pain in hEDS patients. Despite concerns about complication rates, long-term studies indicate favorable outcomes, encouraging consideration of surgery in select cases. Modern techniques, such as arthroscopic capsular plication, show potential in optimizing postoperative rehabilitation by addressing joint instability, although they require further research to establish long-term efficacy and reduce associated risks.
Overall, the evolving landscape of surgical management for EDS, particularly in shoulder instability, presents a more hopeful outlook for patients. While challenges remain, including the need for specialized care and the demanding nature of newer techniques, ongoing research and development are essential to refine surgical approaches and improve outcomes in this complex condition.
Keywords:Orthopedic Surgery; Ehlers-Danlos Syndrome; Shoulder Instability; Musculoskeletal Treatment; Joint Hypermobility
Abbreviations:EDS: Ehlers-Danlos Syndrome; hEDS: hypermobile Ehlers-Danlos Syndrome; HCTDs: Heritable Connective Tissue Disorders
Introduction
Ehlers-Danlos Syndromes (EDS) are multisystemic heritable connective tissue disorders (HCTDs) which affects predominantly women [1-4]. It was thought to have occurred with a prevalence of at least 1/5000 [5], but Joanne C Demmler, et al. [2] reported that the incidence is much higher at roughly 10 cases for every 5000 patients. Historically the First comprehensive description of EDS was reported by Tschernogobow in 1892 [6]. The following instances were reported consecutively by two dermatologists Ehlers in 1901 [7] and Danlos in 1908 [8]. The First aforementioned author focused on joints and imperfection of connective tissue; other authors presented cases of the syndrome. However, all of the authors agreed with general syndrome description.
The accelerating development of genetics in recent years allowed us to distinguish many types of EDS. Parallelly the nomenclature of EDS had been improving and in March 2017 the Ehlers-Danlos Society announced the latest actualization of the EDS classification. Currently 13 subtypes of EDS are differentiated [3].
The most common type of EDS is hypermobile Ehlers-Danlos Syndrome (hEDS) [5]. In literature hEDS is characterized by joint hypermobility, systemic manifestation of generalized connective tissue disorder, absence of unusual skin fragility, 1 or more firstdegree relatives meeting current diagnostic criteria for hEDS as well as musculoskeletal complications [9]. In regard to the shoulder joints the main symptoms are subluxation or joint dislocation [9], impaired shoulder function [9,10] and increased shoulder pain [10]. There are no genetic tests available to diagnose patients with hEDS, therefore the clinical manifestation and positive family history are crucial for accurate diagnosis [3]. Additionally, in the study performed by Bo Song, et al. the problem of shoulder-related hEDS was common and involved 78% of hEDS patients participating in the study [5].
In clinical practice it is uncommon to differentiate the subtypes of EDS. However, each patient with the EDS should receive specialized care. The patients with shoulder-related EDS frequently suffer from bidirectional shoulder instability [1]. And due to connective tissue disfunction the treatment of EDS-patients has been challenging not only in orthopedics. Past researchers reported [1,11] that the surgical treatment of EDS directly correlated with a great rate of failure of the interventions. In the paper published by Thomas Rogers, et al. [12] it is stated that in case of failed surgical procedure and/or recurring dislocations arthrodesis is both endstage and effective treatment of EDS. It is clear that previous surgical intervention results were dissatisfactory. Some researchers even suggested shoulder-arthrodesis as end-stage procedure [13]. But recently the surgical treatment of EDS has been given a second chance. The new surgical procedures have been developed with much more optimistic results for EDS-patients’ treatment [14,15]. In this article we have collected all available publications and literature regarding surgical management of shoulder-EDS patients.
Arthroscopic surgery management of patients with shoulder instability – the current state of mind.
During the recent years a few articles and technical notes, regarding surgical management of joint hypermobility syndromes including EDS were published (Table 1).
Table 1:Key publications discussed thoroughly in this review.
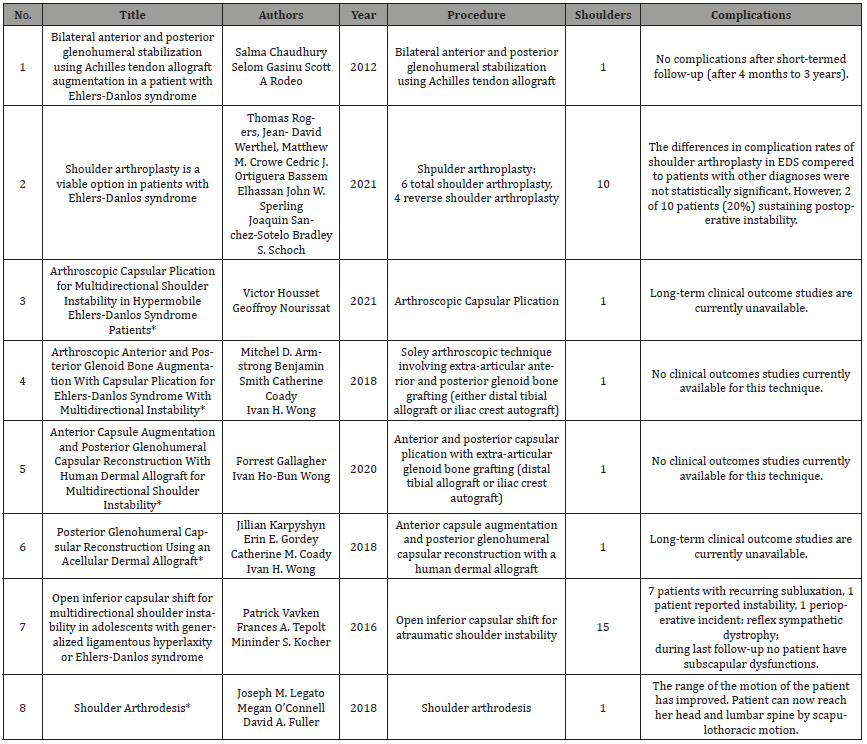
* Technical note.
In 2018 Karpyshyn J, et al. described technique for reconstruction of the posterior glenohumeral capsule with utilization of an acellular dermal allograft in treatment of posterior instability in EDS and a previously failed plication [15]. Even though there are many options in surgical treatment of shoulder instability in EDS, there are a few alternatives for patients who have failed primary repair (approximately 3-25% failure rate in early clinical studies and 6-7% at an average of 36 months after the operation) and also have soft tissue pathology. The quality of the tissue is the main challenge for the operator. This procedure has both advantages as well as disadvantages. The technique described in the article in the great detail offers patient the benefit’s like miniinvasive arthroscopic procedure, no donor site morbidity, maintains native anatomy, utilization of allograft tissue in connective tissue disorders (e.g. EDS) and most last but not least the reduction of postoperative pain in relation to non-arthroscopic procedures. In addition, the application of acellular dermal allografts has been described with promising results in various different procedures for superior capsular reconstruction and open reconstruction of the anterior capsule in anterior shoulder instability [16-18]. The main drawbacks include the risk that the capsule reconstruction may not be sufficient in case of significant glenoid retroversion, the procedure requires the correction of scapular dyskinesia prior to this operation. Even though this technique is acceptable for surgical management of these patients the long-term outcomes are still unknown [15].
According to Gallagher F, et al. the anterior capsule augmentation and posterior glenohumeral capsular reconstruction with human dermal allograft are a viable procedure in multidirectional shoulder instability which includes EDS [14]. As mentioned before, surgical management is especially demanding in patients with connective tissue disorders and there is a need for a breakthrough in the surgical techniques. For this technique the allograft is expected to incorporate itself into the patients’ capsule hence it dissipates posterior directed forces affecting the shoulder. The primary advantages of this procedure lie in the application of arthroscopy which has been proven to have more beneficial outcomes compared to open surgeries. Furthermore, the patients who underwent this operation have greater postoperative range of motion, improved recovery time, lower postoperative pain, and recurrence rates. Here we also achieve the lack of the harvest site morbidity as well as glenohumeral joint reduction. Despite many benefits the disadvantages of the technique, such as skill-dependent nature of the procedure, high cost of allograft, requirement for extremely careful graft insertion and as in previous technical note - the lack of long-term clinical outcomes should have been also taken into the consideration while planning the patient with multidirectional shoulder instability treatment [14].
The latest technical note regarding surgical management of instable shoulders was published by Housset V, et al. and presented the arthroscopic capsular plication for multidirectional shoulder instability in hEDS patients [19]. Authors address recurring problem and challenges regarding performing surgeries on patients with connective tissue disorders, but point out the exceptional difficulty in patients affected by hypermobile type of EDS. The greatest population with hEDS are young and active people that were failed by conventional surgical management of the condition. The authors aim to optimize postoperative rehabilitation by improving proprioception. It is achieved by performing global volume reduction of the glenohumeral joint. This arthroscopic procedure seems promising as it has reduced invasiveness compared to open surgeries, allows for better exploration of both anterior and posterior capsular labral complex and presents no labral or cartilage aggression. However, it has similar drawbacks as aforementioned techniques such as long learning curve, high cost and additionally noticeable loss of range of motion, especially regarding the external rotation.
The other authors e.g., Armstrong, et al. also present allarthroscopic technique involving extra-articular anterior and posterior glenoid bone grafting with utilization of either distal tibial allograft or iliac crest autograft [20]. The technique involves addition of the bony augmentation to the glenoid (which is not present in the traditional procedures) and increasing the contact surface area therefore the shoulder stabilization is more resilient to changes in the joint which would most likely appear with the passage of time e.g., insufficient shoulder stability due to stretching of the plicated capsule. The procedure has similar advantages and disadvantages as aforementioned methods, but here is worth highlighting that both soft-tissue laxity (with capsular plication) and reinforcement of glenohumeral stability (with anterior and posterior glenoid bone graft) take place simultaneously [20].
Open surgical management of patients with shoulder instability
Non-arthroscopic treatment of hEDS patients is still in use. Open inferior capsular shift or shoulder arthroplasty are a viable option in surgical management of hEDS [21,12]. The first method was profoundly analyzed by Vavken P, et al. in the study involving 18 shoulders in 15 hEDS patients. The results showed that 87% of patients reported improved pain and stability, 64% were able to return to sports. Among all the study’s participants 47% had no recurrence of instability, another 47% reported recurrent subluxation and just 1 patient (7%) experienced increased postoperative shoulder instability. Authors report that after the shoulder stabilization the mean follow-up was 7.5 ± 3.5 years, with a minimum follow-up of 32 months. The data clearly presents that inferior capsular shifts can produce predictable quality-of-life improvement in shoulder function in patients with hEDS [21]. On the other hand, Rogers T, et al. in 2021 researched the outcomes of shoulder arthroplasty (SA) in patients suffering from hEDS. The study describes results and complications of two types of shoulder arthroplasties: anatomic total shoulder arthroplasties (6 patients) and reverse shoulder arthroplasties (4 patients).
The follow-up averaged at 60 months and the group’s results were compared to patients who underwent SA due to primary osteoarthritis or cuff tear arthropathy with ratio 1:2, counting 20 patients in the control group. The results are conclusive and show that both cohorts experience comparable pain relief with no significant difference between these groups in VAS pain score forms pre- to postoperatively. The same situation takes place regarding the range of the motion: forward elevation, external rotation, internal rotation. When comparing EDS and non-EDS cohort patients there were no significant difference in complications (3/10 vs. 3/20) and reoperations (0/10 vs. 2/20). Which shows that absolute complication rate in EDS was high (30%), furthermore, 2 of 10 patients experienced postoperative instability [21]. In some cases of failed prior shoulder-stabilization attempts there is still at least one alternative available to help in alleviating patients’ pain and improving joint stabilization-shoulder arthrodesis. This endstage procedure has many indications, multidirectional shoulder instability ergo also EDS is amongst them [13].
The aim of the procedure described by Legato JM, et al. in the publication was to perform an arthrodesis with shoulder prior position of 30 degrees of flexion, 30 degrees of abduction and 30 degrees of internal rotation. At the end the functional motion is assessed via ranging the patient’s elbow so that patient would be able to reach her mouth with ease. Additionally, during follow-up patients’ range of motion increased-she was able to reach the top of her head and lumbar spine through scapulothoracic motion. The results are very promising in this case in particular because she is the patient with refractory shoulder instability who failed previous surgical management [13].
Methods
Two independent researchers found publications by browsing medical data bases (PubMed and Cochrane) using phrases such as “Ehlers-Danlos Syndrome instability shoulder”, “Ehlers-Danlos Syndrome Shoulder”, “Ehlers-Danlos Shoulder Multidirectional” or by utilizing the references of the articles already found. We collected 26 publications. Among which 8 meet inclusion criteria: original publication with described surgical management of the shoulder of the EDS patient. Even though other studies mentioned the topic of shoulder EDS they did not put emphasis on describing surgical management of the shoulder joint. The authors of these articles comprehensively described the diagnosis, symptoms, or physiotherapy of the patient suffering from EDS and having shoulder-related issues, therefore these publications were not included in this review.
Conclusion
The patients suffering from Ehlers-Danlos Syndrome are challenging to diagnose. The lack of genetic tests and vast array of symptoms, including the non-musculoskeletal one’s, adds to the difficulty. Due to the nature of this condition, its relatively high prevalence and most importantly the latest Ehlers- Danlos Society guidelines the number of patients diagnosed with EDS will only increase in the near future. Additionally, the treatment of these patients had not been as effective as we would have assumed. Hence the demand for qualitative and improved ways to manage their condition.
Even though the older academic literature and some publications [1,11] discourage physicians from surgical management of the EDS patients, including shoulder-EDS, the approach to each case should be particularly individual in this condition. According to the latest publications and current state of the knowledge in some cases the operation, either arthroscopic or open, should be seriously considered. Among the procedures mentioned in this review as well as source publications the open inferior capsular shift for atraumatic shoulder instability [21] or shoulder arthroplasty [12] have promising results, with low probability of complications and decreased recurrence of instability. The pioneering arthroscopic techniques that involve allografts [14,15,20] also seem to be a viable and non-invasive alternative for open surgeries. They would bring numerous benefits of arthroscopic surgery over the open surgery. All of the aforementioned publications highlight the fact that the surgical management of EDS in 21st century may be beneficial for the patient, improve their quality of life and even allow them the return to practicing sport. However, it is worth mentioning that the long-term results of the latest arthroscopic techniques are unknown, require new clinical studies and research to decisively prove their effectiveness and decrease complications’ probability. In addition, the newest procedures are as challenging as diagnosing the EDS in itself and have a demanding learning curve. Therefore, it is crucial to broaden our knowledge in surgical management of this condition, develop new techniques and study the long-term results of already invented methods.
Acknowledgements
None.
Conflicts of Interests
The authors declare no conflict of interest.
References
- Song B, Yeh P, Harrell J (2021) Systemic manifestations of Ehlers-Danlos syndrome. Proc (Bayl Univ Med Cent) 34(1): 49-53.
- Tinkle B, Castori M, Berglund B, Cohen H, Grahame R, et al. (2017) Hypermobile Ehlers-Danlos syndrome (a.k.a. Ehlers-Danlos syndrome Type III and Ehlers-Danlos syndrome hypermobility type): Clinical description and natural history. AM J Med Genet C Semin Med Genet 175(1): 48-69.
- Tschernogobow A (1892) Cutis laxa. Moscow Dermatologic and Venereologic Society. Monatsh Prakt Dermatol 14-76.
- Ehlers E (1901) Cutis laxa, tendency to hemorrhages in the skin. Loosening of several articulations (case for diagnosis). Derm Zeitschr 8: 173-178.
- Danlos H. (1908). A case of cutis laxa with tumors due to chronic contusion of the elbows and knees. Bull Soc Fr Dermatol Syphiligr 19: 70-74.
- Homere A, Bolia IK, Juhan T, Weber AE, Hatch GF (2020) Surgical Management of Shoulder and Knee Instability in Patients with Ehlers-Danlos Syndrome: Joint Hypermobility Syndrome. Clin Orthop Surg 12(3): 279-285.
- Johannessen EC, Reiten HS, Lovaas H, Maeland S, Juul- Kristensen B (2016) Shoulder function, pain
- Ericson Jr WB, Wolman R (2017) Orthopaedic management of the Ehlers–Danlos syndromes. Am J Med Genet Part C Semin Med Genet 175(1): 188-194.
- Rogers T, Werthel JD, Crowe MM, Ortiguera CJ, Elhassan B, et al. (2021) Shoulder arthroplasty is a
- Legato J, O'Connell M, Fuller DA (2018) Shoulder Arthrodesis. J Orthop Trauma 32 Suppl 1: S4-S5.
- Gallagher F, Wong IH (2020) Anterior Capsule Augmentation and Posterior Glenohumeral Capsular Reconstruction with Human Dermal Allograft for Multidirectional Shoulder Instability, Arthrosc Tech 9(5): e657-e662.
- Karpyshyn J, Gordey EE, Coady CM, Wong IH (2018) Posterior Glenohumeral Capsular Reconstruction Using an Acellular Dermal Allograft. Arthrosc Tech 7(7): e739-
- Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, et al. (2013) Clinical results of arthroscopic
- Petri M, Warth RJ, Horan MP, Greenspoon JA, Millett PJ (2016) Outcomes After Open Revision Repair of Massive Rotator Cuff Tears with Biologic Patch Augmentation. Arthroscopy. 32(9): 1752-1760.
- Pogorzelski J, Hussain ZB, Lebus GF, Fritz EM, Millett PJ (2017) Anterior Capsular Reconstruction for Irreparable Subscapularis Tears. Arthrosc Tech 6(4): e951-e958.
- Housset V, Nourissat G (2021). Arthroscopic Capsular Plication for Multidirectional Shoulder
- Armstrong MD, Smith B, Coady C, Wong IH (2018) Arthroscopic Anterior and Posterior Glenoid Bone Augmentation with Capsular Plication for Ehlers-Danlos Syndrome with Multidirectional Instability.
syndrome after a first shoulder dislocation. J Shoulder Elbow Surg 27(1): 65-69.
classiTication of Ehlers-Danlos Syndromes. Am J Med Genet C Semin Med Genet 175(1): 8-26.
viable option in patients with Ehlers-Danlos syndrome. J Shoulder Elbow Surg 30(11): 2484–2490.
superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 29(3): 459-470.
Instability in Hypermobile Ehlers-Danlos Syndrome Patients. Arthrosc Tech 10(12): e2767-e2773.
Arthrosc Tech. 7(5): e541-e545.
-
Adamus J*, Roszkowska Z, Surma A, Sokalski D, Struzik S, Łęgosz P and Sibilska A. Overview of the Recent Advancements in Surgical Management of Shoulder Instability in the Patients with Ehlers-Danlos Syndrome Diagnosis. Glob J Ortho Res. 5(1): 2024. GJOR.MS.ID.000596.
-
Orthopedic Surgery; Ehlers-Danlos Syndrome; Shoulder Instability; Musculoskeletal Treatment; Joint Hypermobility
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






