 Research article
Research article
Local Versus Intravenous Application of Tranexamic Acid in Knee Arthroplasty: A Prospective Randomized Study
Bahaa Kornah, Galal Mohamed Mansour Hegazy and Mohamed Tawfiq Ibrahim Mohamed*
Department of Orthopedic Surgery, Faculty of Medicine, Egypt
Mohamed Tawfiq Ibrahim Mohamed, Department of Orthopedic Surgery, Faculty of Medicine, Al-Azhar University, Egypt.
Received Date: June 15, 2020; Published Date: July 09, 2020
Abstract
Purpose Total knee arthroplasty (TKA) is commonly performed for advanced knee joint disease. Considerable postoperative blood loss, however, is an unavoidable occurrence because of extensive soft-tissue release, and the large area of cancellous bone osteotomy associated with the procedure. Besides, knee flexion and extension activities that begin the day after the operation adds to the problem. Aim of the Work: to compare between the intravenous the intraarticular tranexamic acid (TXA) administration in total knee arthroplasty surgery.
Methods: Methods: It is a prospective double-blinded randomized controlled study. This prospective, two-arm, parallel-group study was conducted at El-Hussein University Hospital and El-Agouza Hospital on 20 patients who underwent total knee arthroplasty and fulfilled all assumed inclusion and exclusion criteria.
Result: Results: The average total blood loss amount in the drain after 48 hrs. in the 1st group was 365±74.722 while in the 2nd group it was 575±88.976. This indicates a significant decrease in blood loss amount in the 1st group (intraarticular TXA group) than the 2nd group (intravenous TXA group). Also, it was found that the decrease in hemoglobin (Hb) level is less in the 1st group than in the 2nd group which indicates less postoperative anemia.
Conclusion: Concerning intraarticular administration of TXA seemed to be effective much more than intravenous injection in terms of blood loss amount and transfusion frequency.
Keywords: Blood Loss– Tranexamic Acid –Total Knee Arthroplasty.
Introduction
Total knee arthroplasty (TKA) is commonly performed for advanced knee joint disease, which could lessen pain and greatly improved the knee joint function. The number of total knee surgery increases in clinical application as there is an improved newer surgical technique and implant used. Considerable postoperative blood loss, however, is an unavoidable occurrence because of extensive soft-tissue release, and the large area of cancellous bone osteotomy associated with the operation. Besides, knee flexion and extension activities that begin the day following the operation adds to the problem. Postoperative dominant blood loss after unilateral TKA can reach 1,200–1,900 mL [1,2].
A growing number of elderly patients undergo TKA. This patient group can suffer from many underlying diseases, such as the inability of the hematopoietic system to apply compensatory mechanisms and CVS diseases. As such, hemorrhage could be a serious consequence. Anemia is a key impeding factor in patients’ postoperative recovery. Homologous blood transfusion is often used to solve postoperative anemia, but this carries a substantial risk of immunologic reaction and disease transmission for the patients and also increases medical expenses. Therefore, a reduction in operative blood loss, especially post TKA, is beneficial to recovery and decreases the transfusion risks. The usage of pneumatic tourniquets leads to an increase in the activity of the blood fibrinolytic system (a naturally existing enzymatic system that regulates clot and thrombus formation in the body) [3-5].
Various measures have been tried to decrease the bleeding and subsequently, the transfusion requirements, such as the usage of anti-fibrinolytic agents. Tranexamic acid (TXA) which is a synthetic compound derived from amino acid lysine is acting as a competitive inhibitor of plasminogen activation [6,7]. Tranexamic acid prevents fibrinolysis by competing with the lysine molecule on fibrinogen binding sites and showed effectiveness in reducing blood loss amount, but still the controversy regarding the dosage and the type of administration exists [8].
Aim of the Work
The objective of this randomized comparative study was to compare between the administration route of both intraarticular and intravenous tranexamic acid (TXA) injection in total knee arthroplasty, regarding the blood loss amount and the change in Hb levels preoperatively and 48 hours postoperatively.
Patients and Methods
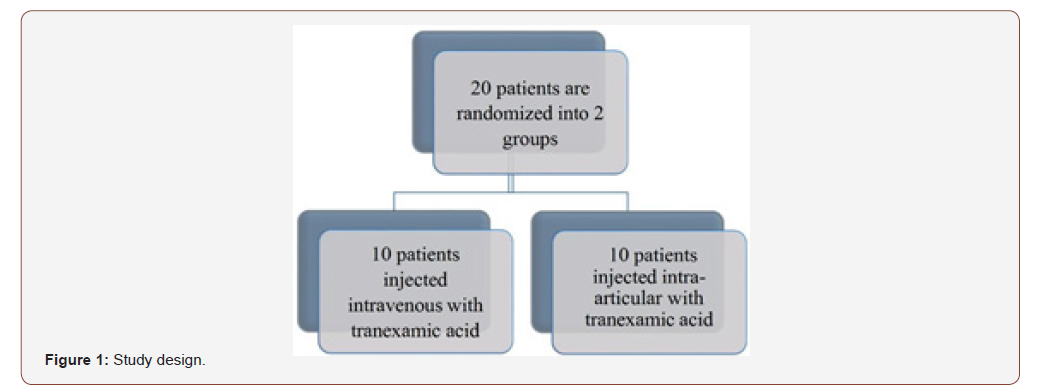
It is a prospective double-blinded randomized controlled study. This prospective, two-arm, parallel-group was performed at El-Hussein University Hospital and El-Agouza Hospital from June 2018 till February 2019 on 20 patients who underwent total knee arthroplasty and fulfilled all inclusion and exclusion criteria. The study design is shown in (Figure 1). The study was approved by the Ethics Board of Al-Azhar University and informed written consent was taken from each participant in the study (Figure 1).
Inclusion criteria
• Patients undergoing unilateral TKA for primary osteoarthritis and rheumatoid arthritis. Age above 55.
• The same approach used for all cases (standard mid-line incision with medial para-patellar).
Exclusion criteria
Patients presenting one or more of the following criteria were excluded from the study:
Patients presenting one or more of the following criteria were excluded from the study:
• History of coagulation or cardiovascular disorders; vascular diseases.
• Current use of anticoagulant drugs.
• Orthopedic surgery in lower extremities.
• Contraindication for TXA use (active intravascular clotting process, acquired defective color vision, subarachnoid hemorrhage, and hypersensitivity to TXA).
Patients
Preoperative patient evaluation
All patients were above the age of 55 years suffering from severe osteoarthritis in the knee joint which was already on medical treatment with no clinical improvement or even by intraarticular injections.
History taking
A full history was obtained about the patients’ symptoms and their duration. All the patients complained of severe pain in knee especially on flexion and having problems walking distances longer than 20 meters without stopping from pain. Full present history was taken from patients about smoking, hypertension, diabetes, cardiac, previous operations, and previous DVT and regular drugs taken by the patients. For Cardiac patients who were taking aspirin 75 mg, aspirin was stopped 5 days before operation day and shifted to low molecular weight heparin (LMWH; enoxaparin sodium 40 mg).
Clinical examination
All patients had a full knee joint examination, tenderness, and inability to do knee flexion was presented in all patients. Furthermore, a flexion deformity or valgus deformity was found in some patients, besides that some of them had visible baker cyst in the knee posterior aspect.
Lab investigation
Preoperative full laboratory investigation was done for all patients; complete blood count, prothrombin time, partial thromboplastin time, INR, fasting, and 2 hrs. postprandial blood sugar, ESR, CRP, ALT, AST, and kidney functions were measured.
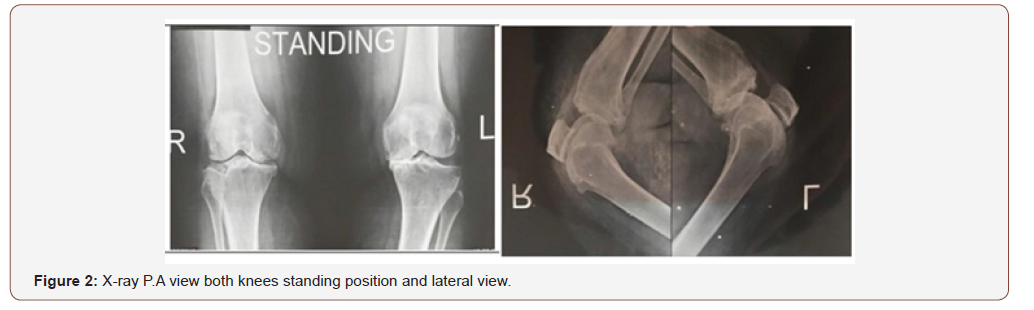
Radiographic evaluation
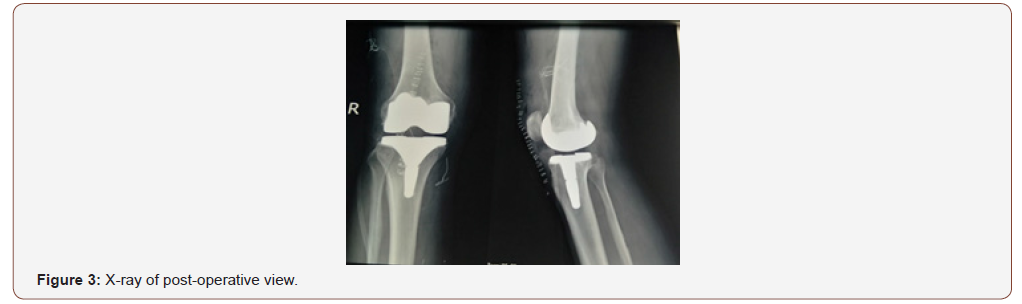
All patients had an X-ray in standing position on both knee joints; anteroposterior and lateral view as in (Figure 2) and postoperative TKR (Figure 2&3).
Methods
Twenty patients underwent total knee replacement surgery divided into equal two groups:
• The first group: 10 cases had intraarticular tranexamic acid (1.5 g injected into the cavity of the knee joint after the closure of the joint capsule).
• The second group: 10 cases received intravenous tranexamic acid (15 mg/kg in 100 mL of saline single dose at the start of operation).
Anesthesia
All patients were operated upon under epidural anesthesia, with tourniquet control of 350 Hg pressure.
Crystalloids in the form of normal saline (NS) were used as a maintenance fluid, also plasma of the same blood group of the patient was used in some of the patients as a maintenance fluid.
All patients were positioned similarly in the supine position.
Surgical technique
A standard midline incision with a medial parapatellar approach was used for all the surgeries. Standard techniques of intraoperative hemostasis were used. The knee implanted used in all cases was posterior stabilized (the cruciate ligaments are removed and parts of the implant substitute for the posterior cruciate ligament) cemented knee (Zimmer). Wounds were closed in layers over the non-suction drain and the drain was closed for 2 hrs.
Postoperative protocol
A similar protocol for both groups was used. Postoperative note for nurse staff to leave the drain closed for 2 hrs. postoperatively and continuous reading for the drain was recorded in patients’ files. Postoperative X-ray on the knee was requested. Complete blood count was done 48 hours after surgery to evaluate Hb level postoperatively.
Prophylactic broad-spectrum antibiotics were used covering both Gram +ve and –ve bacteria. They were given as I.V injection during 5-7 days’ hospital stay then the patients were shifted to oral antibiotics till the first visit which was 10 days postoperatively.
Standard prophylactic measures against venous thromboembolic disorders in the form of subcutaneous injections of low molecular weight heparin (LMWH) was given to all patients once daily from the 1st day till the 21st day postoperatively.
During the first visit in the outpatient clinic evaluation of joint movement, skin edema, clinical evaluation for the presence of DVT, and removal of the stitches and X-ray (AP, lateral views) were done.
Postoperative evaluation
Complete blood count was done 48 hrs. after the operation to evaluate Hb level postoperatively.
Total draining fluids in the drain were documented for 48 hrs. according to the recorded amount in the patient file.
All the results were collected in a personal notebook to be used in statistical analysis
Also, evaluation for DVT clinically was done during the patient stay in the hospital.
Statistical analysis
Data were analyzed using Statistical Package for Social Science, IBM SPSS. Quantitative data were shown as mean± standard deviation (SD). Qualitative data were shown as frequency and percentage.
The following tests were applied:
• An independent-sample t-test of significance was set when comparing two means.
• A paired sample t-test of significance was set when comparing pre- and postoperative means in the same group.
• The (chi-squared) X2 test of significance was set to compare proportions between two qualitative parameters.
• Probability (P-value)
• P-value (<0.05) was considered significant.
• P-value (<0.001) was considered highly significant.
• P-value (>0.05) was considered insignificant
Result
Demographic features
The patients’ age, sex, side of the operation, and co-morbidity (hypertension, smoking, diabetes) are shown in table (1).
• 5 patients are smokers (25.0%) and all are males.
• 14 patients are diabetic (70.0%), all controlled on oral hypoglycemic drugs.
• 10 patients are hypertensive (50.0%), all controlled on oral antihypertensive drugs (Table 1).
Age and Sex
A comparison between both groups according to the age of patients and sex of patients in each group as shown in (table 2).
Table 1: Demographic and co-morbidity features of the study group.

Table 2: Comparison between group I and group II according to demographic data.

This table shows no significant difference between both groups statistically according to age and sex data.
Co-morbidities
A comparison between the 2 groups according to co-morbidity factors (Hypertension, Smoking, Diabetes):
In the 1st group 3 patients were smokers (30.0%), 7 patients were diabetics (70.0%) and 4 hypertensive patients (40.0%), while in the 2nd group 2 patients were smokers (20.0%), 7 patients were diabetics (70.0%) and 6 hypertensive patients (60.0%). There was no statistically significant difference between both groups according to comorbidities.
Side of the operation
Also, another comparison is done between both groups according to the side of TKR done to the patient shown in (table 3).
This table shows no statistically significant difference between both groups according to the side of TKR.
Comparison According to outcomes
Comparison between the Hb level preoperatively and 48 hours postoperatively (Table 4)
This table shows a statistically significant difference between both groups according to the mean Hb drop. The decrease in Hb level is less in the 1st group than in the 2nd group which indicates less postoperative anemia.
Comparison in the total blood loss amount in the drain 48 hours postoperatively between the two groups (Table 5)
This indicates a significant decrease in blood loss in the 1st group (intraarticular TXA group) than the 2nd group (intravenous TXA group) (Table 5).
Table 3: Comparison between group I and group II according to the side of TKR.

Table 4: Comparison between preoperative and postoperative according to Hb in each group.

Table 5: Comparison between group I and group II according to total Redivac Drain in CC.

This table shows a highly significant difference between both groups statistically according to total Redivac Drain drainage in CC.
Patient evaluation
Complete blood count was done 48 hrs. after surgery to evaluate Hb level postoperatively. Total draining fluids in the drain were documented for 48 hrs. according to recorded amounts in the patient file. Clinical evaluation for DVT was done before patient discharge.
Complications
1. DVT
No cases had reported any signs of DVT
2. Infection
No cases had reported fever or any signs of infection.
Discussion
The main common problems after TKA are blood loss and increase the blood transfusion rate with its complication. Considerable postoperative blood loss, however, is an unavoidable occurrence because of extensive soft-tissue release, and the large area of cancellous bone osteotomy associated with the operation. Besides, knee flexion and extension activities that begin the day after the operation adds to the problem [9]. Because TKR is usually performed under tourniquet, the lower limb veins are in a state of hypoxia. This results in the release of tissue plasminogen activator from the vascular endothelium, which promotes fibrinolysis. Tourniquet deflation results in sudden vein expansion in the lower extremity, which leads to increased bleeding [10].
In the current study no, significant difference was obtained when comparing both groups statistically according to demography (age, sex), side of the operation, and comorbidities (hypertension, DM, smoking).
Patients in both groups had a decrease in Hb level postoperatively but it was found that the decrease in Hb level was significantly less in the 1st group than in the 2nd group which indicates less postoperative anemia and blood loss in the 1st group (injected with IA tranexamic acid).
The most important finding in this study was that TXA decreased blood loss in TKR and decreased the need for transfusion accordingly. Comparing two TXA groups, the intraarticular route of TXA seems to be more effective than the intravenous route in terms of the blood loss amount and the need for blood transfusion. Intraarticular injection at the surgical site provides direct and straightforward means of application before tourniquet releasing [11]. Also, intraarticular TXA injection induces partial microvascular hemostasis by preventing fibrin clot dissolution in the operative area. Once injected intraarticularly, TXA is rapidly absorbed and maintains a biological half lifetime within the joint fluid for approximately 3 hrs [12].
A concern exists on the use of TXA that the antifibrinolytic effect of TXA may cause thromboembolic complications in patients given TKA [13]. Due to this concern, cardiac patients or patients with the thromboembolic disease were excluded from this study enrolment. Furthermore, no thromboembolic problems such as DVT or pulmonary embolism were encountered after the intraarticular injection of TXA. In comparison with other literature, many studies prove the efficacy of intraarticular and intravenous TXA in reducing blood loss after TKR. Stowers et al 2017 Multicentered, Randomized, Controlled Trial, they concluded that elective TKA, a single 1.5-g dose of TXA given intraoperatively either systemically or topically effectively reduces blood loss without an increase in complications [14] The best way for the TXA administration will remain the topic of continuous debate and controversy in the upcoming years [15].
Intraarticular application of TXA was investigated by many authors in last years. As the drugs are applied predominantly to the joint cavity, the site of bleeding could achieve a higher therapeutic concentration. This could effectively limit blood loss with minimal or no systemic absorption or subsequent systemic side effects. It is also, easy to administer in this route [15] Other recent studies also concluded that the two types of administration are comparable for blood transfusion incidences after TKR [16-18]. But wang et al 2017 [19] concluded that Intra-articular administration of TXA significantly reduced total blood loss and drainage volume to a greater degree than IV injection in total knee arthroplasty without reduction of HBL A Prospective Randomized Controlled Trial.
Their findings support the postulation that the therapeutic effect of TXA will appear when the proteolysis of plasmin allows the dissolution of the fibrin clot. As TXA works at the site of active bleeding of the wound rather than within the blood vessels, its presence within the clot is considered effective irrespective of the route of administration. However, three recent studies favored intraarticular TXA to intravenous administration [19-21].
Conclusion
Injection of TXA effectively reduced postoperative blood loss and so decreased the need for blood transfusion after cemented TKR. This decreased the hospital stays and permit the patients early mobilization instead of bed stay for 3 days. The patient moved after removal or even before removal of the drain 48 hours postoperatively without evidence of the occurrence of complications.
Concerning the administration route, intraarticular administration of TXA seemed to be more effective than intravenous injection regarding amounts of blood loss and transfusion frequency.
Recommendation
1. All patients who will have TKR surgery should be injected by IA TXA to decrease the blood amount loss postoperatively and to decrease the need for repeated transfusion.
2. More clinical trials are needed to decide the exact dose to double the effect of the TXA with fewer side effects.
3. More studies are needed to see the combined effect of both the IV TXA and the IA route.
4. As this study was done with relatively few numbers of cases and its statistical power wasn’t high enough, and thus, further upcoming studies are required to confirm its findings.s
Acknowledgement
None.
Conflicts of Interest
There are no conflicts of interest in the manuscript, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest. Authors had no disclose for any financial ties to the subject of this research.
References
- Kalairajah Y, Simpson D, Cossey AJ, GM Verrall, A J Spriggins (2005) Blood loss after total knee replacement: effects of computer-assisted surgery. The Journal of bone and joint surgery 87(11): 1480-1482.
- Nadler SB, Hidalgo JU, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2): 224-232.
- Cid J, Lozano M (2005) Tranexamic acid reduces allogeneic red cell transfusions in patients undergoing total knee arthroplasty: results of a meta-analysis of randomized controlled trials. Transfusion 45(8): 1302-1307.
- Ishida K, Tsumura N, Kitagawa A, Sayaka Hamamura, Koji Fukuda et al. (2011) Intraarticular injection of tranexamic acid reduces not only blood loss but also knee joint swelling after total knee arthroplasty. International orthopaedics 35(11):1639-1645.
- Wong J, Abrishami A, El Beheiry H, Nizar N Mahomed, J Roderick Davey, et al. (2010) Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am 92(15): 2503‐2513.
- Rajesparan K, Biant LC, Ahmad M, RE Field (2009) The effect of an intravenous bolus of tranexamic acid on blood loss in total hip replacement. The Journal of bone and joint surgery 91(6): 776-783.
- Zohar E, Ellis M, Ifrach N, Avraham Stern, Oleg Sapir, et al. (2004) The postoperative blood-sparing efficacy of oral versus intravenous tranexamic acid after total knee replacement. Anesthesia & Analgesia 99(6): 1679-1683.
- Eubanks JD (2010) Antifibrinolytics in major orthopedic surgery. JAAOS-Journal of the American Academy of Orthopedic Surgeons 18(3): 132-138.
- Salido JA, Marin LA, Gomez LA Pedro Zorrilla, Cristobal Martinez (2002) Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. JBJS 84(2): 216-220.
- Tai TW, Lin CJ, Jou IM, Chih-Wei Chang, Kuo-An Lai, et al. (2011) Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy 19(7): 1121-1130.
- Chen Y, Chen Z, Cui S, Li Z, Yuan Z (2016) Topical versus systemic tranexamic acid after total knee and hip arthroplasty: A meta-analysis of randomized controlled trials. Medicine 95(41): e4656.
- Laskin RS, Beksac B, Phongjunakorn A (2004) Minimally invasive total knee replacement through a mini- midvastus incision: an outcome study. Clinical Orthopedics and Related Research 428: 74-81.
- Kolisek FR, Bonutti PM, Hozack WJ, James Purtill, Peter F Sharkey, et al. (2007) Clinical experience using a minimally invasive surgical approach for total knee arthroplasty: early results of a prospective randomized study compared to a standard approach. The Journal of arthroplasty 22(1): 8-13.
- Stowers MDJ, Aoina J, Vane A, Poutawera V, Hill AG, et al. (2017) Tranexamic Acid in Knee Surgery Study-A Multicentered, Randomized, Controlled Trial. J Arthroplasty 32(11): 3379‐3384.
- Zhang Y, Fu X, Liu WX et al. (2014) Safety and efficacy of intra-articular injection of tranexamic acid in total knee arthroplasty. Orthopedics 37(9): e775-e782.
- Wong J, Abrishami A, El Beheiry H, Nizar N Mahomed, J Roderick Davey, et al. (2010) Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. JBJS 92(15): 2503-2513.
- Huang Z, Ma J, Shen B, FuXing Pei (2014) Combination of intravenous and topical application of tranexamic acid in primary total knee arthroplasty: a prospective randomized controlled trial. The Journal of arthroplasty 29(12): 2342- 2346.
- Wang H, Shen B, Zeng Y (2014) Comparison of topical versus intravenous tranexamic acid in primary total knee arthroplasty: a meta-analysis of randomized controlled and prospective cohort trials. The Knee 21(6): 987-993.
- Wang J, Wang Q, Zhang X, Wang Q (2017) Intra-articular Application is More Effective Than Intravenous Application of Tranexamic Acid in Total Knee Arthroplasty: A Prospective Randomized Controlled Trial. J Arthroplasty 32(11): 3385‐3389.
- Hamlin BR, DiGioia AM, Plakseychuk AY (2015) Topical versus intravenous tranexamic acid in total knee arthroplasty. The Journal of arthroplasty 30(3): 384-386.
- Seo JG, Moon YW, Park SH et al. (2013) The comparative efficacies of intra-articular and IV tranexamic acid for reducing blood loss during total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy 21(8): 1869-1874.
-
Bahaa Kornah, Galal Mohamed Mansour Hegazy, Mohamed Tawfiq Ibrahim Mohamed. Local Versus Intravenous Application of Tranexamic Acid in Knee Arthroplasty: A Prospective Randomized Study. Glob J Ortho Res. 2(3): 2020. GJOR.MS.ID.000539.
-
Tranexamic Acid, Knee Arthroplasty, Hemoglobin, Blood Loss, Tranexamic Acid, Total Knee Arthroplasty, Inclusion criteria, Radiographic evaluation, Postoperative protocol
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






