 Review Article
Review Article
Lateral Extraarticular Tenodesis in Combination with ACL Reconstruction: Indications, Technique Description
Sebastian Orduna1* and Nagib Atallah Yordi1
Health point Hospital, Abu Dhabi Knee and Sports Center, United Arab Emirates
Sebastian Orduna, Health point Hospital, Abu Dhabi Knee and Sports Center, United Arab Emirates.
Received Date: July 01, 2019; Published Date: July 09, 2019
Introduction
Anterior cruciate ligament (ACL) injury is one of the most frequent injuries in sportsmen with a reported prevalence of around 68.6/100,000 per year [1]. ACL reconstruction (ACLR) is one of the most commonly performed orthopedic procedures. An ACL-deficient knee shows an anterior laxity and a variable degree of associated rotational instability. A variable injury to the lateral capsule-ligamentous structures has been hypothesized in the onset of rotational laxity. Historically, anterior laxity in ACL-deficient knees was surgically treated with isolated extra-articular tenodesis, as described by Lemaire or MacIntosh. This procedure was effective in reducing the rotation of the tibial plateau relative to the femur; however, isolated extra-articular reconstructions provided only moderate control of anterior laxity. In addition, the overall longterm results of these procedures were poor and only few patients reported good to excellent results. The main drawback of these techniques is that they are non-anatomic and do not restore the function of the ACL in preventing anterior tibial translation. These procedures were largely abandoned when single-bundle intraarticular ACL reconstruction emerged as the gold standard surgical treatment of ACL tear. However, traditional trans-tibial ACLR had the disadvantage of inter-related tunnels preparation. This may lead to a vertical femoral tunnel, with insufficient pivoting control. In fact, the most common problem after ACLR is the residual rotational instability, which has been described in 11% to 30% [2- 4].
More anatomic single bundle procedures (for example anteromedially performed femoral tunnel) have the advantage of more horizontal graft with better rotational stability [5-7]. More recently double-bundle technique has been proposed to achieve the anatomic and biomechanics of the native knee. Unfortunately, up to date there is no clear evidence of better control of rotational laxity [8-10]. Rotational instability has been related to the injury and loss of function of the antero-lateral structures [11-12] with the anterolateral ligament receiving increasing interest in recent years. The antero-lateral capsular injury is frequently associated with ACL tears, the capsular avulsion is termed a Segond fracture when associated with bony avulsion of the lateral tibial plateau but does not always include an osseous fragment.
This lesion has been shown to be present in the vast majority of acute ACL injuries and its presence is associated with significantly increased rotational knee laxity [13]. In order to improve the control of pivoting phenomenon in patients with antero-lateral capsule injury, some surgeons have started using the addition of a lateral extra-articular tenodesis to the standard intra-articular ACL reconstruction (ACLR). Nowadays an extra-articular tenodesis is recommended only in patients showing explosive rotatory instability with pivot shift 3+.
Anatomy and Biomechanics
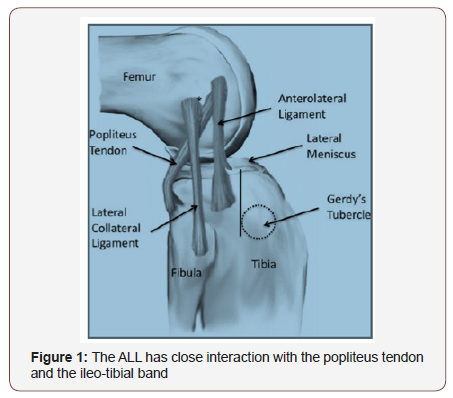
The anterolateral ligament (ALL) takes origin near the popliteus tendon insertion and inserts into the lateral meniscus and tibial plateau 5 mm distal to the articular surface and posterior to Gerdy’s Tubercle [14,15] (Figure 1). The average width of this relatively flat structure is 8.2±1.5 mm, and the average length is 34.1±3.4 mm. Histologic analysis shows a fibrous core surrounded by synovium; additional peripheral nervous innervation and mechanoreceptors have also been showed. Biomechanics studies have shown that ALL section resulted in a significant increase in ATT at 60° and IR at 30°, 45°, and 60° [16]. Therefore, it was postulated that damage of the ALL after knee sprain could be related to the pivot shift phenomenon. On the contrary the role of all in meniscal stability and in the onset of meniscal pathology remains unclear.
Indications and Contraindications
Indications
Extra articular procedures should be considered in cases where the expected failure rate is increased. Therefore, the primary indication for an extra-articular tenodesis is in case of a 3+pivot shift during physical examination. In these patients, isolated intra-articular reconstruction may not completely control excessive anterior tibial translation and internal rotation in the lateral compartment. Other indication is in case of patients with generalized hyperlaxity. Extra-articular augmentation in patients who plan to return to collision sports, in female patients playing contact sports, in case of genu recurvatum >10˚ and when concomitant extensive medial menisectomy is performed. The additional constraint may help to protect these knees from the high loads seen in these sports and may decrease the re-rupture rate. Extra-articular tenodesis should also be considered in patients younger than 20 years of age. It has been shown that these patients are at an increased risk of rerupture of an isolated intra-articular graft. Finally, these augmentations should be performed in revision cases.
Contraindications
The addition of an extra-articular reconstruction is contraindicated in ACL-deficient knees with an associated posterolateral corner injury. In this situation, the lateral augmentation may fix the tibia in a posterolaterally subluxed position. The extra-articular reconstruction should also be carefully considered in skeletally immature patients because of the risk of injury to the femoral physics. Older studies have shown increased risk of lateral tibiofemoral degeneration after an isolated extra-articular reconstruction. This may have been a result of over tensioning of the graft leading to over constraint of the lateral compartment or may have been related to the 4 to 6 weeks of postoperative immobilization
The History of Extra Articular Procedures
Segond was the first to describe a reinforcement of the lateral joint capsule by fibers of the iliotibial band [17]; in addition, this structure showed increased tension during forced internal rotation. Terry and La Prade referred to this reinforcement as the “capsuloosseous layers” of the iliotibial band and associated its injury with increasingly abnormal Lachman, pivot shift, and anterior drawer tests [18,19]. LaPrade and colleagues described the same structure as the “mid-third lateral capsular ligament” [19]. Campos and colleagues called it the “lateral capsular ligament” and Vieira and colleagues referred to it as the anterolateral ligament [20].
Isolated extra-articular proceduress
These operations were proposed as isolated procedures in anterior cruciate deficient knees.
1967 Lemaire procedure [21]:A strip of iliotibial band was harvested detaching it proximally. The strip was prepared and then passed deep to the fibular collateral ligament (FCL), through a femoral tunnel at the attachment point of the head of the lateral gastrocnemius. The graft was then passed deep to the FCL a second time and fixed with sutures to the iliotibial band with the knee flexed to 30 and held in external rotation.
1976 MacIntosh procedure [22]:A strip of iliotibial band was detached proximally and passed deep to the FCL. The strip was then passed through an osteoperiosteal tunnel prepared posterior to the FCL femoral attachment. The graft was then looped through the lateral intermuscular septum and sutured back onto itself at the Gerdy tubercle with the knee flexed to 90 and held in external rotation.
1978 Losee procedure [23]:An iliotibial band graft was detached proximally and passed through a femoral tunnel that originated at the attachment point of the lateral gastrocnemius and ended anterodistal to the FCL femoral insertion site. The graft was then sutured at the Gerdy tubercle with the knee flexed to 30° and held in external rotation.
1979 Arnold and Coker procedure [24]:A strip of iliotibial band was detached proximally, passed beneath the FCL and popliteus tendon, and sutured to the Gerdy tubercle with the knee flexed to 90-100° and the foot held in external rotation.
1979 Ellison procedure [25]:A distally detached strip of iliotibial band with a bone flake was passed deep to the FCL and anchored in a bone trough slightly anterior to its original harvest site at the Gerdy tubercle with the knee flexed at 90° and held in external rotation. The capsular structures were reefed deep to the FCL.
1982 Benum procedure [26]:The lateral one-third of the patellar tendon was harvested proximally with a patellar bone block, passed deep to the FCL, and fixed with a staple within a bony groove deep to the femoral origin of the FCL with the knee flexed to 45° and held in external rotation.
1982 Andrews procedure [27]:Two strips of iliotibial band were detached proximally and sutured a tubulized at their proximal ends. Then, the sutures were passed through 2 parallel tunnels, which originated at the lateral femoral condyle and exited at the medial femoral condyle. After passing through the tunnels in the lateral-to-medial direction, the sutures were tied together over the adductor tubercle. The grafts were fixed with the knee flexed to 90° and held in external rotation. In addition, the grafts were fixed to ensure that the anterior bundle was taut in flexion and the posterior bundle was taut in extension.
1983 Müller procedure [28]:A strip of iliotibial band was detached proximally and fixed with 2 cancellous screws to a point anterior to the junction of the femoral shaft and lateral femoral condyle with the knee held in external rotation.
Modified Andrews procedure [27]:The iliotibial band was divided, and a 20-mmwide portion of the band was detached proximally. The strip of iliotibial band was fixed with a soft-tissue fixation screw and washer at the distal insertion of the lateral muscular septum on the linea aspera, just anterior to the posterior femoral cortex.
1990 Wilson and Scranton procedure [29]:A strip of iliotibial band was detached proximally, passed deep to the FCL and lateral gastrocnemius tendon and sutured back onto itself with the knee flexed to 60° and the foot held in external rotation. This extraarticular reconstruction was used in conjunction with an intra-articular ACL semitendinosus graft reconstruction.
Combined extra-articular procedures
These operations were proposed in addition to ACLR to increase stability and achieve better control of pivot shift phenomenon.
1979 Marshall procedure [30]:It was described as a modification of the original MacIntosh procedure to address both the ACL insufficiency and the lateral structures damage. The central third of the entire extensor mechanism was harvested including part of the prepatellar aponeurotic tissue. The tibial tunnel was prepared in a standard fashion and location; the graft was then passed through this tunnel, into the joint and over the top of the lateral femoral condyle to be fixed on the Gerdy tubercule.
1985 Combined MacIntosh procedure [31]:It is variation of the previous isolated extraarticular tenodesis to perform combined ACLR and lateral tenodesis. A 25cmX4cm ITB strip was obtained keeping the distal insertion in place. The graft was passed underneath the LCL and through a subperiosteal tunnel to exit anterior to the condylar attachment of the lateral intermuscular septum. The strip was then retrieved in the joint, passed in the tibial tunnel and finally through another tunnel running deep from the insertion of the patellar tendon back to the Gerdy’s tubercle. The fixation with non-absorbable suture was performed at three levels: the femoral attachment of the LCL, the exit of the subperiosteal tunnel, and the medial aspect of the tibial tuberosity and at Gerdy’s tubercle.
1986 Zarins and Rowe procedure [32]:The semitendinosus tendon was detached proximally and passed through an obliquely oriented tibial tunnel, across the knee joint, and over the lateral femoral condyle. After passing it over the lateral femoral condyle, the graft was passed deep to the FCL and sutured onto the iliotibial band. Similarly, the iliotibial band was passed deep to the FCL and over the superior aspect of the lateral femoral condyle. After passing over the lateral femoral condyle, the graft was passed across the knee joint, through the same obliquely oriented tibial tunnel as the semitendinosus tendon, and fixed with sutures to the semitendinosus tendon with the knee flexed to 60 and held in external rotation.
1987 Lerat procedure [33]:The lateral third of the patellar tendon with an attached 10– 12 cm strip of quadriceps tendon was harvested. The tibial tunnel was created in a standard fashion and the femoral tunnel emerged just proximal to the LCL insertion. An additional tunnel was then created at the level of the Gerdy tubercle. The patellar bone graft was shaped in order to obtain a press fit fixation in the femoral tunnel while the tibial bone block was retrieved from the tibial tunnel, tensioned with a metallic wire and fixed over a screw. With the knee at 60° of flexion the quadriceps tendon was passed underneath the LCL, through the tunnel under the Gerdy tubercle and sutured to itself.
1989 Ekstrand procedure [34]:It is a personal modification of the combined MacIntosh procedure. A femoral tunnel was prepared to host the graft instead of the “over the top” option.
1998 Marcacci and Zaffagnini procedure [35]:The semitendinosus and gracilis tendons were harvested proximally, sutured together, and passed through a tibial ACL reconstruction tunnel. The graft exited the tibial tunnel intra-articularly and was passed through the posterior aspect of the femoral notch and over the top of the lateral femoral condyle. The graft was then passed deep to the iliotibial band and over the FCL and was fixed distal to the Gerdy tubercle with the knee flexed to 90 and held in external rotation .
2011 Colombet procedure [36]:A 21 cm hamstring graft was prepared after detachment of the tibial insertion. The femoral and tibial tunnels were drilled in a standard manner, while an additional tunnel was drilled from the Gerdy tubercle to the hamstring origin. In case of sufficient length, a 4-strand intra-articular portion (9cm) was used to replace the ACL and 2-strand extra-articular part (12cm) was prepared to perform the lateral tenodesis. In case of insufficient length both the intra and extra-articular portions were prepared in a 2-strand fashion. The graft was then fixed with two screws at the level of tibial and femoral tunnel. The extra–articular portion was passed under the ITB but superficial to the LCL, into the tunnel in Gerdy’s tubercle and finally fixed with an interference screw.
2013 Neyret procedure [37]:This technique was introduced in the nineties; it predicts an “out-in” ACLR using a 9mm central third bone-patellar tendon-bone graft. The tibial bone block used on the femoral tunnel was wider (around 11-12mm) to host a 4.5 mm drill hole. The femoral tunnel was drilled just posterior and proximal to the origin of the LCL. An additional tunnel was created at the level of the Gerdy tubercle. The gracilis tendon, which was prepared for the extra articular tenodesis was passed through the tibial bone block hole to obtain two strands of the same length. The patellar tendon graft was introduced into the knee through the femoral tunnel. The tibial bone block was impacted into the femoraltunnel to achieve a press-fit fixation, securing at the same time the gracilis into the bone tunnel. Tibial fixation was achieved with an interference screw. The two ends of gracilis were passed underneath the LCL and in opposite directions through a bony tunnel created in Gerdy’s tubercle. Final fixation was obtained suturing the ends to each other with the knee held at 30° of flexion.
Antero-lateral ligament reconstruction
2015 Smith procedure [38]:This technique uses both hamstring tendons. The semitendinosus is used for an “all-inside” ACLR, the gracilis to reconstruct the ALL. Two 4.5 mm by 25 mm tunnels are created, one just anterior and superior to the femoral insertion of the LCL and the second halfway between Gerdy’s tubercle and the fibular head, around 1cm below the joint line. A whipstitch is placed in the proximal end of the gracilis tendon, which is then passed into the femoral tunnel and secured with an absorbable fully threaded knotless anchor. The graft is then passed underneath the ITB and into the tibial tunnel. Final fixation is performed with another fully threaded knotless anchor.
2015 Helito procedure [39]:It is a combined procedure involving tripled semitendinosus and single strand gracilis in order to obtain a four-strands ACL and single-strand ALL. Under fluoroscopic control, a 5 mm metal suture anchor is placed at the ALL femoral attachment (3–4 mm distal to the halfway point on Blumensaat’s line). ACL femoral tunnel is performed in an out-in fashion and the tibial tunnel in a standard manner. The graft is retrieved from distal to proximal in order to have the four-strands in the joint. Femoral fixation is performed first, with a linetoline absorbable screw. Tibial fixation is the achieved with a +1 absorbable screw holding the knee at 30° of flexion and neutral rotation. The gracilis is fixed on the femur using the metal anchor. Tibial fixation is achieved with a second suture anchor positioned at the anatomic insertion halfway between Gerdy’s tubercle and the fibular head, 5 to 10 mm below the joint line88. The graft is then passed under the ITB and is fixed with the second anchors sutures at 60–90° of flexion.
2016 Sonnery-Cottet procedure [40]:It is a similar technique, with pediculate hamstring graft. The tibial tunnel is performed in a standard fashion. Two stab incisions are performed to create an additional 3.2mm tunnel connecting the supero-lateral corner of Gerdy’s tubercle and the site of the Segond fracture (more proximal and lateral) is created. The ACL femoral tunnel emerged at the ALLisometric point. ACL graft was fixed with absorbable screws. The remaining part of the gracilis tendon is passed deep to the ITB but superficial to the LCL, through the ALL tibial tunnel and then back through the femoral tunnel in order to create a Y-shaped ALL construct. The ALL graft is fixed with an interference screw in extension and neutral rotation and secured at the ACL femoral tunnel with the ACL graft traction sutures.
2016 Wagih procedure [41]:It is a percutaneous technique of ALL reconstruction using a polyester tape90. A 5mm transverse skin incision is performed at the level of femoral insertion of the ALL (just anterior and distal to the lateral femoral condyle). A 4.5mm tunnel is drilled over a 2.7mmpassing pin. In a similar way, two 4.5mm transverse tunnels are drilled just proximal to the midpoint between the head of the fibula and Gerdy tubercle leaving a 1cm bony bridge. A polyester tape of 4 mm diameter and 60 mm length is loaded over a cortical suspensory fixation button, which is retrieved from the medial femoral tunnel. The two free hands of the tape are passed deep to the ITB and retrieved on the lateral aspect of the proximal tibia. Finally, the two strands are passed through the tibial tunnels and tied together over the 1 cm bone bridge with the knee in 30° of flexion.
Our Technique
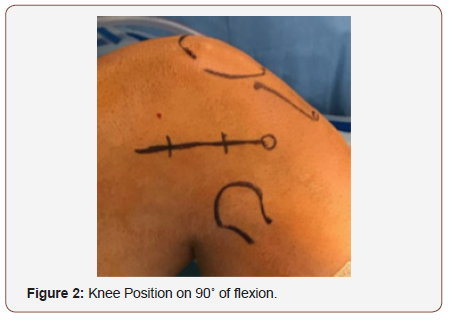
Lateral extra-articular tenodesis (LET) technique was developed to improve the anterolateral capsular structures deficiency. Patient in supine position under femoral block anesthesia. We start the surgery drawing the approach line over the lateral area of the knee, (Figure 2).

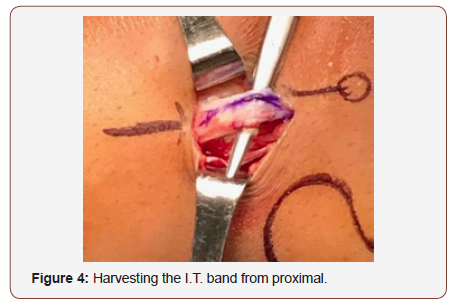
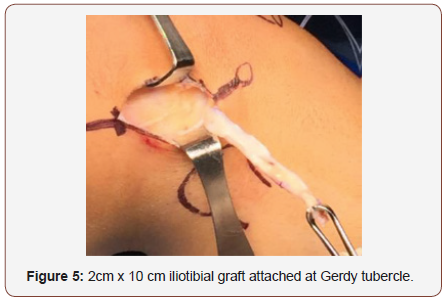
We perform the physical examination of the knee performing Lachman, anterior drawer and Pivot shift, varo-valgo stress tests in 0-30-90 degrees knee flexion. We don’t use hemostatic support active, just keep it in the thigh for some emergency. We perform 4-5 cm approach, after soft tissue release, we reach the Iliotibial band, we use three retractors for marking the fascia late graft 2cm width by 10cm length (figure 3). We release proximally the graft and leave the distal attachment intact on the gerdy tubercle (Figure 4,5).

Then we use a white cottony tape for augmentation the graft and make strong Krakow suture in the end of the graft (figure 6). We indentify the LCL and the graft is passed under the LCL using a right-angle pincer (figure 7,8).


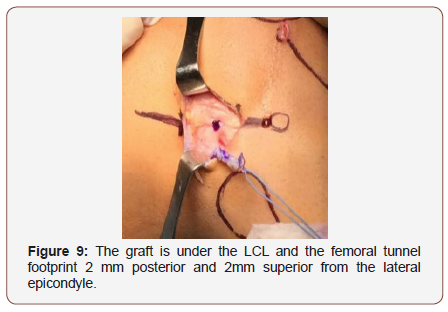
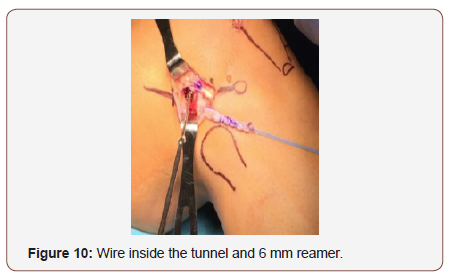
After the graft is placed under LCL, the femoral tunnel is performed, the footprint is situated 2 mm posterior and 2mm superior from the lateral epicondyle (Figure 9). We use a wire passing through both condyle, then we measure the graft width and use the driller for making the tunnel, usually 6-7 mm driller size by 6 cm length (Figure 10).
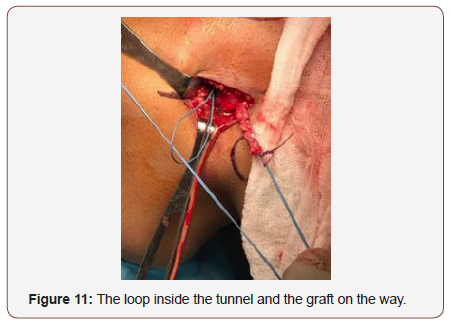
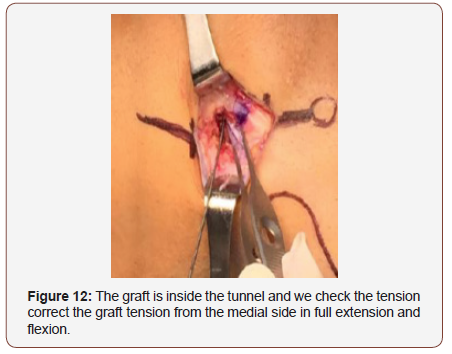
We use the wire guide for passing the irreabsorbible suture and passing the graft through the tunnel. (figure 11). The graft is passed through the tunnel and it is fix temporarily by the time we perform the knee stability tests, and we confirm the full range of motion of the knee without over tensioning the graft either the lateral compartment (Figure12).
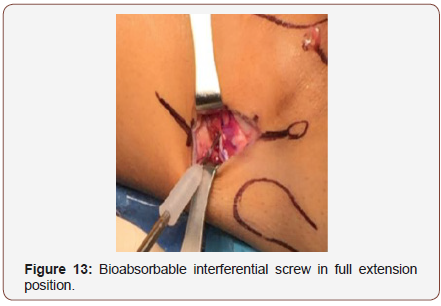
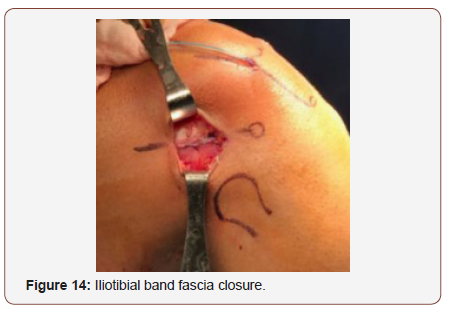
We fix the graft with an interferential bioabsorbable interferential screw in full extension and neutral rotation of the knee (figure 13). We carefully close iliotibial band avoiding overtightening because the patient will complain pain during the postop (figure 14)
We use a drainage 24 hs. We indicate brace for 4 weeks allowing the patient physiotherapy and 0-90 degrees flexion 48 hs post op.
Conclusion
ACLR is a successful procedure both in terms of patients’ satisfaction and sports recovery. However persistent instability and re-rupture rates are still a concern. Anatomic and biomechanics studies have investigated the role of the structures of the lateral and anterolateral aspect of the knee. They contribute to the rotatory stability of the knee, thus preventing the pivot shift phenomenon. Imaging studies have shown high rate of injuries of these structures in patients who have been diagnosed as affected by isolated ACL rupture. It seems therefore reasonable to address the damage of the anteo-lateral structures in the setting of an ACLR at least in specific situations. Current indications include explosive preoperative pivot shift and revision cases. Historic extra-articular procedures have been replaced by more anatomic ALL reconstruction with promising results.
Acknowledgement
None.
Conflict of Interest
No Conflict of Interest.
References
- Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, et al. (2016) Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am J Sports Med 44(6): 1502-1507.
- Anderson AF, Snyder RB, Lipscomb AB Jr (2001) Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med 29: 272–279.
- Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, et al. (2002) Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am 84: 1560-1572.
- Sonnery Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, et al. (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43: 1598-1605.
- Bedi A, Feeley BT, Williams RJ (2010) Management of articular cartilage defects of the knee. J Bone Joint Surg Am 92(4): 994-1009.
- Markolf KL, Jackson SR, McAllister DR (2010) A comparison of 11 o’clock versus oblique femoral tunnels in the anterior cruciate ligamentreconstructed knee: knee kinematics during a simulated pivot test. Am J Sports Med 38: 912-917.
- Kato Y, Maeyama A, Lertwanich P, Wang JH, Ingham SJ, et al. (2012) Biomechanical comparison of different graft positions for single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21(4): 816-23.
- Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: A meta-analysis. Am J Sports Med 36(7): 1414-1421.
- Muneta T, Hara K, Ju YJ, Mochizuki T, Morito T, et al. (2010) Revision anterior cruciate ligament reconstruction by double bundle technique using multi-strand semitendinosus tendon. Arthroscopy 26(6): 769-781.
- Zaffagnini S, Signorelli C, Lopomo N, Bonanzinga T, Marcheggiani Muccioli GM, et al. (2012) Anatomic double-bundle and over-the-top single bundle with additional extra-articular tenodesis: An in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 20(1): 153-159.
- Matsumoto H, Seedhom BB (1994) Treatment of the pivot-shift intra-articular versus extraarticular or combined reconstruction procedures: a biomechanical study. Clin Orthop Relat Res 299: 298-304.
- Bull AMJ, Amis A (1998) The pivot-shift phenomenon: a clinical and biomechanical perspective. Knee 5(1): 141-158.
- Claes S, Bartholomeeusen S, Bellemans J (2014) High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament injured knees. Acta Orthop Belgica 80(1): 45-49.
- Claes S, Vereecke E, Maes M, Victor J, Verdonk P, et al. (2013) Anatomy of the anterolateral ligament of the knee. Journal of Anat 223(4): 321-328.
- Vincent, JP, Magnussen RA, Gezmez F, Uguen A, Jacobi M, et al. (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthro 20(1): 147-152.
- Monaco E, Ferretti A, Labianca L, Maestri B, Speranza A, et al. (2012) Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc 20(5): 870-877.
- Ségond P (1879) Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Prog Med 7: 297-9, 319-21, 40-1.
- Terry GC, Hughston JC, Norwood LA (1986) The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med 14(1): 39-45.
- La Prade RF, Gilbert TJ, Bollom TS, Wentorf F, Chaljub G, et al. (2000) The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am J Sports Med 28(2): 191-199.
- Campos JC, Chung CB, Lektrakul N, Pedowitz R, Trudell D, et al. (2001) Pathogenesis of the Segond Fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 219(2): 381-386.
- Lemaire M (1967) Ruptures anciennes du ligament croise anterieur du genou. J Chir 311-320.
- Macintosh D, Darby T (1976) Lateral substitution reconstruction. In: Proceedings of the Canadian Orthopaedic Association. J Bone Joint Surg Br 58(1): 142.
- Losee RE, Johnson TR, Southwick WO (1978) Anterior subluxation of the lateral tibial plateau. A diagnostic test and operative repair. J Bone Joint Surg Am 60(8):1015-1030.
- Arnold JA, Coker TP, Heaton LM, Park JP, Harris WD (1979) Natural history of anterior cruciate tears. Am J Sports Med 7: 305-313.
- Ellison AE (1979) Distal iliotibial-band transfer for anterolateral rotatory instability of the knee. J Bone Joint Surg Am 61(3): 330-307.
- Benum P (1982) Anterolateral rotary instability of the knee joint. Results after stabilization by extraarticular transposition of the lateral part of the patellar ligament. A preliminary report Acta Orthop Scand 53(4): 613-617.
- Andrews JR, Sanders R (1983) A “mini-reconstruction” technique in treating anterolateral rotatory instability (ALRI). Clin Orthop Relat Res 172: 93-96.
- Muller W (1983) The Knee Form, Function, and Ligament Reconstruction New York, Springer Verlag, pp. 253-257.
- Wilson WJ, Scranton PE Jr (1990) Combined reconstruction of the anterior cruciate ligament in competitive athletes. Bone Joint Surg Am 72(5): 742-748.
- Marshall JL, Warren RF, Wickiewicz TL, Reider B (1979) The anterior cruciate ligament: a technique of repair and reconstruction. Clin Orthop Relat Res 143: 97-106.
- Bertoia JT, Urovitz EP, Richards RR, Gross AE (1985) Anterior cruciate reconstruction using the MacIntosh lateral-substitution over-the-top repair. J Bone Joint Surg Am 67: 1183-1188.
- Zarins B, Rowe CR (1986) Combined anterior cruciate-ligament reconstruction using semitendinosus tendon and iliotibial tract. J Bone Joint Surg Am 68(2): 160-177.
- Lerat JL, Duprã La Tour L, Herzberg G, et al. (1987) Review of 100 patients operated on for chronic anterior laxity of the knee by a procedure derived from the Jones and MacIntosh methods. Value of dynamic radiography for the objective analysis of the results. Rev Chir Orthop Reparatrice Appar Mot 73(Suppl 2): 201-204.
- Ekstrand J (1989) Reconstruction of the anterior cruciate ligament in athletes, using a fascia lata graft: a review with preliminary results of a new concept. Int J Sports Med 10(4): 225-232.
- Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, et al. (1998) Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 6(2): 68-75.
- Colombet PD (2011) Navigated intra-articular ACL reconstruction with additional extraarticular tenodesis using the same hamstring graft. Knee Surg Sports Traumatol Arthrosc 19(3): 384-389.
- Duthon VB, Magnussen RA, Servien E, Neyret P (2015) ACL reconstruction and extra-articular tenodesis. Clin Sports Med 32: 141-153.
- Smith JO, Yasen SK, Lord B, Lord B, Wilson AJ (2015) Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surg Sports Traumatol Arthrosc 23(11): 3151–3156.
- Helito CP, Bonadio MB, Gobbi RG, Da Mota E Albuquerque RF1, Pécora JR, et al. (2015) Combined intra- and extra-articular reconstruction of the anterior cruciate ligament: the reconstruction of the knee anterolateral ligament. Arthrosc Tech 4(3): 239-244.
- Sonnery-Cottet B, Daggett M, Helito CP, Thaunat M, Fayard JM, et al. (2016) Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction. Arthrosc Tech 5(6): e1253-e1259.
- Wagih AM, Elguindy AM (2016) Percutaneous Reconstruction of the Anterolateral Ligament of the Knee with a Polyester Tape. Arthrosc Tech 5(4): 691-697.
-
Sebastian Orduna, Nagib Atallah Yordi. Lateral Extraarticular Tenodesis in Combination with ACL Reconstruction: Indications, Technique Description. Glob J Ortho Res. 1(4): 2019. GJOR.MS.ID.000520.
-
Anterior cruciate ligament, ACL reconstruction, ACL-deficient, Anterior laxity, Rotational laxity, Inter-related tunnels, Anterolateral ligament, Indications, Contraindication, Tenodesis, Iliotibial band, Lateral capsular ligament
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






