 Research Article
Research Article
Impact of Falls from Occupational Injuries: A Comparative Analysis of Mortality and Disability Across Sociodemographic Index 2010 to 2019
Christine Vella1* and J Zammit Meampel2
1Surgical trainee, Malta
2Orthopaedic and Trauma Surgeon Consultant, Malta
Corresponding AuthorChristine Vella, Surgical trainee, Malta
Received Date: August 08, 2024; Published Date: October 01, 2024
Abstract
This study investigates the impact of falls from occupational injuries on disability, focusing on a comparative analysis across different Socio- Demographic Index (SDI) categories from 2010 to 2019 using data from the GBD database. The primary aim is to identify trends, disparities, and contributing factors to the rate of Years Lived with Disability (YLD) resulting from occupational falls. A retrospective cross-sectional observational design was employed, analyzing data from various global regions categorized by high, middle, and low SDI. The results indicate a significant disparity in disability outcomes related to occupational falls across SDI categories. Lower SDI groups consistently showed higher rates of YLD, suggesting an increased burden and a lack of sufficient occupational health policies and safety measures in these regions. The regression analysis revealed a statistically significant relationship between SDI groups and the rate of YLD (p-value = 0.004), while the relationship between year and the rate of YLD was not statistically significant (p-value = 0.197).
These findings are crucial for informing policies and interventions to reduce occupational falls. The study highlights the need to enhance safety standards, especially in low SDI areas, and suggests that global health policies prioritize tailored interventions for different sociodemographic groups. Understanding these disparities and contributing factors provides evidence-based insights to help mitigate the impact of occupational injuries on worker health and well-being.
Introduction
Falls from occupational injuries constitute a significant and persistent threat of morbidity and mortality within various demographic groups. The incidence, mortality, and disability resulting from these incidents are influenced by factors including age, gender, socioeconomic status, and geographical location, affecting individuals across all age groups. Despite their preventable nature, falls continue to pose substantial risks in modern healthcare settings, necessitating the implementation of safety measures and interventions [1]. In younger populations, falls can result in severe disabilities such as traumatic brain injuries or spinal cord injuries, while older adults may experience heightened morbidity due to comorbid conditions such as osteoporosis or medication usage [2]. Surprisingly, falls often remain overlooked as a global issue, despite their ranking as a leading cause of disability-adjusted life years and unintentional injury-related deaths[3].
In the Global Burden of Diseases, Injuries, and Risk Factors Study 2017 (GBD 2017), falls emerged as a significant contributor to the burden of disease, ranking among the top causes of disabilityadjusted life years and unintentional injury-related deaths [4].
Beyond the personal toll, these falls are also economically costly, with implications for healthcare expenditure, loss of productivity, and long-term disability costs. According to the National Institute of Safety and Health at Work (INSST) in Europe, the economic burden of occupational falls reaches upwards of 476 billion euro. The Health and Safety Executive (HSE) has calculated that workrelated injuries and illnesses in the United Kingdom amount to £14 billion, approximately 1% of the GDP [5]. The International Labour Organization (ILO) reports that approximately 2.3 million individuals globally die each year from work-related accidents or diseases, which equates to more than 6000 deaths daily. Additionally, there are about 340 million occupational accidents and 160 million cases of work-related illnesses worldwide every year [6].
While existing research on falls has predominantly focused on older populations, it is imperative to understand their impact across all age groups and demographics. The World Health Organisation reports that falls are a leading cause of injury-related deaths among those aged 65 and older, emphasising the need for comprehensive studies to assess the distribution of falls-related morbidity and mortality [3]. The GBD Study serves as a vital resource for analysing the global burden of falls, offering comprehensive estimates of mortality, non-fatal health outcomes, and risk factors across various demographics and regions. However, to date, there has been limited examination of falls specifically within the occupational setting. In this study, the GBD 2017 framework was used to investigate the impact of falls from occupational injuries on mortality and disability, conducting a comparative analysis across sociodemographic indices from 2010 to 2019 [7].
While occupational falls are well-documented as major causes of morbidity, mortality, and economic burdens, research on variations across countries of differing economic statuses is sparse.
Most studies focus on general data, not on how socioeconomic factors distinctly influence outcomes in different regions. This gap underscores the need for this study, which analyses variations across countries with different SDI levels. This research extends existing literature and provides crucial insights for more tailored and effective global workplace safety interventions. The primary aim of this dissertation was to conduct a comparative analysis of mortality and disability following falls from occupational injuries across sociodemographic indices. Specifically, the study seeks to quantify trends, identify disparities, and elucidate the factors contributing to differential outcomes [8].
Methods
A retrospective cross-sectional observational design was adopted, utilizing data from the GBD database from 2010 to 2019. This approach facilitated the analysis of trends and patterns in fallsrelated mortality and disability across different sociodemographic indices globally, categorizing data into high, middle, and low SDI groups. The GBD 2019 study provides comprehensive estimates for incidence, prevalence, mortality, and Years Lived with Disability (YLDs) for 369 diseases and injuries across 204 nations. The study uses diverse data sources, including population censuses, household surveys, civil registration systems, disease registries, health service data, and air pollution monitors. YLDs are estimated by combining prevalence figures with disability weights specific to each condition [9-11]. Data were extracted using structured injury risk codes from the GBD 2019 study, focusing specifically on occupational injuries due to falls. The data selection process involved choosing ‘Deaths’ and ‘YLDs’ from the ‘Measure’ category, refining metrics to ‘Number’ and ‘Rate’, and setting ‘Occupational Injuries’ as the risk parameter.
Data were further categorized by SDI levels (low, middle, high) and covered the years 2010-2019. Rates were calculated per 100,000 individuals. The study included data on all age groups and both sexes across all SDI categories. Exclusion criteria were set to omit data unrelated to occupational injuries and falls, including non-occupational injuries, other types of workplace accidents, and records with incomplete sociodemographic information or unverifiable outcomes. This ensured a focused and reliable analysis over the 10-year period. The analysis was stratified by SDI, which is calculated using income per capita, average educational completion over age 15, and total fertility rate under age 25. This index spans from 0 (lowest development levels) to 1 (highest development levels), providing a comprehensive assessment of development across regions. Primary variables included the number of deaths and YLDs attributable to occupational falls [12,13].
To minimize bias, a standardized protocol for data extraction and analysis was employed, with cross-referencing for accuracy. The GBD’s methodology ensures comparability across countries and time, accounting for variations in data quality and availability [14]. Descriptive statistics provided an overview of mortality and disability trends. Time-series analysis identified changes and trends over the specified period. Data analysis was conducted using IBM SPSS Statistics software (version 29.0.2.0) [15]. A scatter plot illustrated the rate of death by year for High, Medium, and Low SDI groups, including a linear regression line to indicate overall trends. The p-value assessed the statistical significance of these relationships [16].
Results
The scatter plot (Figure 1) illustrates the rate of death by year for three SDI groups (High, Medium, Low) from 2010 to 2019 (Table 1). The High SDI group consistently exhibits the lowest mortality rates across all years, with data points clustered near the bottom of the plot, indicating stable and low rates of death. The Medium SDI group shows higher mortality rates, with data points scattered near the top of the plot, suggesting slight variability but consistently higher rates compared to the High SDI group. The Low SDI group displays a declining trend in mortality rates over the observed period, with data points gradually decreasing from higher to lower positions on the plot.
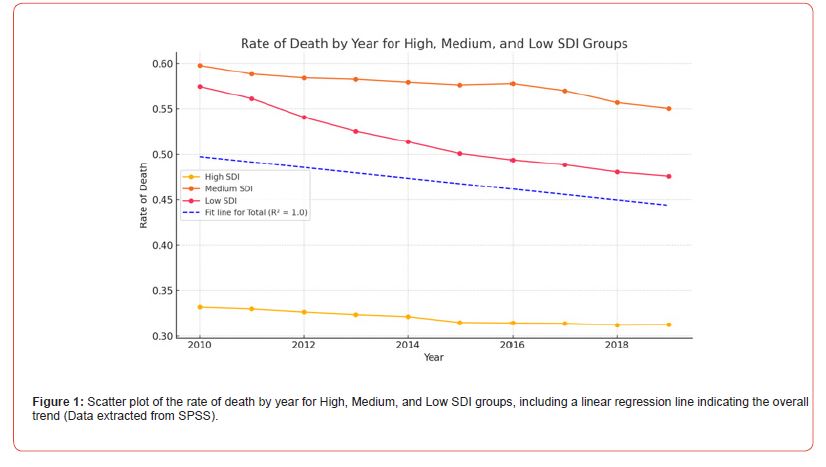
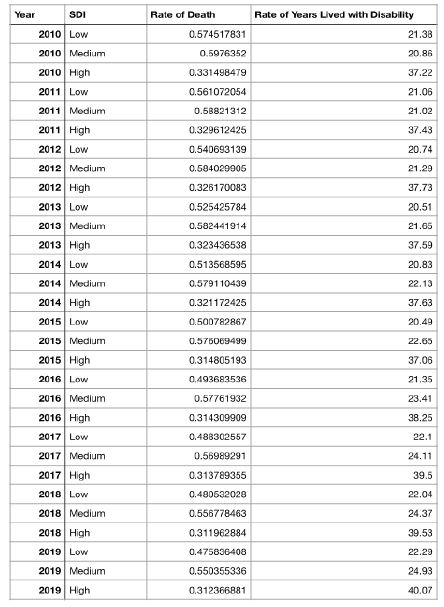
Table 1: Rate of Death and Years Lived with Disability by Socio-Demographic Index (SDI) from 2010 to 2019.
-->
The linear regression line, which fits the overall data, shows a slight negative slope, indicating a general decrease in the rate of death from 2010 to 2019. However, the R-squared value of 0.024 suggests that the year explains only 2.4% of the variance in the rate of death, indicating that the year alone is not a strong predictor of mortality rate changes across the SDI groups. The p-value for the Year variable was 0.218, indicating no statistical significance at the 95% confidence level. However, the p-value for the SDI Group variable was less than 0.001, indicating a statistically significant relationship between SDI groups and the rate of death at the 95% confidence level. This significant p-value suggests that changes in SDI groups are associated with significant changes in the rate of death.
The scatter plot (Figure 2) presents the rate of YLD by year for three SDI groups (High, Medium, Low) from 2010 to 2020. Each data point represents the rate of YLD for a specific SDI group in a given year. The High SDI group consistently shows the lowest rates, with data points clustered near the bottom of the plot, indicating stable and low disability rates across the years. The Medium SDI group exhibits the highest rates, with data points consistently near the top of the plot. The Low SDI group shows varying rates but generally falls between the High and Medium SDI groups. A linear regression analysis was conducted to determine the relationship between SDI groups, year, and the rate of years lived with disability. The p-value for the Year variable was 0.197, indicating no statistical significance at the 95% confidence level. However, the p-value for the SDI Group variable was 0.004, indicating a statistically significant relationship between SDI groups and the rate of YLD at the 95% confidence level. This significant p-value suggests that changes in SDI groups are associated with significant changes in the rate of years lived with disability.
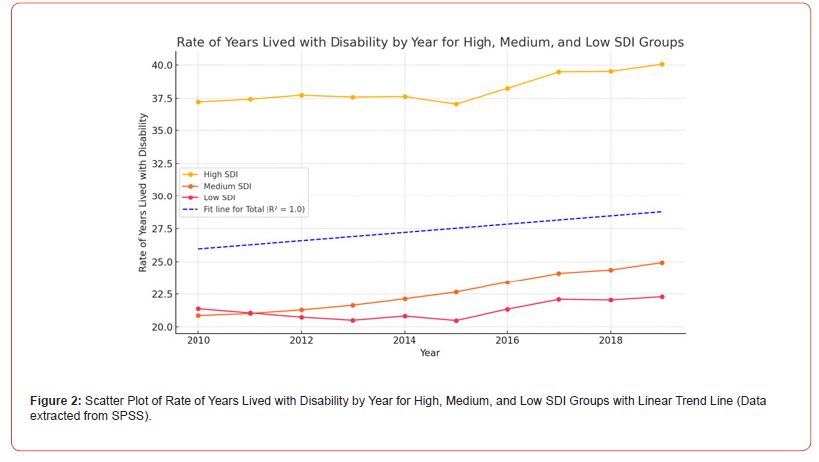
The regression line in Figure 2, fitted to the overall data, shows a slight positive slope, indicating a general increase in the rate of years lived with disability from 2010 to 2020. However, the R-squared value of 0.013 suggests that the year explains only 1.3% of the variance in the rate of YLD, indicating that the year alone is not a strong predictor of disability rate changes across the SDI groups. Despite this, the significant relationship between SDI groups and the rate of YLD emphasises the importance of sociodemographic factors in understanding health outcomes.
Discussion
This dissertation has comprehensively examined the epidemiology of occupational falls across groups of varying sociodemographic indices, utilising a decade of data from the Global Burden of Disease study. Through this analysis, the research has illuminated significant trends and disparities in the incidence and consequences of occupational falls, offering a detailed understanding of their global impact. Contrary to expectations, high SDI countries exhibit higher reported death and morbidity rates. Enhanced reporting systems and health surveillance in regions with high SDI were observed to potentially lead to a more precise collection of data regarding non-fatal injuries. The improvement in diagnostic capabilities, coupled with a stronger focus on the systematic recording and monitoring of occupational injuries, was noted to contribute to an increase in the documented cases of morbidity. The comprehensive availability of such detailed records might also facilitate greater recognition and classification of chronic health conditions as being related to occupational environments.
This shift towards more thorough documentation and classification practices is likely to have a significant impact on the understanding of the scope and scale of occupational health issues within these high SDI region [17,18]. Such developments are critical for providing a clearer picture of occupational health trends and for formulating more effective workplace health policies and interventions. These observations underscore the importance of continuous improvements in health surveillance systems to enhance the accuracy and comprehensiveness of occupational health data.
In this study, higher rates of morbidity were notably observed in regions with middle and high SDI levels. Individuals in higher socioeconomic groups often have better access to healthcare and legal resources, enabling them to report injuries more frequently and pursue compensation claims effectively, leading to more robust data on occupational injuries [19]. Studies have shown that workers’ compensation claims are substantially more common in developed countries, where regulatory frameworks and healthcare systems are more advanced [20]. This enhanced infrastructure not only supports better documentation of occupational injuries but also improves survival rates from severe injuries, although often with significant disabilities. However, this framework does not fully explain the high morbidity rates in middle SDI countries, suggesting the presence of additional factors affecting these outcomes, which require further exploration to understand the complex dynamics at play [21].
Results may be influenced by the ‘healthy worker’ effect. This suggests that the working population generally appears healthier than the general population [22]. The effect arises because seriously ill or disabled individuals are less likely to be employed. Improved healthcare has enabled more individuals with disabilities to work, potentially increasing recorded YLDs in occupational settings. This study focuses on individuals who returned to work after a disability, excluding those who couldn’t return and lived with the disability outside the workforce. Therefore, while the healthy worker effect might suggest an underestimation of disabilities within the employed population, this analysis does not encompass those who have left the workforce permanently. This limitation means the data might underestimate disabilities in the employed population. Policymakers must consider this when interpreting occupational health data and planning interventions to support disabled workers [23-26].
The categorisation of countries into different SDI groups is useful for broad comparisons but may mask important variations within these groups. These intra-group differences can provide critical insights into occupational health outcomes. Generalising SDI categories without recognising these differences may limit the ability to fully understand and address specific occupational health challenges within similar economic contexts. While SDI offers a valuable framework for analysis, it also introduces complexity in data interpretation. Additionally, the 2018 annual report by the ILO reinforced these findings, pointing out that in regions with low SDI, informal workers, who are frequently omitted from traditional occupational health surveillance systems encounter substantially higher risks. These workers, often engaged in unregulated sectors, lack formal employment protections and access to health and safety resources, placing them at increased vulnerability to occupational injuries [27].
This lack of inclusion in safety programs and health monitoring means that the actual rate of injuries in these populations may be underreported, and the severity of occupational health issues underestimated. The findings from the ILO report underline the critical need for tailored interventions that address the unique challenges faced by workers in low SDI regions. Enhanced safety measures, better regulatory oversight, and increased training opportunities are essential to mitigate the disparities in occupational health outcomes observed across different regional and economic contexts [28].
The longitudinal dynamics of occupational injuries, as analysed by Baidwan, NK et al. (2018), indicate that improvements in a country’s SDI generally correlate with a reduction in the rate of severe occupational injuries, though the relationship is not linear [29]. The study highlights that as countries transition from low to middle SDI, often spurred by industrialisation, there is an initial surge in occupational injury risks. This increase can be attributed to rapid workforce changes and industrial practices that outpace the development of safety regulations and worker training. During these transitional phases, emerging industries may not yet have adequate safety protocols in place, and the enforcement of existing standards can be inconsistent or insufficient, thereby elevating the risk of injuries. This dynamic could explain the higher rates of YLD and mortality observed in the middle SDI group. Another contributing factor might be the middle SDI countries’ intermediate capacity in health documentation and reporting.
These countries likely possess better resources to record and report injuries and mortality compared to low SDI countries but may lack the more advanced medical infrastructure of high SDI countries to effectively treat injuries. This intermediate capability might paradoxically result in higher observed rates of mortality and morbidity than seen in both high and low SDI groups, highlighting a complex interplay between healthcare development and injury outcomes in middle SDI countries [30]. Future research should focus on reducing the burden of falls from occupational injuries and improving workplace safety. Longitudinal studies are needed to understand the long-term effects of occupational falls, including chronic health conditions, disability, and quality of life impacts. These studies will offer insights into the progression and management of fall-related conditions [31]. Developing and implementing preventive strategies is crucial. Enhancing engineering controls, strengthening administrative protocols, and promoting personal protective equipment can significantly reduce fall risks.
Targeted interventions for high-risk industries and vulnerable groups, such as older workers or those in hazardous conditions, are essential for improving occupational health outcomes. Increased investment in educational and training programs is also needed to raise awareness of fall hazards and encourage safe practices. Empowering workers with knowledge and tools to address risks proactively will enhance their safety and well-being [32]. Addressing these research priorities and implementing effective strategies can reduce the frequency and severity of occupational falls, creating safer work environments globally. This research aims to contribute to the body of knowledge in occupational health by providing evidence-based insights into the impact of falls on worker health. The findings are expected to inform policy decisions and interventions to improve workplace safety and reduce the burden of falls [7].
Limitations
This study has limitations, primarily relying on data from the GBD study. While comprehensive, GBD data’s accuracy varies by country. High-income countries often have better health data systems than low-income ones, potentially leading to overrepresentation of certain health outcomes. Reporting and classification methods for occupational injuries differ by region and over time, introducing bias that could affect trends and skew results. There may be delays in GBD data reporting, meaning it might not reflect the most current trends or intervention impacts. Despite these issues, the GBD study is a robust, widely used dataset with a systematic approach to quantifying global health burdens. It is trusted and cited in high-profile studies, including articles in The Lancet and The New England Journal of Medicine, underscoring its critical role in global health research and policy [33-35].
Conclusion
This study assessed the impact of occupational falls on disability across different SDI categories using GBD data from 2010 to 2019. The findings show that lower SDI regions consistently have higher YLD rates due to occupational falls. Regression analysis confirmed a significant relationship between SDI groups and YLD rates, highlighting the role of socio-demographic factors in disability outcomes. These results align with existing literature on the vulnerability of lower-income regions to occupational injuries due to poor safety measures and healthcare access. The study calls for targeted interventions, improved safety standards, and enhanced health surveillance to address these disparities, advocating for global policy reforms and increased investment in occupational health to improve worker well-being.
References
- Najafpour Z, Godarzi Z, Arab M, Yaseri M (2019) Risk Factors for Falls in Hospital In-Patients: A Prospective Nested Case Control Study. Int J Health Policy Manag 8(5): 300-306.
- Rapp K, Rothenbacher D, Magaziner J, Becker C, Benzinger P, et al. (2015) Risk of Nursing Home Admission After Femoral Fracture Compared with Stroke, Myocardial Infarction, and Pneumonia. J Am Med Dir Assoc 16(8): 715.e7-715.e12.
- Vaishya R, Vaish A (2020) Falls in Older Adults are Serious. Indian J Orthop 54(1): 69-74.
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159): 1789-1858.
- Tompa E, Mofidi A, van den Heuvel S, van Bree T, Michaelsen F, et al. (2021) Economic burden of work injuries and diseases: a framework and application in five European Union countries. BMC Public Health 21(1): 49.
- Takala J, Hämäläinen P, Sauni R, Nygård CH, Gagliardi D, et al. (2024) Global-, regional- and country-level estimates of the work-related burden of diseases and accidents in 2019. Scand J Work Environ Health 50(2): 73-82.
- GBD 2019 Risk Factors Collaborators. (2020) Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258): 1223-1249.
- Busey A, Asfaw A, Applebaum KM, O’Leary PK, Tripodis Y, et al. (2021) Mortality following workplace injury: Quantitative bias analysis. Ann Epidemiol 64: 155-160.
- Peden AE, Cullen P, Francis KL, Moeller H, Peden MM, et al. (2022) Adolescent transport and unintentional injuries: a systematic analysis using the Global Burden of Disease Study 2019. Lancet Public Health 7(8): e657-e669.
- Safiri S, Karamzad N, Kaufman JS, Bell AW, Nejadghaderi SA, et al. Prevalence, Deaths and Disability-Adjusted-Life-Years (DALYs) Due to Type 2 Diabetes and Its Attributable Risk Factors in 204 Countries and Territories, 1990-2019: Results From the Global Burden of Disease Study 2019. Front Endocrinol (Lausanne). 2022 13: 838027.
- James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, et al. (2020) The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev 26(Supp 1): i3–i11.
- Go DS, Kim YE, Yoon SJ (2020) Subnational Burden of Disease According to the Sociodemographic Index in South Korea. Int J Environ Res Public Health 17(16): 5788.
- Zhang YJ, Kong XM, Lv JJ, Yang CH, Li XY, et al. (2023) Analysis of the global burden of disease study highlights the global, regional, and national trends of idiopathic epilepsy epidemiology from 1990 to 2019. Prev Med Rep 36: 102522.
- Global Burden of Disease methodology. In: World Report on Disability 2011. World Health Organization.
- Thurber KA, Thandrayen J, Maddox R, Barrett EM, Walker J, et al. (2022) Reflection on modern methods: statistical, policy and ethical implications of using age-standardized health indicators to quantify inequities. Int J Epidemiol 51(1): 324-333.
- Tenny S, Abdelgawad I (2024) Statistical Significance. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
- Improvement of national reporting, data collection and analysis of occupational accidents and diseases.
- The Global Burden of Disease: Generating Evidence, Guiding Policy | Institute for Health Metrics and Evaluation.
- National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Flaubert JL, Le Menestrel S, Williams DR, Wakefield MK, editors. Washington (DC): National Academies Press (US).
- Di Donato M, Sheehan LR, Gray S, Iles R, van Vreden C, et al. (2023) Development and initial application of a harmonised multi-jurisdiction work injury compensation database. Digit Health 9: 20552076231176695.
- Molassiotis A, Kwok SWH, Leung AYM, Tyrovolas S (2022) Associations between sociodemographic factors, health spending, disease burden, and life expectancy of older adults (70 + years old) in 22 countries in the Western Pacific Region, 1995–2019: estimates from the Global Burden of Disease (GBD) Study 2019. GeroScience 44(2): 925-951.
- Chowdhury R, Shah D, Payal AR (2017) Healthy Worker Effect Phenomenon: Revisited with Emphasis on Statistical Methods – A Review. Indian J Occup Environ Med 21(1): 2-8.
- Thygesen LC, Hvidtfeldt UA, Mikkelsen S, Brønnum-Hansen H (2011) Quantification of the healthy worker effect: a nationwide cohort study among electricians in Denmark. BMC Public Health 11(1): 571.
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159): 1789-858.
- Lyons RA, Kendrick D, Towner EM, Christie N, Macey S, et al. (2011) Measuring the Population Burden of Injuries-Implications for Global and National Estimates: A Multi-centre Prospective UK Longitudinal Study. PLoS Med 8(12): e1001140.
- Bhalla K, Harrison JE, Shahraz S, Fingerhut LA (2010) Global Burden of Disease Injury Expert Group (2010) Availability and quality of cause-of-death data for estimating the global burden of injuries. Bull World Health Organ 88(11): 831-838C.
- Rantanen J, Muchiri F, Lehtinen S (2020) Decent Work, ILO’s Response to the Globalization of Working Life: Basic Concepts and Global Implementation with Special Reference to Occupational Health. Int J Environ Res Public Health 17(10): 3351.
- Flynn MA (2014) Safety & the Diverse Workforce. 59(6): 52-57.
- Baidwan NK, Gerberich SG, Kim H, Ryan AD, Church TR (2018) A longitudinal study of work-related injuries: comparisons of health and work-related consequences between injured and uninjured aging United States adults. Inj Epidemiol 5(1): 35.
- Haagsma JA, James SL, Castle CD, Dingels ZV, Fox JT, et al. (2020) Burden of injury along the development spectrum: associations between the Socio-demographic Index and disability-adjusted life year estimates from the Global Burden of Disease Study 2017. Inj Prev 26(Supp 1): i12-i26.
- HSIAO H (2014) Fall Prevention Research and Practice: A Total Worker Safety Approach. Ind Health 2014 52(5): 381-392.
- Organization WH, Burton J (2010) WHO healthy workplace framework and model: background and supporting literature and practices. World Health Organization.
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859): 2095-2128.
- Li Y, Li H, Jiang Y (2023) Analysis of the burden and trends of communicable diseases in Pacific Island countries from 1990 to 2019. BMC Public Health 23(1): 2064.
- GBD 2021 Demographics Collaborators (2024) Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950-2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440): 1989-2056.
-
Christine Vella* and J Zammit Meampel. Impact of Falls from Occupational Injuries: A Comparative Analysis of Mortality and Disability Across Sociodemographic Index 2010 to 2019. Glob J Ortho Res. 4(5): 2024. GJOR.MS.ID.000598.
-
Osteogenesis imperfecta, non-telescoping rods, Fracture risk reduction, Recurrent fractures, Osteogenesis Imperfecta, Elastic Stable Intramedullary Nail
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






