 Research Article
Research Article
Page 1 of 7 Screwed Plate Osteosynthesis (SPO) for Pediatric Femur Fractures: A Report of 15 Cases
Aloise Sagna1*, Ndeye Fatou Seck2, Ibrahima Bocar Welle3, Ibrahima Fall4
1Department of paediatric surgery of Albert Royer’s children national university hospital in Dakar
2Pediatric surgeon at Albert Royer’s children national university hospital in Dakar
3Pediatric surgeon at Albert Royer’s children national university hospital in Dakar
4Department paediatric of surgery of Albert Royer’s children national university hospital in Dakar
Corresponding AuthorAloise Sagna, Cheikh Anta Diop University Faculty of Medicine Pharmacy and Dentistry, Senegal.
Received Date:June 06, 2023; Published Date:September 11, 2023
Abstract
Background: The management of femur fractures in children is made complex by the wide variety of surgical procedures. Although Elastic Stable
Intramedullary Nailing (ESIN) is the leading surgical indication in children, Screwed Plate Osteosynthesis (SPO) appears as a definite alternative
with better results in some cases. The purpose of this work is to present our prospective short study of SPO in pediatric femur shaft fractures
and highlight the need in older children to embrace innovative new approach of minimally invasive plate osteosynthesis (MIPO) in a Senegalese
children’s hospital. Results: All the patients were between 7 and 15 years with an average of 11 years old. This was a short continuous series of 15
patients, 13 males and 2 females, with a sex ratio of 6.5. The mechanism of fracture was mainly direct impact force following a high-energy trauma.
Most of the fractures involved the dominant limb (66.6%), and line fractures most often located in the middle third of the shaft, that is 10 children.
The procedure had been performed open in all cases using a locking compression plate (LCP) with an average of 6 to 8 holes. Walking with a pair of
canes and without either unilateral step support or physiotherapy was prescribed in early postoperative period. Two cases of superficial surgical
wound suppuration which responded well under antibiotic therapy and directed healing, as well as a limb shortening of 1 cm in the long run followup,
were noted. It was radiologically found a mean time consolidation of 60 days (extremes 45 and 90 days). According to the FLYNN criteria and
after a mean follow-up of 24 months, thirteen patients had good results while three ones got a medium score. Our study had shown that classic SPO
could achieve good performance with minor post-operative complication controlled.
Conclusion: Authors believe that migration to minimally invasive approach with new less invasive stabilization system (LISS) ancillaries and
luminance amplifier would certainly bring the benefit of closed defect with most excellent outcomes compared to the ESIN.
Keywords:Pediatric femur shaft; Fracture osteosynthesis; screwed plate; minimally invasive surgery
Abbreviations:SPO-Screwed plate osteosynthesis; ESIN: Elastic stable intramedullary Nailing; AO: Association of osteosynthesis; LCP: Locking compression plate; AAOS: American academy of orthopedic surgeons; PSW-Plate span width; MIPO: Minimally invasive plate osteosynthesis
Background
The management of pediatric femur fractures is made complex by the wide variety of surgical procedures. Although Elastic Stable Intramedullary Nailing (ESIN) is the leading surgical indication in older children, SPO appears as a definite alternative with better results in some cases [1,2]. The purpose of our study is to present the contribution of SPO in the context of pediatric surgery in west Africa.
Methods
We included all femur shaft’s fractures treated with SPO at the Pediatric Surgery Department of the Albert ROYER Children’s Hospital during the study period. Our work excluded fractures with underlying bone pathology, and patients with incomplete or unrecovered records. Children who were lost from view or did not have regular follow-up with post-operative assessment were not included, that was three cases. This is a preliminary, prospective, descriptive, and analytical monocentric study over 3 years. It involved a series of femur fractures in 15 patients operated at a tertiary children’s hospital in Dakar between January 1, 24 2014, and December 31, 2016. The study protocol included a first step of data collected from patients’ records, and consultation registers. The second step was surgical technique performed under general anesthesia with Child placed in supine or lateral position on ordinary or orthopedic table. The limb was draped free from the iliac crest to the foot. A longitudinal lateral incision centered on the fracture site was performed through the skin and the Tensor Fascia Lata muscle. A deep non-bleeding dissection released Vastus Lateralis muscle line insertion on the femoral crest. Fracture reduction was obtained either by traction on orthopedic table in case of supine position, or by manual traction knee bent at 90 degrees in lateral position. Conventional 3.5 mm or 4.5 mm broad AO pediatric compression plates (LCP) were used in all cases. As a rule, the plate length should allow the insertion of at least two screws on both sides of fracture site. Postoperative plaster immobilization of limb was indicated only in case of delicate primary stability of devices. A pair of canes was prescribed the next day by a physiotherapist who taught how to walk with. The patient should start walking without the support of an operated limb and move progressively toward weight-bearing ambulation. The quantitative variables listed were presented as averages, while qualitative ones were assessed as percentages. The circumstances of accident were classified as lowenergy trauma such a common fall, and a high-energy trauma when related to traffic accident, a fall from a high height or sport accident. Postoperative complications were listed in blood loss, surgical site infection, parietal infection, and general infection; the overall evolution of the fracture was evaluated according to FLYNN criteria (Table I). Data analysis allowed us to make statistical correlations using on the one hand COX model, and the BRAVAIS-PEARSON test with a significant link when the coefficient tends towards 1, on the other one (Table 1).
Table 1:Assessment for complications according to Flynn’s Criteria [31].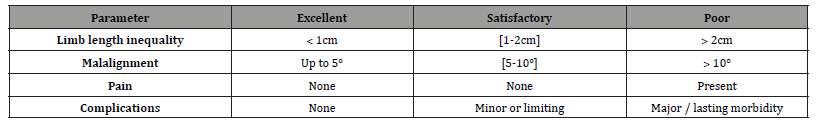
Results
Fifteen patients with sixteen closed femoral shaft fractures were treated with SPO. There were thirteen males and two females, with an average age of 11 years (range, 7-15 years). The figure 1 shows the age distribution with a sex-ratio of 6.5. Eighteen of these injuries were caused by a high-energy trauma, and the mechanism was direct in 80% (Table 2).
Table 2:Distribution of patients according to the accident type.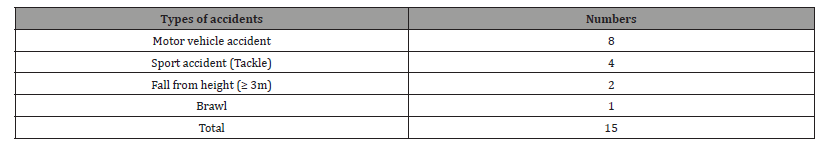
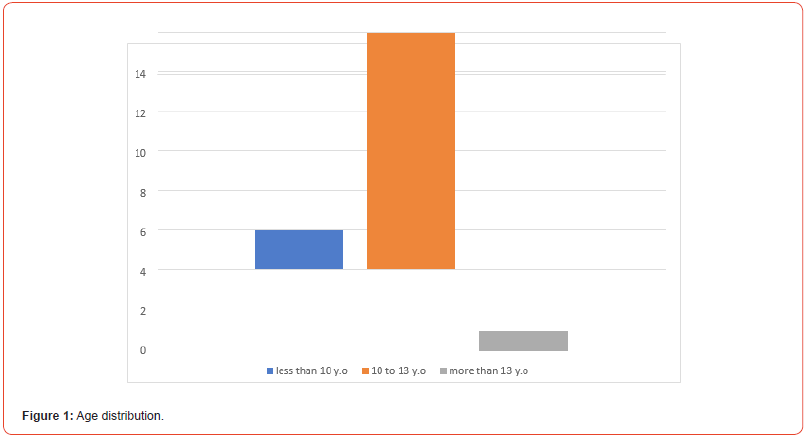
Nine patients were seen within twenty-four hours following the trauma, with dominant limb and middle femur shaft involved in 10 cases. A limb shortening and complete functional disability was found in thirteen patients, with foot external rotation in 4 cases. Swelling, with thigh deformation were noted in seven children. Associated skeletal injuries were recorded in five cases, which included 2 head traumas, 1 fracture of both forearm bones, 1 isolated fibula fracture, and 1 iliac wing fracture. Dermabrasion of the skin or superficial wounds were recorded in two patients. There was one case of subdural hematoma as revealed by C-T Scan performed in the children with associated head trauma. Pubic symphysis disjunction was highlighted by ultrasound in the patient with associated iliac wing fracture. Two of our patients had hemoglobin levels below 10g/dl, which required blood transfusion prior to surgery. Antibiotic therapy was introduced during pre, per and postoperative periods in polytrauma patients with bladder burst, followed by pyuria, leukocytosis, and high level of C- reactive protein. Sixteen conventional LCP plates were performed in 15 children; surgery was preceded by limb traction using Elastoplast tape method, in seven patients. The procedure was performed on an orthopedic table in 9 cases, and fracture reduction was obtained by manual traction on an ordinary table in six patients. Surgical approach was made through a lateral incision of different length (range: 4cm – 10cm, mean: 8cm) The plates used were distributed according to the number of holes (Table III). We used on average three on either side of the fracture, that was 6 with extremes of 4 and 10 screws (Table 3) (Figure 1&2).
Table 3:Plates’ distribution according to the numbers of holes.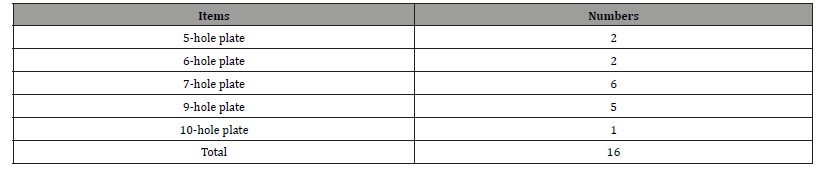
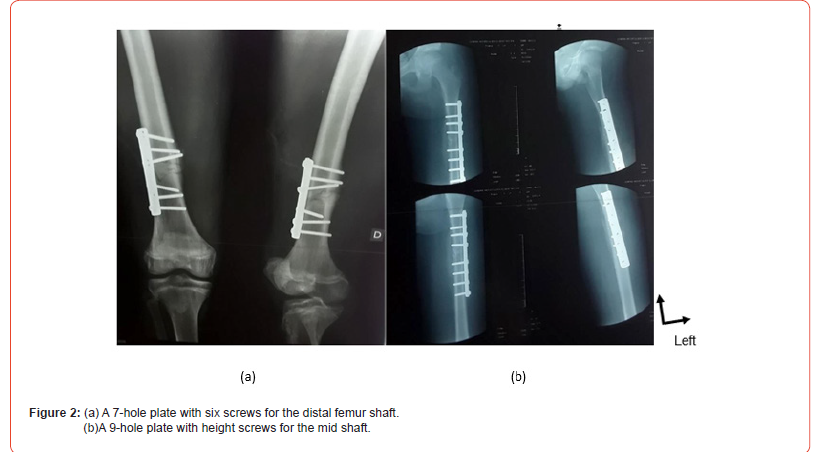
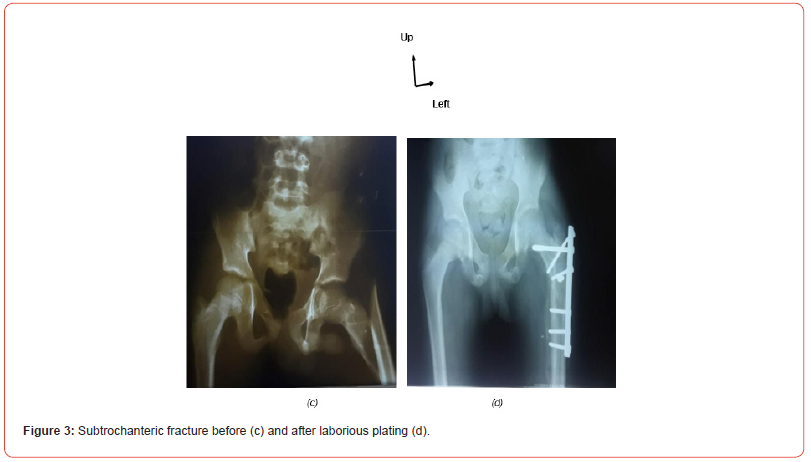
After a postoperative mean follow up of 24 months (extremes: 5-60 months), we recorded, according to the FLYNN criteria, 13 good results and 3 intermediate ones. The average time of radiological consolidation was 60 days with (extremes: 45-90 days). Postoperative immediate surgical follow-up was simple except in two boys (7 and 14-year-old), traffic victims with superficial parietal wound suppuration healed by prolonged antibiotic therapy within10 days. One child developed a centimeter limb shortening following a subtrochanteric fracture with laborious and precarious osteosynthesis plan completed by a postoperative cruropedic cast (Figure 3). Walk recovery with two crutches was effective on day one after surgery. The resumption of everyday life activities was spontaneous without any physiotherapy sessions in all cases as soon as the pain disappeared. We did not report any early postoperative complications such as acute or chronic anemia; neither did note any joint stiffness of the knee or hip (Figure 3).
The study registered a lack of significant correlation (p = 0.0012) between bone consolidation time and the length of the plate. There was, however, a strong link between healing time and patient age, with radiological bone callus occurring much faster than the child is young (p =0.973). The multivariate statistical analysis of the risk of complication correlated to the various factors such as age, sex, fracture line type, fracture mechanism, affected side, plate length, number of holes and number of screws, shows a dispersion of these factorial variables.
Discussion
The treatment of the child’s femur fractures using screwed plate osteosynthesis has often been associated with significant morbidity, mainly related to the destructive effect on the periosteum, and to the high risk of infection compared to closed site ESIN [3]. Before the age of seven, all authors agree on the principle that the treatment for femur shaft fractures is non-surgical, unless contraindicated headinjured child or in the management of polytrauma. In those specific patients, fracture surgical fixation is needed to facilitate nursing and early mobilization which avoids decubitus complications [2]. Our cohort, with a mean age of 11 years joins that of PEYROU [4] in France which recorded a mean age of 10 years and 8 1 m o n t h s about seventeen pediatric shaft plating. However, we believe, as does KREGOR [2] in the USA, that the use of SPO is to be considered as a successful way in the treatment of polytrauma. Our sex ratio of 6.5 corroborates the data in the literature with a variation in the type of accident according to age. Before 4 years of age, home and leisure accidents are as common as traffic accidents. Between 4 and 13 years of age, road accidents predominate, and after 13 years of age, there are mainly high energy sports accidents [4,5]. In our study, road accidents (8 cases) and sports injuries (4 cases), together represent 80% of the causes of femoral fractures. Also, the frequent occurrence of femoral diaphysis fracture in boys could be explained by the greater activity of boys and their tendency to early integration into working life compared to girls who play less dangerous and who are often confined to housework in Africa.
In general, the frequent fracture site at the middle third of pediatric femur shaft is noted by most authors. This is explained by high-energy mechanism and anatomical middle bone weakness [5]. Transverse or short oblique fracture lines are the most common in this area with often constant displacement due to the high-energy impact of muscle masses [6]. Our study, like that of VITIELLO [7] in Rome, corroborates the prevalence of these types of fractures at the middle third of femur pediatric shaft.
We recorded closed site shaft fracture in all cases, with associated head-injured in two patients, forearm two bones closed site fracture in one child, an isolated right fibula fracture in one case and a left iliac wing fracture with pelvic contusion and bladder ruptured in a patient. The most frequently reported associated injury in the literature remains head trauma. MIRDAD [8] in Saudi Arabian population, noted 48.3% of head-injured, which corroborates our work. We found no hemodynamic disorder or vasculo-nervous injury. Those two complications are considered rare or exceptional in the literature [9-11]. LYNCH [64] believes that if hemodynamic instability occurs, it should require investigation for an associated injury. The indication of surgical treatment for femur shaft fractures in children has long been debated in different teams [12]. ESIN appears to be a safe and efficient option, but according to LONGIS [13] in France, it is limited to children between 6 and 13 years of age with little developed muscles. In the USA, the recommendations of the American Academy of Orthopedic Surgeons (AAOS) for Titanium Elastic Nailing are referred to isolated shaft fracture in pediatric populations at least older than 6 years and under 45Kg of weight [14, 15]. In our work the mean age was 11 years with extremes of 7 and 15 years. Technically, rigid intramedullary fixation is referred to children with bone age greater than 13 years, which corresponds to the period when consequences of iatrogenic epiphysiodesis are avoided [16]. The open SPO appears, in the literature, to have fewer and fewer indications, but plating provides anatomical reduction and excellent primary stability superior to other methods [3]. GREENE [17], emphasize that plate strength is lower than that of a rigid +intramedullary nail. Authors such as LEFEVRE [18] in Bordeaux, specify that conventional open screwed plate compression on the bone can cause periosteal stripping, extramedullary and intramedullary vascular damage. This can lead to bone rarefaction under the plate, slowing down bone healing time which exposes the child to iterative fractures. Nowadays Minimally invasive plate osteosynthesis has revolutionized fracture fixation especially in comminuted fractures [19]. Such method preserves the blood supply to the injured bone, improves the rate of fracture healing, and lowers the incidence of infection and other complications. It does not only help in retaining the soft tissue envelope around the fragments, but also prevents the loss of fracture hematoma which in turn dramatically reduces the chances of infection, delayed union or non-union [20]. Careful and meticulous reduction also goes a long way in prevention of malunion, though one should remember that LCP application with minimally invasive plate osteosynthesis is not a simple procedure, and it requires a learning curve. Adequate preoperative planning too is mandatory, as well as accurate surgical timing. This percutaneous plating appears to be the next step in the evolution of biological plating [21,22].
In our study, we performed conventional LCP plating without bone consolidation disruption, loosening, malunion or iterative fracture. We believe that our surgical non-hemorrhagic approach of Vastus Lateralis muscle disinsertion allows undamaging bone access with a good exposure of the fracture site. This contributes to the patient postoperative rapid mobilization. It is important to select the implant length according to the type of fracture. From a mechanical point of view, the plate or number of screws should be chosen to avoid implant rupture before consolidation. The ideal length of the plate is estimated using an index called “Plate Span Width” (PSW) (equal quotient: Implant Length / Fracture Line Length). According to GAUTIER [23] and STOFFEL [24], this index must be greater than 2 or 3 in a comminuted fracture and 8 or 10 in a simple fracture. MIPO advocates using long plates, with 10-16holes, to increase the work area by reducing the strain on the plate [1]. Our study records a six screwed plate in most cases (11 patients) which corresponds to an average of length between ten and twelve centimeters. The results of our study are globally overlapping the literature, coming close to those of SINK [1] in the USA about a series of 19 screwed plate osteosynthesis, and PEYROU in France [4]. Table X compares the results of different authors in literature. The main complications found in the literature are implant infection, malunion, fracture of the plate and pseudarthrosis. Most complications of open reduction and plating have been reported due to extensive surgical exposure and periosteal stripping. In addition, open reduction and plating can involve significant blood loss during application and during implant removal. Second extensive surgery is required for hardware removal [1,2,25]. Overall, open plating for pediatric shaft femur fractures has shown mixed results. GANEM [26] in Egypt, in a meta-analytic study published in 2021, compared the results of minimally invasive plating with those of ESIN for pediatric femur shaft fractures. All six series included in this work were randomized clinical trials comparing the two techniques in children aged between 5 to 15 years. He concluded that screwed plate method is more stable than nailing but fixed the indications for unstable or comminuted fractures.
We have recorded a mean time of radiological bone bridging callus formation of 60 days. Two wounds presented superficial suppuration which was healed under antibiotic therapy and procedure directing the scar. The study noted in addition a case of 1cm limb shortening in the long run, after an average follow-up of 24 months. Use of open femur shaft plating in children is not very common and a few have been reported in literature so far [26]. However, we believe that the evolution of biological fixation and new technic of percutaneous plating does hold a promise and appears to be a great step in managing pediatric femur fractures in our context. Multivariate study of complication risk in our series revealed that the following predictor factors such as age, sex, fracture-line type, fracture mechanism, affected side, plate length, number of plate holes and number of screws, are independent variables of interest not associated to the risk of complication occurrence. In addition, there was no significant correlation (p =0.0012) between fracture consolidation time and the length of the plate, on the one hand, and on the other one fracture consolidation time was highly associated with the patient’s age as radiological callus appeared to be much faster when the child is young (p = 0.973).
Conclusion
Open pediatric screwed plate osteosynthesis for femur shaft fractures appears in our context to be a successful way of treatment. The results in our study have revealed good anatomical and functional outcomes. Healing was rapid, and postoperative care was simplified specially in strong children and adolescents. Such method allows an early full motion, good mobility, and easy hygienic management in polytraumatized patients. This leads to a short stay hospitalization, a decrease of missed days of school with insignificant risk of serious complications. The authors highly recommend breakthrough percutaneous plating technic to respect the periosteum and achieve the same risk level of ESIN where nailing is not indicated (Table 1-3) (Figure 3).
Declaration Section
We, the undersigned, declare that the information given in this
study is correct according to the rules and meet these followings:
• Ethics approval and consent to participate are legally
included in the statutes of ours national teaching hospitals
• Consent for publication is approve by all the authors
• Availability of data and material is made possible by
archiving services
• There’s no competing interest
• This scientific work has no funding support
• Authors’ contributions involved medical record reviews
by Ndeye Fatou Seck, the data collection by Ibrahima Bocar
Wellé, long-range identification and tracking information by
Aloïse Sagna, Manuscript writing and syntax correction by
Aloïse Sagna and Ibrahima Fall.
Acknowledgement
None.
Conflicts of Interest
• All authors work in the same hospital named Albert Royer
National children hospital.
• We declare that there are no known conflicts of interest
associated with this publication and there has been no
significant financial support for this work that could have
influenced its outcome.
• We confirm that the manuscript has been read and
approved by all named authors and that there are no other
persons who satisfied the criteria for authorship but are not
listed.
• We further confirm that the order of authors listed in the
manuscript has been approved by all of us.
• We take full responsibility for the work being reported. It
is the original study and has been neither published elsewhere
nor submitted for publication.
References
-
<
- Sink El, Hedequist D, Morgan Sj, Hresko T (2006) Results and technique of unstable pediatric femoral fractures treated with submuscular bridge plating. J Pediatr Orthop 26(2): 177-181.
- Kregor PJ, KM Song, ML Routt, BJ Sangeorzan, RM Liddell, et al. (1993) Plate fixation of femoral shaft fractures in multiple injured children. J Bone and Joint Surg 75(12): 1774-1780.
- Ward WT, Levy J, Kaye A (1992) Compression plating for child and adolescent femur fractures. J Pediatr Orthop 12(5): 626-632.
- Peyrou P (2003) Plate osteosynthesis of femur fractures in children. Ann Orthop West 36: 217-252.
- Kamina P (1991) Anatomy: osteology of the limbs. maloine 2: 87-99.
- Clavert Jm, Metaizeau Jp (1990) Limb fractures in children. Montpellier, Sauramps medical: distribution Vigot.
- Vitiello R, Lillo M, Donati F, Masci G, Noia G, et al. (2019) Locking plate fixation in pediatric femur fracture: evaluation of the outcomes in our experience. Acta Biomed 90(1): 110-115.
- Tarek Mirdad (2000) Operative treatment of femoral shaft fractures in children: a nine-year experience in a Saudi Arabian population. Injury Int J Care Injured 31(10): 769-771.
- Clavert JM, Karger CL, Lascombes P, Ligier JN, Metaizeau JP et al. (2000) Childhood fractures (GEOP). Sauramps Medic 213-237.
- Khale W, Leonhardt H, Platzer W (1991) Locomotor device. Flammarion Med Scienc 188-190.
- Metaizeau JP (2006) Femoral shaft fractures in children. Encycl Med Chir, Musculoskeletal system 14-078 -B-10.
- Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, et al. (2010) American Academy of Orthopedic Surgeons Clinical Practice Guideline on Treatment of Pediatric Diaphyseal Femur Fracture. J Bone Jt Surg-Am Vol juil 92(8): 1790-1792
- Longis B, Bergerault F, Bocquet Jf, Hammel A, Peyrou P et al. (2003) Femur fractures in children. Ann Orthop West 36: 217-252.
- Donati F, Mazzitelli G, Lillo M, Menghi A, Conti C et al. (2017) Elastic titanium nailing in diaphyseal femoral fractures in children under six years of age. Monde J Orthop 8 (2): 156.
- Heyworth BE, Suppan CA, Kramer DE, Yen YM (2012) Management of pediatric fractures of the diaphyseal femur. Curr Rev Musculoskelet Med juin 5(2): 120-125.
- Galpin RD, Willis RB, Sabano N (1994) Intramedullary Nailing of Pediatric Femoral Fractures. J Pediatr Orthop, 14(2): 184-189.
- Greene WB (1998) Displaced fractures of the femoral shaft in children. Clin Orthop 353: 86-96.
- Lefevre Y, Plommier N (2012) Fracture of both forearm bones in children. Med thesis, Bordeaux 3027.
- Bener A, Justham D, Azhar A, Rysavy M, Hamad A et al. (2007) Femoral fractures in children related to motor vehicle injuries. J Orthop Nurs 11:146 -150.
- Ben Jann R (2008) Fracture of the femoral diaphysis in children Pediatric surgery thesis Rabat Univers Mouham V 229.
- Bergerault F, Agostini L, Le Carrou T, Bonnard C (2002) Fractures of the femoral diaphysis in children. Sauramps Medical, Montpellier 201-221.
- Blanquart D (1987) Stable elastic pinning of femur fractures in children. Medical thesis. University of Nancy.
- Gautier E, Sommer C (2003) Guidelines for the clinical application of the LCP. Injury, int J Care Injured 34: S-B63-S-B76.
- Stoffel K, Dieter U (2003) Biomechanical testing of the LCP: how can stability in locked internal fixators be controlled? Injury, int J Care Injured 34: S-B11-S-B19.
- Hedequist D, Bishop J, Hresko T (2008) Locking plate fixation for pediatric femur fractures. J Pediatr Orthop 28(1): 6-9.
- Ganem A M, Salama A M, Elhewala T A, Saleh M K (2021) Comparing outcomes of plating versus flexible nailing of femur shaft fracture in children. Europ J Molecul Clin Med 8(3): 3335-3341.
-
Aloise Sagna*, Ndeye Fatou Seck, Ibrahima Bocar Welle and Ibrahima Fall. Screwed Plate Osteosynthesis (SPO) for Pediatric Femur Fractures: A Report of 15 Cases. Glob J Ortho Res. 4(5): 2023. GJOR.MS.ID.000591.
-
Pediatric femur shaft, Fracture osteosynthesis, Screwed plate, Minimally invasive surgery, Screwed plate osteosynthesis, Elastic stable intramedullary Nailing, Association of osteosynthesis, Locking compression plate, American academy of orthopedic surgeons, Plate span width, Minimally invasive plate osteosynthesis
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






