 Case Report
Case Report
Masquelet Technique in Clavicle Fracture with Large Post-Infection Bone Defect: Case Report
Rafael Costa Mathias1, Danielle Horing Grubert2* and Luciano Campelo3
1Orthopedist and traumatologist at the Good Samaritan Charitable Association - Maringá - PR, Brazil
2Orthopedist and traumatologist at the Good Samaritan Charitable Association - Maringá - PR, Brazil
3Orthopedist and traumatologist, Full member of the SBOT and member of the SBCOC, preceptor of the Orthopedics and Traumatology Service at the Santa Rita hospital - Maringá - PR, Brazil
Corresponding AuthorDanielle Horing Grubert, Orthopedist and traumatologist at the Good Samaritan Charitable Association- Maringá, PR Brazil
Received Date:April 28, 2025; Published Date: May 06, 2025
Summary
This case study reports the treatment of a 40-year-old female patient, victim of a motorcycle accident, who presented a comminated fracture of the right clavicle complicated by postoperative infection and extensive bone loss. Initially treated with internal fixation with a rigid plate, the patient developed persistent infection and significant bone fragmentation. Therefore, the Masquelet technique was adopted in August 2022, with extended debridement and use of antibiotic-impregnated bone cement to control the infection and induce the biological membrane. After improvement of the infection, the spacer was removed and grafted with an autologous fibula.
Treatment included continuous clinical and radiographic monitoring, as well as tissue cultures, in a multidisciplinary approach involving Orthopedics, infectious diseases and physiotherapy. The Masquelet technique proved to be effective both in local control of the infection and in the regeneration of the bone defect, highlighting its relevance in complex fractures with infectious involvement. The case reinforces the need for adaptive therapeutic planning and rigorous monitoring for the success of the treatment.
Abstract
This case report describes the treatment of a 40-year-old female patient, victim of a motorcycle accident, who presented a comminated fracture of the right clavicle complicated by postoperative infection and extensive bone loss. Initially treated with internal fixation with a rigid plate, the patient developed persistent infection and significant bone fragmentation. Therefore, the Masquelet technique was adopted in August 2022, with extended debridement and use of antibiotic-impregnated bone cement to control the infection and induce the biological membrane. After improvement of the infection, the spacer was removed and grafted with an autologous fibula. Treatment included continuous clinical and radiographic monitoring, in addition to tissue cultures, in a multidisciplinary management involving Orthopedics, infectiology, and physiotherapy. The Masquelet technique proved to be effective both in local control of the infection and in regeneration of the bone defect, evidencing its relevance in complex fractures with infectious involvement. The case reinforces the need for adaptive therapeutic planning and rigorous monitoring for treatment success.
Keywords:Bones of the upper extremity; osteomyelitis; masquelet technique; bone graft
Introduction
Clavicle fractures are frequently seen in trauma, especially in motor vehicle accidents. Although conventional treatments have a high success rate, complications such as postoperative infections and bone defects still represent significant challenges in the management of these fractures [1]. In this context, the Masquelet technique has emerged as an effective alternative in the treatment of complex bone defects, particularly in cases of bone loss associated with severe infections [2]. The technique involves crucial steps, such as extensive debridement of devitalized tissue and the use of bone cement impregnated with antibiotics, which, in addition to controlling the infection, promote bone regeneration aiming at the formation of a membrane which will later receive a graft [3,4]. This case study aims to evaluate the application of this technique in a patient with significant bone defect, highlighting the clinical outcomes and the challenges faced throughout the treatment.
Methodology and Case Report
A 40-year-old female patient was the victim of a motorcycle accident who developed a closed comminated fracture of the right clavicle, postoperative infection, and pseudarthrosis, and subsequently underwent autologous grafting. The study was approved by the institution’s Ethics Committee and followed all ethical standards to ensure patient safety and confidentiality. Clinical data were collected retrospectively from the electronic medical record, including signs and symptoms, medical procedures adopted, radiographs, images of surgical interventions, antibiotic therapies, and clinical response over time. Clinical follow-up occurred between May 2022 and December 2024, with outpatient care, imaging tests, multiple surgical procedures, and continuous assessment of clinical evolution.
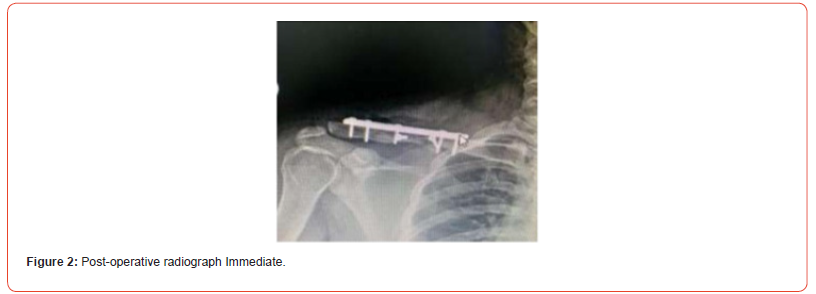
The patient initially underwent internal fixation with a rigid plate in May 2022, immediately after the accident (Figures 1 & 2). In the immediate postoperative period, she developed dehiscence of the surgical wound and signs of infection. In June 2022, the first surgical debridement was performed with removal of the synthesis material. The persistence of the infectious condition and the large bone fragmentation observed on the radiographs led to a new intervention in August 2022, with extended debridement and application of the Masquelet technique, using bone cement impregnated with vancomycin to fill the defect and induce the biological membrane. The spacer was stabilized with an intramedullary Kirschener wire to prevent its displacement (Figures 3 & 4). The patient used oral antibiotic therapy during the treatment period.



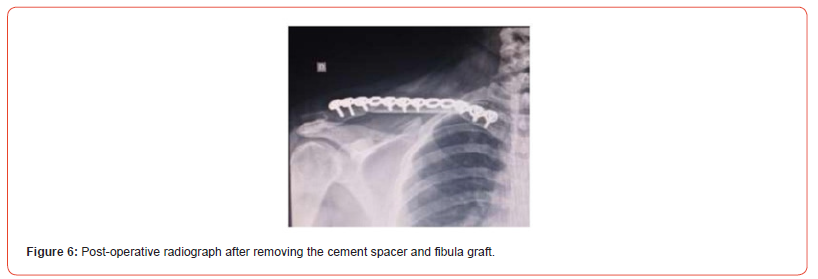
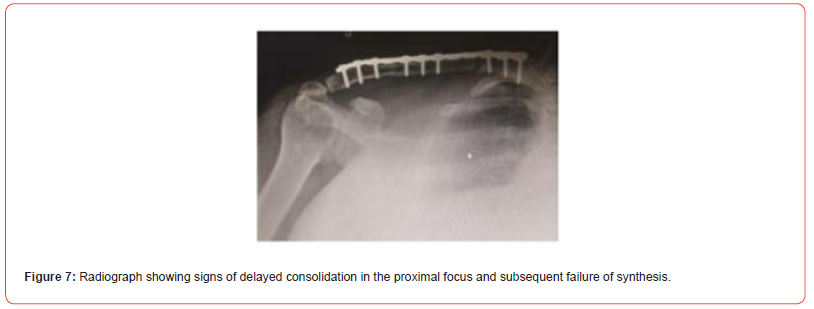
After a few months, with signs of improvement in the infectious process, in April 2023, the induced membrane was opened, the spacer was removed, and a bone graft with an autologous fibula of approximately 6 cm was performed to fill the gap (Figures 5 & 6). During follow-up, the patient presented a delay in consolidation of the proximal focus of the graft, which generated instability and subsequent breakage of the synthesis material at the site (Figure 7), thus requiring a new surgical approach in September 2023. On this occasion, the synthesis was removed, osteotomy of the proximal edge was performed to resection fibrosis at the focus, and the fracture was stabilized with a new rigid plate (Figures 8 & 9). Clinical follow-up was continuous, with serial radiographs, tissue cultures, and therapeutic adjustments according to the evolution of the clinical response. Management was carried out in a multidisciplinary manner, involving orthopaedists, infectious disease specialists and physiotherapists. In his last evaluation, 19 months after the initial post-operative period, the radiographs demonstrated good consolidation in the fracture site and the patient presented good functional recovery of the right upper limb (Figure 10).




Discussion
The approach of this clinical case highlights the challenges faced in the treatment of complex clavicle fractures, particularly those associated with extensive bone loss and postoperative infection. There is little data in the literature on the use of the Masquelet technique specifically in the clavicle; however, studies in the upper limb demonstrate that it is an effective alternative for both infection control and bone regeneration in highly complex clinical scenarios [1,5]. associated with adequate functional recovery [5-7]. The initial phase of the technique, based on the induction of a biological membrane through the implantation of bone cement impregnated with antibiotics, allowed local control of the infection and the creation of a microenvironment conducive to osteogenesis and the future receipt of an autologous graft aimed at filling the extensive bone defect [3].
The use of this autologous fibular bone substitute in the second stage of the procedure was decisive for the success of the reconstruction. This type of graft offers rigid support, osteogenic properties and low local immunogenicity, favouring integration at the local site. [2,4] Despite the occurrence of delayed bone consolidation, subsequent revision of the synthesis material and local removal of fibrosis to stimulate osteogenesis were fundamental for the outcome. clinical. Another important factor was to provide rigidity to the fracture site using a stiffer long plate in this reapproach.
Final Considerations
This study reinforces the effectiveness of the Masquelet technique in the treatment of complex bone defects, especially in clavicle fractures associated with postoperative infection. By promoting an environment favourable to bone regeneration and controlling local infection, the technique has proven to be a safe and efficient alternative. The experience reported also highlights the importance of rigorous monitoring to optimize results. Thus, the Masquelet technique reaffirms itself as a valuable tool in the therapeutic arsenal for complicated fractures, whose application should be carefully monitored, and its use expanded through new research.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Devkota P, Acharya BM, Pradhan NMS, Shrestha SK, Thakur AK, et al. (2021) Minimally-Invasive Plate Osteosynthesis for Clavicle Fractures. Rev Bras Ortop (Sao Paulo) 57(2): 295-300.
- Quesada A, Videla Ávila F, Horué Pontoriero G, Filisetti JE. (2023) Transport over the clavus respecting Masquelet's membrane in severe segmental defects. Series of cases.Rev Asoc Argent Ortop 88(1): 79-90.
- Guimarães JAM, Scorza BJB, Machado JAP, Cavalcanti ADS, Duarte MEL (2023) Characterization of the Masquelet Induced Membrane Technique in a Murine Segmental Bone Defect Model. Rev Bras Ortop (Sao Paulo) 58(5): e798-e807.
- Quiroz Williams J, Gaytán Fernández S, Barragán Hervella RG, Morgan Padrón S, Rojas Durán O, et al. (2023) Clinical experience on the management of post- traumatic bone defects of long bones treated with the membrane induction technique. Minutes Ortop Mex 37(5): 264-269.
- Bourgeois M, Loisel F, Bertrand D, Nallet J, Gindraux F, et al. (2020) Management of forearm bone loss with induced membrane technique. Hand Surg and Rehabil 39(3): 171–177.
- Braswell MJ, Bulloch LR, Gaston RG, Garcia RM (2023) Outcomes After Use of the Induced Membrane Technique for Fractures of the Upper Extremity. The Journal of Hand Surgery 48(7): 735.e1–7.
- Ma XY, Liu B, Yu HL, Zhang X, Xiang LB, et al. (2022) Induced Membrane Technique for the Treatment of Infected Forearm Nonunion: A Retrospective Study. J Hand Surg Am 47(6): 583.e1-583.e9.
-
Rafael Costa Mathias, Danielle Horing Grubert* and Luciano Campelo, Kimiya Shirbacheh. Masquelet Technique in Clavicle Fracture with Large Post-Infection Bone Defect: Case Report. Glob J Ortho Res. 5(1): 2025. GJOR.MS.ID.000601.
-
Bones of the Upper Extremity, Osteomyelitis, Masquelet technique, Bone Graft
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






