 Review Article
Review Article
External Fixation in Tibial Pilon Fractures
Horacio Tabares Sáez1* and Horacio Tabares Neyra2
1Transilvania University of Brasov, Medicine PhD School, Cuba
2Universidad Médica de La Habana, Cuba
Corresponding AuthorHoracio Tabares Sáez, Transilvania University of Brasov, Medicine PhD School, Cuba
Received Date:June 04, 2025; Published Date:June 30, 2025
Abstract
Introduction: Tibial pilon fractures, caused by high-energy trauma, are accompanied by severe damage to the vulnerable soft tissue envelope and joint damage, which favors the occurrence of complications. Nowadays, external fixators are not only used as a temporary fixation device, but also as a definitive treatment method.
Purpose: To present an approach to the use of external fixation methods in the treatment of tibial pilon fractures.
Search strategy: Search in PubMed, Google Scholar and Elsevier, of publications between the years 2013-2025 in English with the terms:
“external fixation in tibial pylon fractures”, “fractures of the distal end of the tibia treated with external fixation” and “external fixation in metaphysoarticular fractures of the distal tibia”.
Development: The high number of complications prompted the search for new treatment methods. External fixation began to be used as a
definitive treatment, especially in distal tibial fractures caused by traumas where high energy was released and therefore great comminution
occurred, also accompanied by extensive damage to the surrounding soft tissues, open Gustilo fractures types II and III, wounds with great
contamination or the presence of important comorbidities of the patient; situations where internal reduction and osteosynthesis is associated with
a high rate of failure and complications.
Conclusions: Tibial pilon fractures are rare, but present an immense challenge for orthopedic surgeons. External fixation is useful in more
complex cases, where internal fixation shows high rates of complications and poor results.
Keywords:External fixation; complex fractures; ligamentotaxia
Introduction
Tibial pilon fractures are serious injuries resulting from predominantly axial impaction. They are often accompanied by severe damage to the vulnerable soft tissue envelope and joint damage, making them prone to complications [1]. Tibial pilon fractures are quite rare, accounting for 3% to 10% of all tibia fractures and less than 1% of all lower extremity fractures. Men tend to suffer these injuries slightly more often than women, with most injuries occurring around age 45. In 75-90% of cases, the fibula is also fractured [2]. These are high-energy lesions that occur in young patients, and the typical mechanism involves axial compression combined with shear forces. The classic pattern of fragments that develops after the impact of the talus on the distal tibia, and the location and extent of the articular comminution, are determined by the position of the foot; they should be understood as a wide range of osteoarticular, metaphyseal and soft tissue injuries; therefore, the management of this fracture remains a challenge and a complex task for clinicians [3]. Unfortunately, the prognosis for this injury is not encouraging, and often results in lifealtering disability and reduced quality of life [4]. The unacceptably high complication rate in the 1990s prompted the search for new definitive treatment methods [5].
From there, external fixators were not only used as a temporary fixation device, but also as a definitive treatment method. Especially in highly comminuted distal tibia fractures with maximum soft tissue damage, open Gustilo type III fractures, highly contaminated wounds, or significant patient comorbidities, where open reduction and internal fixation is associated with a high risk of failure and complications [6,7] Therefore, external fixators may present a satisfactory alternative form of definitive treatment [8,9]. The purpose of this paper is to show an approach to the use of external fixation methods in the treatment of tibial pilon fractures.
Search Strategy and Selection Criteria
References were identified by searching PubMed, Google Scholar and Elsevier for publications between 2013-2025 in English with the terms: «external fixation in tibial pylon fractures», «fractures of the distal end of the tibia treated with external fixation» and «external fixation in metaphyso-articular fractures of the distal tibia». Articles accessible freely or through the Clinical key and Hinari services were also reviewed.
Development
External Fixation
External fixation can be used as a temporary measure for the staging of tibial pilon fractures, as well as for definitive fixation. It is based on the principle of capsuloligamentotaxia, with the intention of indirectly reducing the fracture by stressing the soft tissues surrounding the ankle bones.
Time Fixation
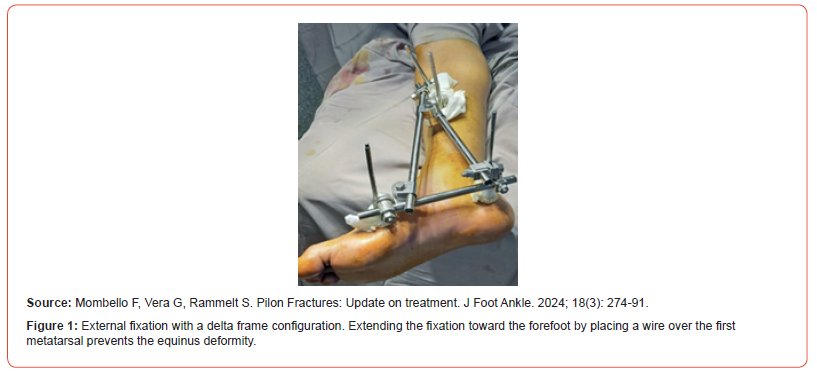
As most tibial pilon fractures are strongly comminuted due to the high-energy trauma mechanism, the initial treatment consists of an external fixation encompassing the ankle in terms of damage control surgery [10-12]. Temporary fixation should be performed as quickly as possible to achieve realignment and restore length and anatomical reduction. When used temporarily for staging, it is important to carefully place the pins outside the area of injury and the planned surgical site so as not to interfere with the definitive fixation and cross future surgical approaches, which also reduces the risk of infection, since higher rates of infection have been reported when the definitive internal fixation extended to the area of the provisional external fixator pins [13]. There are multiple different external fixator systems, and most of them form a «Delta» shape above the ankle (Figure 1). An extension of the external fixator at the front of the foot, most commonly to the first metatarsal, is advisable to prevent contracture of the equine. This safe reduction and thus minimal movement of bone fragments relative to each other provides an ideal environment for soft tissues to recover [14].
Definitive External Fixation
The high number of complications that occurred, caused by the difficulties in its treatment, prompted the search for new definitive treatment methods. External fixation began to be used not only as a temporary fixation device, but also as a definitive treatment, especially in distal tibial fractures caused by traumas where high energy was released and therefore great comminution occurred, also accompanied by extensive damage to the surrounding soft tissues, open Gustilo fractures types II and III, wounds with great contamination or presence of important comorbidities of the patient; situations where internal reduction and osteosynthesis is associated with a high rate of failure and complications. Today, external fixation methods for definitive primary treatment are indicated primarily in tibial pilon fractures, where the risk of serious complications due to poor soft wrapping, grade II or III open fractures, and severe patient comorbidities is too great [15]. For all of the above, external fixators may present a satisfactory alternative form of definitive treatment.
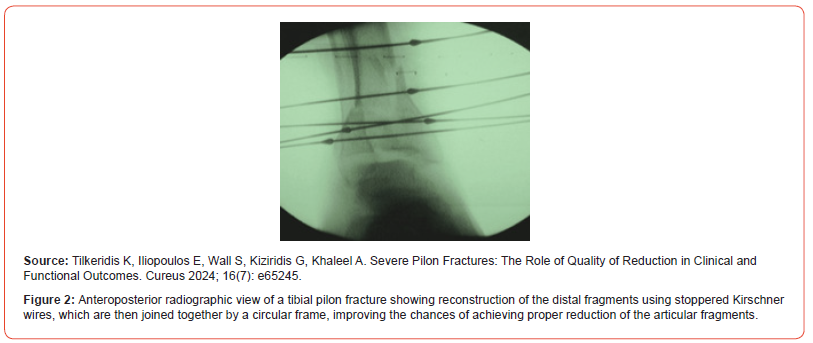
Several different external fixation techniques are described in the literature. These include simple bridge frames that extend or reserve the ankle, circular frames or hybrid frames. In general, a basic distinction can be made between ankle fixation and ankle extension systems. Ankle preservation systems are beneficial for functional outcome, as movement in the ankle joint is not restricted. If the external attachment method is sufficiently stable, it is possible to support the weight load; That’s especially true in hybrid systems [16]. Hybrid fixator systems consist of at least three tensioned Kirschner wires, which are placed in the distal fragments of the fracture site and connected through a circular frame (Figure 2). Mostly, hybrid external fixation systems can be used in the ankle sparring technique, and after a while, it is possible to support the entire weight [17]. Circular frame fixators have been used as a definitive fixation for high-energy pylon fractures where bone or soft tissue injury prevented internal fixation. Thin wire frame fasteners and hybrid fasteners with high consolidation rates have been described [18]. While there are also high rates of nail-tract infections, deep infections and osteomyelitis are rare. (Figure 3) Since the joint surface is usually very comminuted and lacks soft tissue insertions, capsuloligamentotaxis cannot reliably reduce joint fragments, especially in cases of central impaction or depression. Limited internal fixation has been used, in addition to the frame structures, to improve the quality of the reduction. In addition, no differences in functional outcomes have been found between articulated external fixators that allow early mobility of the ankle and those that immobilize it for an extended period. A meta-analysis comparing this method with open reduction and internal fixation found no difference in infection or complication rates between the two groups [19].
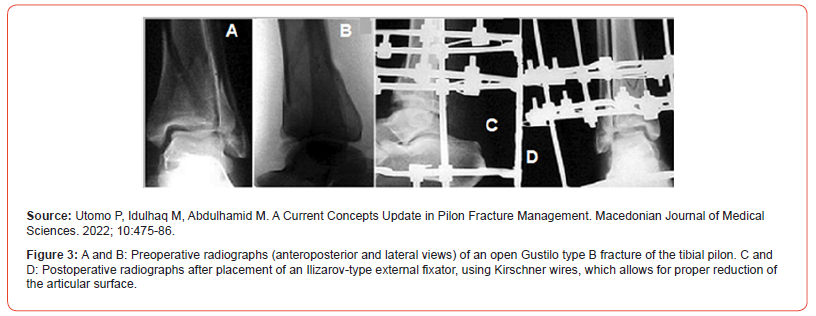
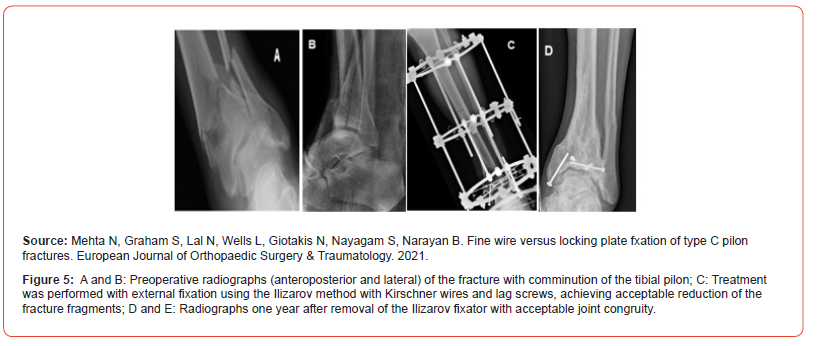
The introduction of the Ilizarov external fixation method has presented new possibilities. Their use of tensioned transfixiating wires offers the possibility of securely fixing small bone segments and thus building a tight bone construct while allowing axial micromovement, which, as is known, promotes bone healing. In addition, its circular configuration often implies that the ankle joint does not need to be pierced and therefore early movement is possible that improves blood flow to the injured cartilage. When there is significant bone loss, the Ilizarov fixation system can provide a tool for distraction osteogenesis [20]. An external tibiocalcaneal fixator has been used to reduce skin complications (Figure 4). The nonunion rate is 2% to 15% in studies reporting treatment with an external fixator that joins the ankle, 0% to 16% for hybrid periarticular external fixator, and 3% to 25% for the Ilizarov external fixation method [21]. External fixation methods can also be combined with limited internal osteosynthesis or minimally invasive techniques, e.g., percutaneous Kirschner wire or lag screws, to better reduce joint surfaces (Figure 5). The most common complication associated with the use of external fixators in general is infection of the wire tract, which can also lead to major deep infections, namely septic arthritis and osteomyelitis.

Papadokostakis compared the external ankle fixation systems and found no significant differences in infection rate, lack of union, and time to union in tibial pilon fractures, but ankle ligamentotaxia systems had a significantly higher incidence of malunion. In addition, in systems where ankle stress is applied, the functional outcome was also significantly lower compared to ankle preservation systems [22]. When a hybrid external fixator is used for permanent fixation, stable bone fixation is provided without damaging soft tissues and the joint is free. Papadokostakis’ review of the literature revealed that the rate of pseudoarthrosis was not higher for techniques that leave the ankle free with a hybrid external fixator (5% of 230 fractures) compared to techniques in which the external fixator bridges the ankle (7% of 131 fractures) [23]. These good results with a hybrid external fixator are confirmed in the study by Galante, [24] who reported a rate of delayed healing or pseudoarthrosis of 4% in 162 patients with a healing time of 125 days; the study by Scaglione,16 reported a pseudoarthrosis rate of 5% in 75 patients with a consolidation time of 120 days; and the Babis study,6 showed a pseudoarthrosis rate of 10% in 48 patients. Ristiniemi [25] reported on the use of an external Ilizarov fixator in 47 patients with a binding rate of 74% and a time to union of 133 days, while Leung [26] reviewed 31 patients who had a binding rate of 97% and a time to union of 97 days.
Multiple other studies have compared the outcomes of internal osteosynthesis and external fixation. The result appears to be similar in terms of early complications, but a significantly higher rate of superficial infection was observed, mainly due to wire tract infections. However, the rate of deep infections did not vary significantly between the two methods. The rate of malunion was significantly higher in external fixation than in internal osteosynthesis, which is probably due to the limited possibility of anatomical reduction of external fixation. In addition, the functional outcome seems to be worse in external fixation than in internal osteosynthesis, which was also attested in the lower possibility of anatomical reconstruction of the articular surface. However, studies have shown that both thin wire external fixation and internal osteosynthesis offer an equivalent functional outcome in highly comminuted and severely displaced pylon fractures [27- 29]. From a radiological point of view, the quality of the reduction appears to reduce the rate of osteoarthritis in the long term. Silluzio demonstrated that the use of external fixation was effective, especially in complex fractures, with an 86% good reduction.
Conclusion
Tibial pilon fractures are rare, but present an immense challenge for orthopedic surgeons; They are complex injuries, difficult to treat even for the most expert trauma surgeons. The combination of articular cartilage injury, metaphyseal comminution, and soft tissue damage has often resulted in historically unfavorable outcomes. Tibial pilon fractures are usually caused by high-impact trauma, concomitant injuries are common, and while open reduction and internal fixation remain the mainstay of treatment for most of these fractures, additional treatment modalities are emerging, such as external fixation, that should be considered for more complex cases. The use of external fixation methods as a definitive treatment, alone or in combination with osteosynthesis using Kirschner wires or lag screws to achieve better reduction of joint fragments, constitutes a valid and useful therapy for complex tibial pilon fractures with high comminution.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Hill DS, Davis JR (2023) What is a tibial pilon fracture and how should they be acutely managed? A survey of consultant British Orthopaedic Foot and Ankle Society members and non-members. Ann R Coll Surg Engl.
- Rodriguez Castells F (2020) Fracturas del pilón tibial. Rev Asoc Arg Ortop y Traumatol 61(3): 312-321.
- Murawski CD, Mittwede PN, Wawrose RA, Belayneh R, Tarkin IS (2023) Management of high-energy tibial Pilon fractures. J Bone Joint Surg Am 105(14): 1123-1137.
- Lineham B, Faraj A, Hammet F (2024) Outcomes of Acute Ankle Distraction for Intra-Articular Distal Tibial and Pilon Fractures. Orthop Procs 106-B(Supp5): 11-11.
- (1996) Orthopaedic Trauma Association Committee for coding and classification. Fractures and dislocation compendium. J Orthop Trauma 10(Suppl 1): 57-58.
- Babis GC, Kontovazenitis P, Evangelopoulos DS, Tsailas P, Nikolopoulos K, et al. (2010) Distal tibial fractures treated with hybrid external fixation. Injury 41(3): 253-258.
- Richards JE, Magill M, Tressler MA, Shuler FD, Kregor PJ, et al. (2012) External fixation versus ORIF for distal intra-articular tibia fractures. Randomized Controlled Trial 35(6): 862-867.
- Taylor BC, So E, Karim A (2020) Spanning External Fixation for Pilon Fractures: Steering Wheel and Kickstands. Orthopedics 43(3): e187-e190.
- Flett L, Adamson J, Barron E, Brealey S, Corbacho B, et al. (2021) A multicentre, randomized, parallel group, superiority study to compare the clinical efectiveness and cost-efectiveness of external frame versus internal locking plate for complete articular pilon fracture fxation in adults. Protocol for the active randomized controlled trial. Bone Jt Open 2(3): 150-163.
- Das M, Pandey S, Gupta H, Bidary S, Das A (2023) Clinical characteristics and outcome of tibial pilon fractures treated with open reduction and plating in a tertiary medical college. Journal of Gandaki Medical College 16(2).
- Luo TD, Pilson H (2022) Pilon Fracture. PubMed. Treasure Island (FL), StatPearls Publishing.
- Mair O, Pflüger P, Hoffeld K, Braun KF, Kirchhoff Ch, et al. (2021) Management of Pilon Fractures. Current Concepts. Front. Surg 8: 764232.
- Daniels NF, Lim JA, Thahir A, Krkovic M (2021) Open pilon fracture postoperative outcomes with definitive surgical management options: a systematic review and meta-analysis. Arch Bone Joint Surg 9: 272-282.
- Mombello F, Vera G, Rammelt S (2024) Pilon Fractures: Update on treatment. J Foot Ankle 18(3): 274-291.
- Swords MP, Weatherford B (2020) High-Energy Pilon Fractures: Role of External Fixation in Acute and Definitive Treatment. What are the Indications and Technique for Primary Ankle Arthrodesis? Foot Ankle Clin 25(4): 523-536.
- Scaglione M, Celli F, Casella F, Fabbri L (2019) Tibial pilon fractures treated with hybrid external fixator: analysis of 75 cases. Musculoskelet Surg 103: 83-89.
- Tilkeridis K, Iliopoulos E, Wall S, Kiziridis G, Khaleel A (2024) Severe Pilon Fractures: The Role of Quality of Reduction in Clinical and Functional Outcomes. Cureus 16(7): e65245.
- Utomo P, Idulhaq M, Abdulhamid M (2022) A Current Concepts Update in Pilon Fracture Management. Macedonian Journal of Medical Sciences 10: 475-486.
- Meng YC, Zhou XH (2016) External fixation versus open reduction and internal fixation for tibial pilon fractures: A meta-analysis based on observational studies. Chin J Traumatol 19(5): 278-282.
- Álvarez López A, García Lorenzo YC (2016) Fijación externa en pacientes con fracturas del pilón tibial. Rev Arch Med Camagüey 20(3): 338-344.
- Mehta N, Graham S, Lal N, Wells L, Giotakis N, et al. (2021) Fine wire versus locking plate fxation of type C pilon fractures. European Journal of Orthopaedic Surgery & Traumatology 32: 875–882.
- Papadokostakis G, Kontakis G, Giannoudis P, Hadjipavlou A (2008) External fixation devices in the treatment of fractures of the tibial plafond: a systematic review of the literature. J Bone Joint Surg Br 90: 1-6.
- Galante VN, Vicenti G, Corina G, Mori C, Abate A, et al. (2016) Hybrid external fixation in the treatment of tibial pilon fractures: a retrospective analysis of 162 fractures. Injury 47: S131-S137.
- Ristiniemi J, Flinkkilä T, Hyvönen P, Martti L, Harri P, et al. (2007) Two-ring hybrid external fixation of distal tibial fractures: a review of 47 cases. J Trauma 62(1): 174-183.
- Leung F, Kwok HY, Pun TS, Chow SP (2004) Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury 35(3): 278-283.
- Meena UK, Bansal MC, Behera P, Upadhyay R, Gothwal GC (2017) Evaluation of functional outcome of pilon fractures managed with limited internal fixation and external fixation: a prospective clinical study. J Clin Orthop Trauma 8: S16-20.
- Ramlee MH, Kadir MRA, Murali MR, Kamarul T (2014) Finite element analysis of three commonly used external fixation devices for treating Type III pilon fractures. Med Eng Phys 36(10): 1322-1330.
- Abd-Almageed E, Marwan Y, Esmaeel A, Mallur A (2015) Hybrid external fixation for Arbeitsgemeinschaft für Osteosynthesefragen (AO) 43-C tibial plafond fractures. J Foot Ankle Surg 54(6): 1031-1036.
- Wang C, Li Y, Huang L, Wang M (2010) Comparison of two-staged ORIF and limited internal fixation with external fixator for closed tibial plafond fractures. Arch Orthop Trauma Surg 130(10): 1289-1297.
-
Horacio Tabares Sáez* and Horacio Tabares Neyra.External Fixation in Tibial Pilon Fractures. Glob J Ortho Res. 5(1): 2025. GJOR.MS.ID.000604.
-
External fixation; complex fractures; ligamentotaxia
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






